Unveiling the Journey: How Ozempic Transforms Appetite and Weight Loss
Embarking on a weight loss journey with Ozempic (semaglutide) offers a groundbreaking opportunity to manage appetite and reduce cravings through a sophisticated hormonal mechanism. This GLP-1 receptor agonist mimics natural gut hormones to promote satiety and regulate blood sugar, helping users shift their relationship with food. Yet, understanding the nuances of cravings and learning effective strategies to overcome them can markedly enhance outcomes beyond medication alone.
Strategic Craving Management: Techniques That Complement Ozempic’s Effects
While Ozempic reduces hunger signals, users often encounter psychological or habitual cravings that medication alone cannot extinguish. Integrating mindful eating practices—such as slowing down meals, savoring flavors, and recognizing true hunger cues—provides a critical behavioral layer. Additionally, choosing nutrient-dense, high-fiber foods can prolong fullness, stabilizing blood sugar and mitigating impulsive snacking urges.
Regular hydration also plays an underrated role, as thirst signals can masquerade as hunger, triggering unnecessary eating. Strategic meal timing aligned with Ozempic’s dosing schedule can further optimize appetite suppression, as some studies suggest timing injections to precede main meals maximizes satiety benefits.
Empowering Lifestyle Adjustments: Exercise and Sleep as Allies
Physical activity not only accelerates caloric expenditure but also modulates appetite hormones like ghrelin and leptin, harmonizing hunger cues. Consistent moderate exercise routines enhance metabolic flexibility and reduce emotional eating triggers. Meanwhile, prioritizing quality sleep is indispensable; insufficient rest disrupts hormonal balance, amplifying cravings and diminishing the efficacy of appetite control medications.
How Can Ozempic Users Effectively Balance Medication with Behavior to Beat Persistent Cravings?
Successfully managing cravings requires a multifaceted approach. Users should work closely with healthcare providers to tailor injection timing, dosage, and dietary plans, ensuring an individualized strategy that respects personal triggers and lifestyle factors. Cognitive-behavioral techniques, such as identifying craving patterns and employing distraction or substitution strategies, empower users to reclaim control. Exploring resources like doctor-approved appetite management tips can provide valuable structured guidance.
Moreover, acknowledging the psychological components of cravings is essential. Emotional support, whether through counseling or support groups, complements pharmacological effects and reinforces sustainable change.
Expert Insight: The Science Behind Semaglutide’s Appetite Suppression
Semaglutide’s efficacy derives from its action on GLP-1 receptors in the brain’s hypothalamus, a critical appetite regulation center. This interaction slows gastric emptying and enhances satiety signals, reducing caloric intake. A 2021 study published in The New England Journal of Medicine demonstrated significant weight loss outcomes with semaglutide, underscoring the importance of combining medication with lifestyle modifications for optimal results.
Understanding this mechanism empowers users to align their behavioral strategies with their medication’s physiological effects, fostering a synergistic approach.
Join the Conversation: Share Your Ozempic Craving Control Success
Your experience matters. If you’ve discovered effective ways to manage cravings alongside Ozempic, share your story or insights to help others navigate their weight loss path. Engaging with a supportive community enriches motivation and knowledge exchange.
Reflecting on Real-Life Challenges and Triumphs with Ozempic
Starting my journey with Ozempic, I quickly realized that while the medication significantly curbed my hunger, it wasn’t a magic wand that erased all cravings. The mental tug of habitual snacking or emotional eating still surfaced, especially during stressful days or social gatherings. This prompted me to dig deeper into how I could harmonize Ozempic’s effects with conscious lifestyle choices. For instance, I began journaling my meals and moods, which helped me identify specific triggers that prompted cravings despite reduced physical hunger.
One surprising insight was how hydration influenced my appetite. On days I neglected water intake, I noticed a spike in perceived hunger, which was often just thirst in disguise. Keeping a water bottle handy became a simple yet powerful habit that complemented my treatment.
Crafting a Personalized Routine: Timing and Nutritional Synergy
Through trial and error, I found that timing my weekly injections strategically before my largest meal helped maximize my satiety throughout the day. Aligning meal composition with Ozempic’s action was equally key; meals rich in fiber and lean proteins kept me fuller longer and smoothened out blood sugar fluctuations that might otherwise trigger cravings.
Incorporating regular, enjoyable physical activities like brisk walking and yoga also shifted my relationship with hunger. Exercise not only helped regulate appetite hormones but also boosted my mood and energy, reducing emotional eating episodes.
What Are Some Unexpected Lifestyle Tweaks That Can Amplify Ozempic’s Appetite Control?
Beyond the obvious dietary and exercise habits, I discovered that quality sleep played a pivotal role. Poor sleep often sabotaged my hunger hormones, making me more vulnerable to cravings despite medication. Prioritizing consistent sleep schedules and winding down without screens improved my overall appetite regulation.
Additionally, practicing mindfulness meditation helped me become more aware of my body’s true hunger signals versus emotional impulses. This awareness made it easier to make intentional food choices and resist temptations.
Expert Advice Enhances Personal Experience
Integrating insights from medical experts can further empower your journey. The American Diabetes Association highlights the importance of combining pharmacotherapy like semaglutide with behavioral interventions to achieve sustainable weight loss (source). Their guidance reinforced my commitment to a holistic approach rather than relying solely on medication.
For those navigating this path, exploring resources such as weekly injection weight loss guides can offer structured strategies to optimize your regimen effectively.
Opening the Floor: Your Experiences with Balancing Ozempic and Lifestyle
Have you found unique ways to merge Ozempic with daily habits that helped you conquer stubborn cravings? Perhaps you’ve discovered an unexpected ally or faced challenges worth sharing. I invite you to join the conversation and share your story. Together, we can foster a supportive community that learns and grows from each other’s journeys.
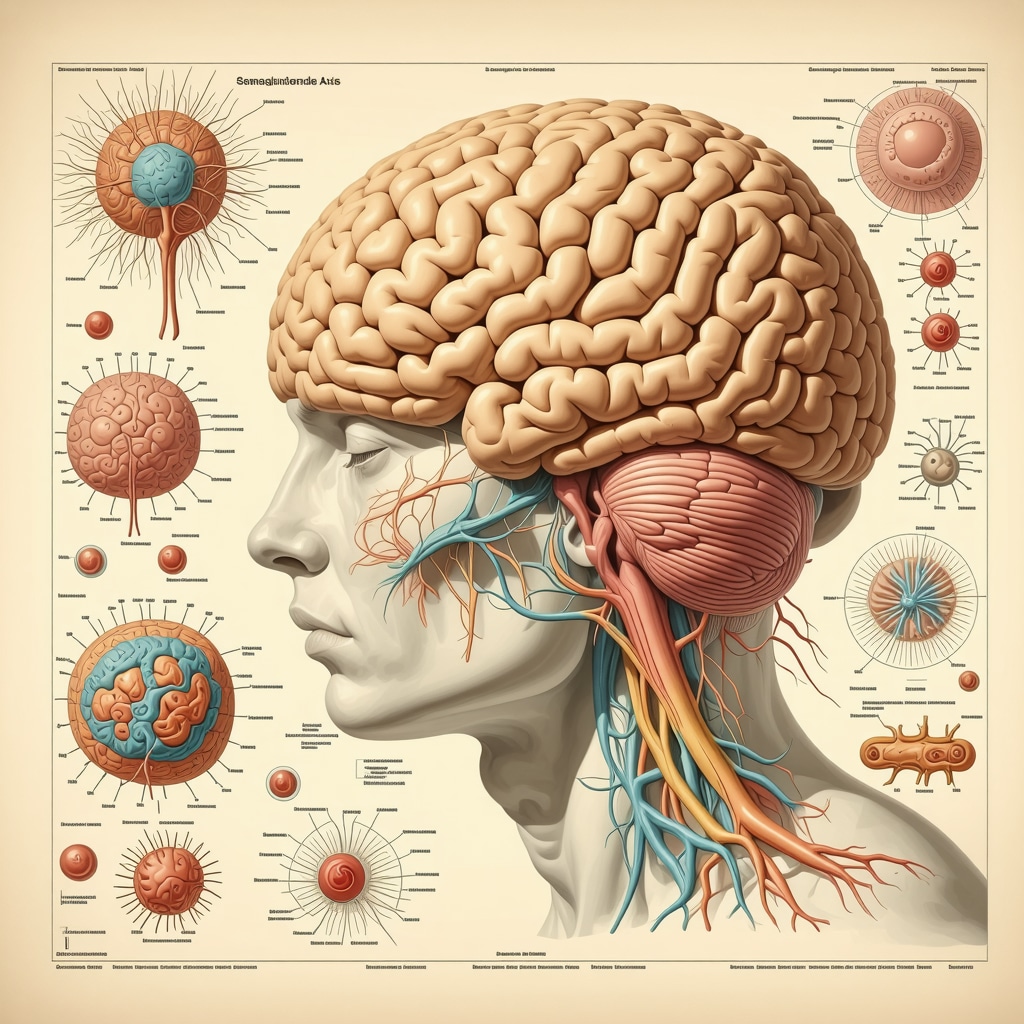
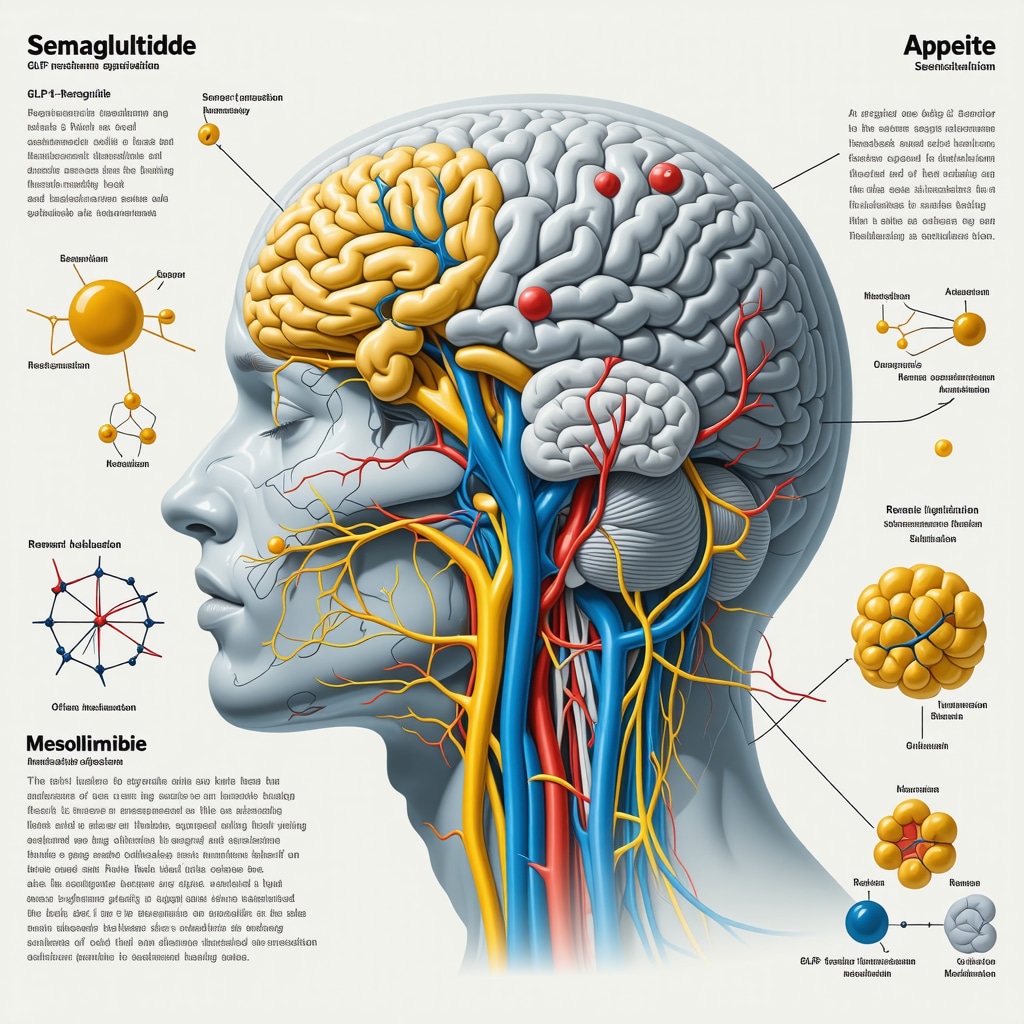
Unlocking Neural Pathways: How Semaglutide Modulates Central Appetite Networks
While semaglutide’s peripheral effects on gastric emptying and insulin secretion are well-documented, its central nervous system actions reveal a more intricate narrative. Recent neuroimaging studies demonstrate that semaglutide crosses the blood-brain barrier to engage GLP-1 receptors within the arcuate nucleus of the hypothalamus, a hub for integrating hunger and satiety signals. This engagement modulates neuronal populations—namely, the pro-opiomelanocortin (POMC) and agouti-related peptide (AgRP) neurons—thereby recalibrating the balance between anorexigenic and orexigenic signaling pathways. Such modulation not only decreases the physiological drive to eat but also attenuates reward-based food seeking behavior often triggered by high-calorie palatable foods.
Can Semaglutide’s Central Appetite Effects Influence Emotional Eating Patterns?
Emotional eating, often driven by limbic system activation and dopaminergic reward circuits, presents a formidable challenge in weight management. Evidence suggests that semaglutide’s action extends beyond hypothalamic centers to influence mesolimbic pathways, dampening the hedonic response to food stimuli. This dual modulation offers a promising avenue for individuals struggling with cravings rooted in emotional or stress-related contexts. However, it is crucial to complement pharmacotherapy with cognitive behavioral therapy (CBT) or mindfulness-based interventions to address the psychological components effectively.
Precision Nutritional Timing: Synchronizing Meal Patterns with Ozempic Pharmacodynamics
Understanding semaglutide’s pharmacokinetic profile—characterized by a prolonged half-life facilitating once-weekly dosing—enables tailored meal timing strategies that optimize appetite suppression. For instance, scheduling the weekly injection approximately 24 hours before the largest caloric intake can potentiate satiety signals during peak consumption periods. Moreover, integrating low-glycemic index (GI) foods during this window can stabilize postprandial glucose excursions, further mitigating hunger spikes.
Emerging research underscores the benefits of chrono-nutrition principles; aligning nutrient intake with circadian rhythms may enhance metabolic flexibility and hormonal harmony. This synchronization can amplify the medication’s effect by reinforcing endogenous regulatory mechanisms, thus reducing reliance on willpower alone.
Leveraging Gut Microbiota Modulation to Support Ozempic-Induced Weight Loss
Recent advances in gut microbiome research reveal its pivotal role in appetite regulation and energy homeostasis. Semaglutide’s influence on gastrointestinal motility and secretion may indirectly shift microbial composition, favoring species associated with improved metabolic profiles. Strategic incorporation of prebiotic and probiotic-rich foods—such as fermented vegetables, inulin-containing plants, and kefir—can synergistically enhance this effect, promoting short-chain fatty acid production that impacts gut-brain signaling pathways.
Integrating microbiota-targeted nutrition not only supports weight loss but also fortifies gut barrier integrity and systemic inflammation control, which are often compromised in obesity.
Expert Recommendations: Integrating Multimodal Approaches for Sustainable Appetite Control
According to a 2023 review in Nature Reviews Endocrinology, combining GLP-1 receptor agonists with behavioral, nutritional, and microbiome-focused interventions offers the most robust outcomes for weight management. This multimodal framework acknowledges the complex biopsychosocial dimensions of appetite and craving, encouraging personalized medicine approaches tailored to individual neurobiology and lifestyle contexts.
Healthcare providers should assess patients holistically, incorporating neuropsychological screening, dietary counseling, and physical activity planning to maximize semaglutide’s benefits while mitigating potential challenges such as residual cravings or emotional eating.
Next Steps: Deepen Your Expertise and Optimize Your Ozempic Journey
If you are navigating appetite control with Ozempic, consider engaging with specialized resources that delve into neurobehavioral strategies and precision nutrition principles. Subscribing to expert-led webinars, consulting with endocrinologists familiar with pharmacodynamics, and participating in structured support groups can elevate your understanding and empower sustained success.
We invite you to explore our advanced guides and connect with a community committed to evidence-based approaches by visiting expert Ozempic strategies. Your journey towards refined appetite mastery is a step away from transformation.
Decoding Neurochemical Synergies: Enhancing Ozempic’s Central Appetite Modulation
Delving deeper into semaglutide’s neurochemical impact reveals its ability to recalibrate reward-based eating circuits, a pivotal factor in tackling persistent cravings that arise from hedonic rather than homeostatic hunger. By engaging GLP-1 receptors in mesolimbic pathways, Ozempic attenuates dopaminergic signaling associated with the pleasurable anticipation of high-calorie foods, thus disrupting the cycle of emotional or stress-induced eating. This neurobiological insight underscores the necessity of integrating pharmacotherapy with psychotherapeutic modalities, such as cognitive-behavioral therapy (CBT) or mindfulness practices, to systematically dismantle maladaptive eating behaviors.
How Can Targeted Behavioral Therapies Complement Ozempic’s Neural Appetite Regulation?
Targeted behavioral therapies, including CBT and acceptance and commitment therapy (ACT), can amplify Ozempic’s efficacy by addressing the cognitive distortions and emotional triggers that perpetuate craving cycles. These interventions promote awareness of internal states and foster adaptive coping mechanisms, thereby reinforcing the drug’s modulation of central appetite circuits. For practitioners, tailoring these therapies alongside pharmacological regimens maximizes long-term weight management success.
Chronobiology Meets Pharmacotherapy: Optimizing Meal Timing and Nutrient Composition
Integrating chronobiological principles with Ozempic’s pharmacodynamics can substantially optimize appetite control. Aligning meal timing with circadian rhythms—favoring larger caloric intake during daylight hours and tapering off in the evening—coupled with the administration of semaglutide approximately 24 hours prior to the main meal, synchronizes endogenous satiety signaling pathways. Emphasizing low-glycemic and fiber-rich foods during this window stabilizes blood glucose and insulin responses, mitigating rebound hunger and enhancing satiety duration.
Microbiome Modulation: Harnessing Gut Flora to Support Appetite Suppression
Emerging evidence positions gut microbiota as a critical mediator in appetite and weight regulation. Semaglutide’s gastrointestinal effects may promote shifts in microbial populations toward species that enhance short-chain fatty acid production, which in turn modulates gut-brain communication pathways governing hunger and satiety. Strategic dietary inclusion of prebiotics and probiotics—such as inulin, resistant starches, and fermented foods—can potentiate these microbiome-driven benefits, fostering systemic metabolic improvements and reinforcing appetite control.
Integrative Clinical Frameworks for Sustainable Weight Loss
According to a 2023 comprehensive review in Nature Reviews Endocrinology, a multimodal approach combining GLP-1 receptor agonists with personalized nutritional counseling, behavioral therapy, and microbiome-targeted interventions yields superior outcomes in obesity management. This paradigm emphasizes the heterogeneity of appetite regulation mechanisms and the necessity for individualized treatment protocols. Clinicians are encouraged to adopt holistic assessment tools encompassing neuropsychological profiling and metabolic phenotyping to customize therapeutic strategies.
Empower Your Journey: Engage with Expert Resources and Community Insights
To deepen your understanding and optimize your experience with Ozempic, consider engaging with specialized webinars led by endocrinologists and behavioral scientists who elucidate the nuances of neurobehavioral and chrono-nutritional strategies. Additionally, participation in structured support groups offers invaluable peer insights and accountability mechanisms. Explore our curated advanced resources and join a thriving community dedicated to evidence-based appetite mastery at expert Ozempic strategies. Elevate your weight management journey through informed, precision-guided interventions.
Frequently Asked Questions (FAQ)
What is Ozempic and how does it help with weight loss?
Ozempic is a brand name for semaglutide, a GLP-1 receptor agonist originally developed for type 2 diabetes management. It promotes weight loss primarily by suppressing appetite through action on brain receptors that regulate hunger and satiety, slowing gastric emptying, and reducing cravings, thereby decreasing caloric intake.
Why do some cravings persist even when taking Ozempic?
Despite Ozempic’s physiological appetite suppression, psychological and habitual factors such as emotional eating, stress, and conditioned behaviors can sustain cravings. These cravings are often mediated by brain reward circuits less influenced by medication, necessitating complementary behavioral interventions for optimal control.
How can meal timing be optimized to enhance Ozempic’s effectiveness?
Timing the weekly Ozempic injection approximately 24 hours before the largest meal can maximize satiety during peak caloric intake. Additionally, aligning meals with circadian rhythms—favoring larger daytime meals and lighter evenings—and consuming low-glycemic, fiber-rich foods help stabilize blood glucose and prolong fullness.
What lifestyle habits best complement Ozempic treatment?
Regular moderate exercise modulates appetite hormones and reduces emotional eating triggers, while quality sleep maintains hormonal balance critical for appetite regulation. Hydration and mindful eating practices are also essential to discern true hunger from thirst or emotional impulses, enhancing medication benefits.
Can Ozempic help reduce emotional or stress-related eating?
Semaglutide’s central action on mesolimbic reward pathways can dampen hedonic food cravings linked to emotional eating. However, integrating cognitive-behavioral therapy or mindfulness-based approaches is crucial to address the psychological components fully and achieve durable behavior change.
How does the gut microbiome influence appetite control with Ozempic?
Ozempic’s effects on gastrointestinal motility and secretions may beneficially alter gut microbiota composition, promoting species that produce short-chain fatty acids involved in gut-brain signaling. Consuming prebiotic and probiotic-rich foods can further support these microbiome-mediated appetite regulation pathways.
Is it safe to use Ozempic long-term for weight management?
Current evidence supports the safety and efficacy of long-term semaglutide use under medical supervision for obesity management, but ongoing clinical monitoring is essential. Treatment should be part of a comprehensive plan including lifestyle modifications to sustain benefits and minimize risks.
What role do behavioral therapies play alongside Ozempic?
Behavioral therapies such as cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT) address cognitive distortions and emotional triggers of cravings. These strategies synergize with Ozempic’s neurochemical appetite modulation to improve adherence and long-term weight management outcomes.
How can one monitor progress and adjust treatment effectively?
Regular consultations with healthcare providers to assess weight trends, appetite patterns, side effects, and psychological factors are important. Adjusting dosage, injection timing, or incorporating additional interventions based on individual response optimizes therapeutic success.
Where can I find expert resources and support for managing appetite with Ozempic?
Specialized webinars, support groups, and evidence-based online guides provided by endocrinologists and behavioral scientists offer valuable education and community engagement. Engaging with these resources enhances understanding and sustainability of weight loss efforts.
Trusted External Sources
- The New England Journal of Medicine (NEJM): This peer-reviewed journal offers pivotal clinical trial data on semaglutide’s efficacy and safety profiles, underpinning evidence-based use in weight management (NEJM Semaglutide Trial).
- Nature Reviews Endocrinology: Provides comprehensive reviews on endocrinology and metabolism, including emerging multimodal approaches combining pharmacotherapy with lifestyle and microbiome interventions for obesity (Nature Reviews 2023).
- American Diabetes Association (ADA): Offers authoritative guidelines on GLP-1 receptor agonists for diabetes and weight management, emphasizing integrated behavioral strategies (ADA Weight Loss Medications).
- Endocrine Society: Provides clinical practice guidelines and expert consensus on obesity pharmacotherapy and personalized treatment protocols.
- Journal of Clinical Endocrinology & Metabolism (JCEM): Publishes research on neuroendocrine mechanisms of appetite regulation and pharmacological interventions.
Conclusion
Ozempic (semaglutide) represents a transformative advancement in appetite control and weight management by engaging central and peripheral mechanisms to reduce hunger and cravings. However, its optimal impact emerges when combined with personalized lifestyle adaptations—including strategic meal timing, mindful eating, physical activity, quality sleep, and behavioral therapies—that address the complex biopsychosocial facets of appetite regulation. Additionally, leveraging gut microbiome modulation and chronobiological principles can further enhance therapeutic outcomes. Sustained success with Ozempic requires a holistic, evidence-based approach informed by expert guidance and continuous self-awareness. We encourage readers to apply these integrative strategies, share their experiences, and explore advanced resources to elevate their weight loss journey with confidence and precision.


I really appreciate how this article highlights that while Ozempic helps with the physiological side of appetite control, managing the psychological and habitual cravings is just as crucial. In my own journey using Ozempic, I’ve noticed that the medication reduces my hunger quite effectively, but emotional eating during stressful times still sneaks in. What’s helped me is combining the medication with mindfulness meditation and journaling my food intake coupled with my moods. This has made me more aware of my triggers and helped prevent those automatic snack urges.
Also, the emphasis on hydration resonated with me; I used to mistake thirst for hunger and found that increasing my water intake lowered unnecessary snacking. I’m curious about others’ experiences—have any readers found specific behavioral strategies or apps that helped track and manage cravings while on Ozempic? I feel like sharing practical tools could really support those of us looking to integrate both pharmacological and behavioral approaches for sustained success.
Melissa, I really resonate with your mention of journaling and mindfulness in managing cravings alongside Ozempic. In my own experience, pairing the medication with a structured behavioral approach dramatically shifted my relationship with food. One strategy that worked well for me was the use of habit-tracking apps combined with scheduled prompts for mindful eating breaks during the day. These reminders encouraged me to slow down and truly assess whether I was experiencing hunger or a craving driven by emotional triggers.
Additionally, I found that incorporating light physical activity, like short walks after meals, not only helped regulate my appetite hormones but also acted as a positive distraction during craving moments. It’s fascinating how exercise complements semaglutide’s hormonal effects by balancing ghrelin and leptin levels.
I also appreciate the post’s emphasis on timing injections before the largest meal and aligning dietary choices with the medication’s pharmacodynamics. This gave me insight into why some meals felt more satisfying than others.
Curious to hear if others have experimented with combining behavior-focused apps or methods along with Ozempic to personalize craving management. What tools or routines have made the biggest difference in your journey?
Reading this post reminded me of how important holistic approaches are when starting with Ozempic. I’ve noticed that while the medication significantly decreases my physical hunger, emotional and habitual cravings still pop up, especially in stressful situations or social settings. Developing a mindful eating routine has really helped me become more aware of my true hunger cues versus emotional triggers. I’ve also started incorporating weekly meal prep with fiber-rich foods, which keeps me full longer and stabilizes blood sugar, making cravings less frequent.
One thing I’ve found beneficial is tracking my moods and cravings in a journal, which has helped me identify patterns and times when I’m most vulnerable. Does anyone have recommendations for apps or additional strategies that support mindfulness and craving management alongside medication? I believe combining behavioral tools with pharmacotherapy can really make a difference in sustaining weight loss efforts. Would love to hear others’ experiences or suggestions.
This article really hits home for me, especially the part about combining medication with behavioral strategies. I’ve been on Ozempic for a few months now, and while it’s helped curb my physical hunger, I still struggle with emotional eating, particularly during stressful workdays. I found that journaling my moods and cravings has been a game-changer—I can identify patterns and develop coping mechanisms. Incorporating mindful eating techniques, like savoring each bite and eating slowly, also helped me recognize genuine hunger versus emotional urges.
An interesting point you raised was about hydration—on days I forget to drink enough water, I tend to feel hungrier than I actually am, which leads to unnecessary snacking. I’ve started using an app that logs my water intake and meals; it’s great for staying accountable.
For others in a similar boat, what types of behavioral tools or apps have you found effective in managing cravings alongside Ozempic? I’m keen to hear practical solutions that can complement the medication for sustained weight loss.