Harnessing Ozempic’s Power: The Art of Managing Hunger Cravings
For many using Ozempic (semaglutide) as part of their weight loss journey, taming hunger cravings remains one of the most pivotal challenges. While Ozempic’s GLP-1 receptor agonist mechanism naturally suppresses appetite and helps regulate blood sugar, understanding how to complement this pharmacological effect with strategic lifestyle choices can significantly enhance outcomes. This article delves into expert-backed, nuanced strategies to manage hunger effectively, making your weight loss experience not only sustainable but empowering.
Strategic Nutritional Choices That Amplify Appetite Control
One of the most tangible ways to manage hunger while on Ozempic is through diet composition. Prioritizing high-fiber, protein-rich foods can extend satiety and reduce the intensity of cravings. Foods such as legumes, lean meats, nuts, and vegetables slow gastric emptying and stabilize blood sugar, aligning synergistically with Ozempic’s effects. Additionally, incorporating healthy fats like those in avocados and olive oil supports hormone balance and prolonged fullness.
Consider the timing and frequency of meals: smaller, nutrient-dense meals spaced evenly throughout the day can prevent the blood sugar dips that often trigger ravenous hunger. Experimentation with mindful eating—focusing on texture, flavor, and chewing pace—enhances the brain-gut connection, reinforcing natural satiety signals.
How Can Ozempic Users Effectively Navigate Emotional Hunger and Cravings?
Emotional hunger can undermine even the most well-planned weight loss strategies. For Ozempic users, recognizing the difference between physiological hunger and emotional triggers is essential. Techniques such as journaling to identify craving patterns, practicing stress-reduction methods like deep breathing or meditation, and engaging in alternative activities (e.g., walking, hobbies) can reduce non-hunger eating episodes. Cognitive-behavioral strategies also empower users to reframe negative thought patterns regarding food and body image.
Optimizing Hydration and Sleep to Support Appetite Regulation
Hydration plays a surprisingly critical role in managing hunger. Sometimes, thirst masquerades as hunger, prompting unnecessary snacking. Drinking water consistently throughout the day, and especially before meals, can reduce caloric intake and improve satiety signals. Meanwhile, quality sleep profoundly affects appetite hormones ghrelin and leptin, which modulate hunger and fullness. Ozempic users benefit greatly from maintaining consistent sleep schedules, creating a restful environment, and addressing sleep disorders promptly.
Physical Activity: The Unsung Ally in Appetite Management for Ozempic Users
Regular exercise not only burns calories but also modulates hunger hormones and improves mood, making it a powerful tool against cravings. Moderate-intensity activities like walking, cycling, or swimming can help regulate appetite and reduce stress-induced eating. Moreover, strength training preserves lean muscle mass during weight loss, enhancing metabolic rate and supporting long-term success.
Integrating movement into daily routines—even brief bouts of activity—supports both physical and psychological aspects of appetite control, complementing Ozempic’s pharmacodynamics.
Expert Insights: The Importance of Medical Guidance in Enhancing Ozempic’s Benefits
While lifestyle strategies are vital, collaborating closely with healthcare providers ensures dosing and injection timing optimize appetite suppression while minimizing side effects. For authoritative guidance on safely maximizing Ozempic’s impact, consider reviewing weight loss tips for Ozempic users on maximizing your injection benefits. Medical professionals can tailor treatment plans, monitor progress, and offer support to navigate challenges effectively.
For more comprehensive approaches that combine diet, exercise, and medication, explore doctor-backed weight loss combining injections with lifestyle, which highlights synergistic strategies proven to enhance fat loss and appetite control.
Understanding the science behind Ozempic’s appetite regulation and integrating behavioral adaptations bridges the gap between medication and mindful living. If you found these insights valuable, share your experiences or questions in the comments below to join a community committed to informed, sustainable weight loss.
For further authoritative reading on GLP-1 medications and their role in weight management, the National Center for Biotechnology Information (NCBI) offers an in-depth review detailing semaglutide’s mechanisms and clinical outcomes.
Listening to Your Body: The Subtle Art of Hunger Awareness
When I first started using Ozempic, I thought the medication alone would handle my hunger effortlessly. But soon, I realized that tuning into my body’s subtle signals made all the difference. Instead of reacting to every craving, I began to pause and ask myself if I was truly hungry or if it was a habitual or emotional urge. This practice transformed my relationship with food and empowered me to make choices aligned with my health goals.
One helpful technique I adopted was the “Hunger Scale,” a method that encourages assessing hunger levels from 1 to 10 before eating. Eating when moderately hungry, rather than starving or just out of boredom, fosters better portion control and satisfaction. Over time, this mindful approach complemented the appetite-suppressing effects of Ozempic, making it easier to maintain a calorie deficit without feeling deprived.
Have You Ever Noticed How Your Environment Influences Your Cravings?
It’s fascinating how surroundings can trigger hunger or cravings even when we’re not physiologically hungry. For me, walking past the bakery or seeing a coworker eat snacks often sparked sudden desires. Recognizing these environmental cues helped me prepare and strategize. Simple habits like keeping healthy snacks on hand or choosing different routes to avoid tempting spots made a big difference.
Research from the Mayo Clinic highlights that environmental factors, including sight, smell, and social settings, significantly impact appetite and food choices. Being aware of these influences allows for better control and intentional eating, especially when combined with medications like Ozempic that modulate hunger signals.
Balancing Meal Composition With Injection Timing: A Personal Insight
Another layer I explored was how the timing of meals in relation to my Ozempic injections affected appetite and energy. I noticed that eating a nutrient-dense breakfast about 30 minutes after my weekly injection helped me kickstart the day with sustained energy and less hunger pangs later on. Conversely, skipping or delaying meals sometimes led to stronger cravings and fatigue.
Through trial, error, and consultation with my healthcare provider, I found a rhythm that worked for me—consistent meal timing, balanced macros, and hydration synchronized with my injection schedule. You can find more detailed advice on this topic by exploring prescription injection weight loss tips on injection timing for maximum effect.
Incorporating Mindful Movement: Beyond Just Exercise
While structured workouts are beneficial, I also discovered the value of incorporating mindful movement throughout the day. Gentle yoga stretches, short walks during breaks, or even standing while working helped me stay connected to my body and reduce stress-induced cravings. These small practices complemented my formal exercise routine and enhanced overall well-being.
This integrative approach aligns with findings from experts who emphasize that movement, stress management, and medication together create a robust framework for appetite control and weight management.
If you have experiences or tips about balancing Ozempic with lifestyle changes, I’d love to hear about them! Share your story or questions in the comments below, and let’s support each other on this journey. Also, for those interested, check out weekly injection weight loss guide tips to stay consistent for ongoing motivation and strategies.
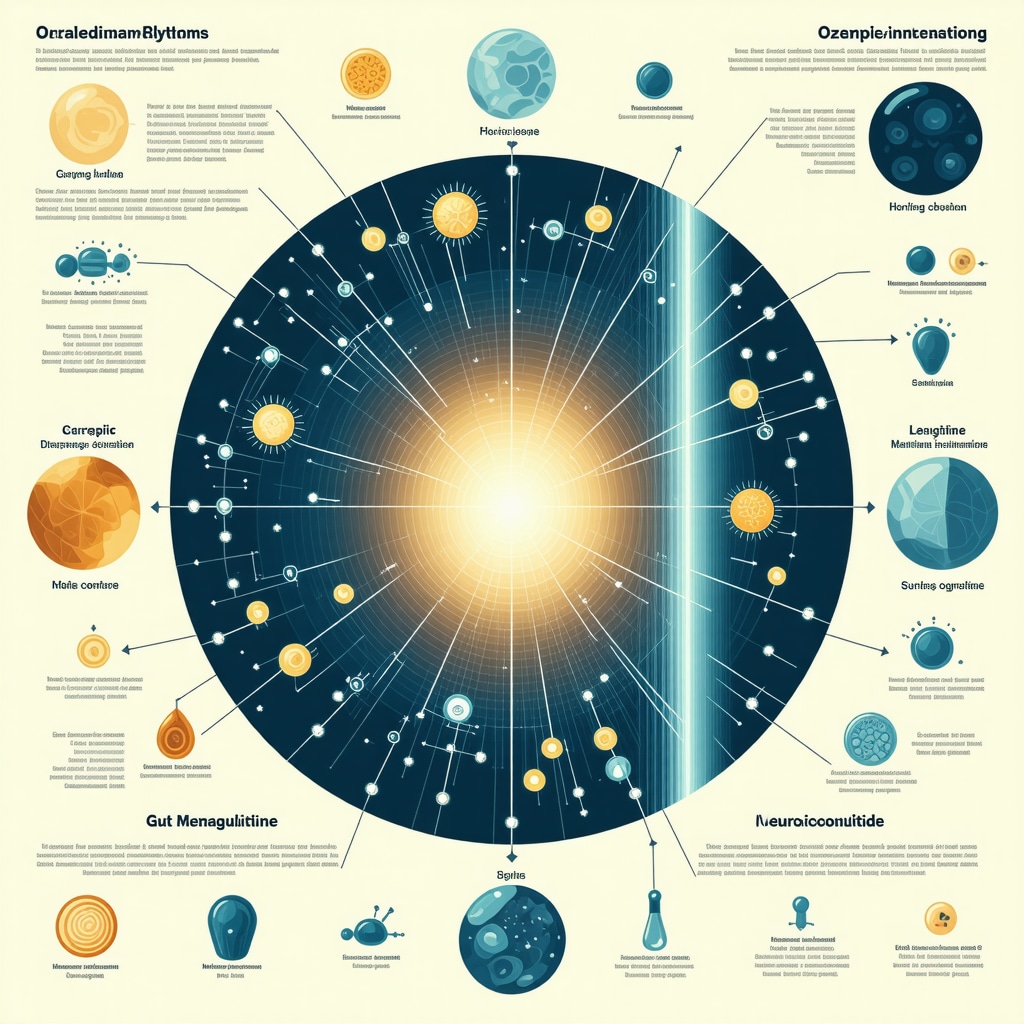
Synchronizing Ozempic Injection Timing with Circadian Rhythms for Enhanced Appetite Control
Emerging research suggests that aligning Ozempic injections with the body’s natural circadian rhythms may potentiate its appetite-suppressing effects. The endogenous secretion of GLP-1 and related metabolic hormones exhibits diurnal variation, typically peaking postprandially and modulating energy homeostasis. Administering semaglutide injections at times that coincide with these physiological fluctuations can optimize receptor sensitivity and downstream signaling pathways.
For example, some patients report improved satiety and reduced cravings when dosing occurs in the morning, potentially due to synchronization with daytime metabolic activity and feeding patterns. Conversely, evening injections may benefit others by attenuating nocturnal hunger and preventing late-night snacking. Personalizing injection timing requires careful monitoring of hunger patterns, energy levels, and glycemic responses in consultation with healthcare providers.
How Does Ozempic Influence Hormonal Crosstalk Beyond GLP-1 to Modulate Appetite?
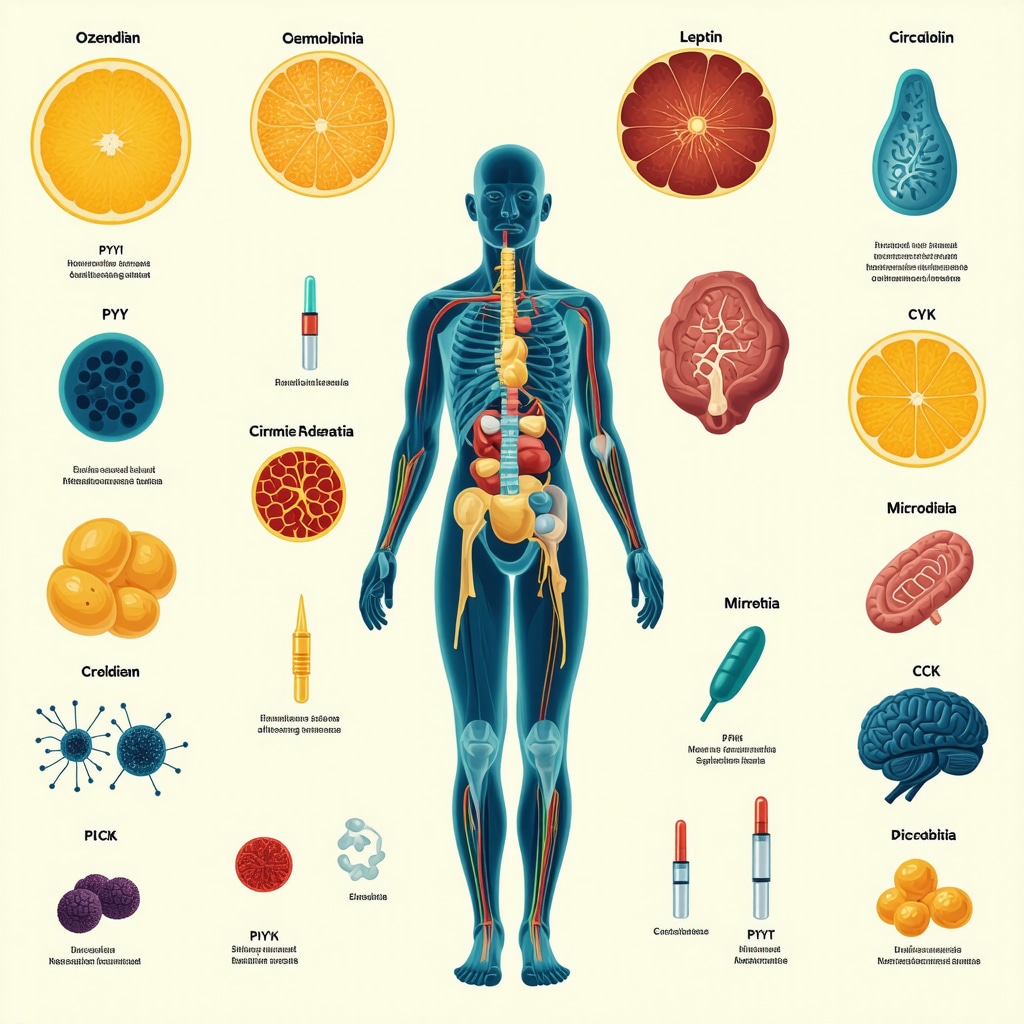
Ozempic’s action extends beyond GLP-1 receptor agonism; it intricately affects the interplay between multiple appetite-regulating hormones. Semaglutide reduces ghrelin, known as the “hunger hormone,” while simultaneously enhancing leptin sensitivity, which promotes satiety. Additionally, it modulates peptide YY (PYY) and cholecystokinin (CCK), gut-derived peptides that contribute to meal termination signals.
This multifaceted hormonal modulation contributes to both reduced caloric intake and improved glycemic control. The integration of these hormonal pathways underscores the complexity of appetite regulation and highlights why a pharmacological agent like Ozempic can be highly effective when combined with behavioral strategies.
Leveraging Behavioral Economics and Neurocognitive Techniques to Combat Cravings
Beyond physiological mechanisms, cognitive and environmental factors significantly influence eating behavior. Applying principles from behavioral economics, such as “nudging,” can help reframe food choices and reduce impulsivity. Techniques like pre-commitment, where individuals plan meals and snacks ahead of time, reduce decision fatigue and the likelihood of succumbing to cravings.
Neurocognitive interventions, including cognitive bias modification and mindfulness-based cognitive therapy, have demonstrated efficacy in attenuating hedonic eating triggers. These approaches retrain neural reward pathways, diminishing the salience of palatable food cues and enhancing self-regulation.
Integrating these advanced psychological strategies with Ozempic’s pharmacodynamics creates a synergistic framework for sustainable appetite control.
Unpacking the Role of Gut Microbiota in Modulating Ozempic’s Efficacy on Hunger
Recent studies illuminate the influence of gut microbiota composition on the therapeutic response to GLP-1 receptor agonists like semaglutide. The microbiome mediates nutrient absorption, bile acid metabolism, and short-chain fatty acid production, all of which interact with host appetite regulation.
Alterations in microbial diversity and function may impact drug metabolism and receptor expression, thereby modulating efficacy. Probiotic and prebiotic interventions aimed at fostering a favorable microbiota profile could enhance Ozempic’s appetite-suppressing effects, although clinical data remain preliminary.
Future personalized medicine approaches may incorporate microbiome assessment to tailor treatment plans for optimal weight loss outcomes.
Decoding the Complex Interplay Between Ozempic and Stress-Related Eating Behaviors
Stress-induced hyperphagia represents a formidable barrier to weight loss, often mediated by hypothalamic-pituitary-adrenal (HPA) axis activation and elevated cortisol levels. Ozempic’s modulation of central appetite circuits may partially counteract these effects, but integrating stress management techniques remains crucial.
Mindfulness meditation, biofeedback, and adaptive coping mechanisms can mitigate stress responses that trigger emotional eating. Understanding the neuroendocrine pathways involved enables a more comprehensive approach, combining pharmacotherapy with psychological resilience-building to sustain appetite regulation.
For readers interested in the neurobiological underpinnings of these mechanisms, the NCBI article on neuroendocrine regulation of appetite and stress provides a detailed exploration.
By embracing these multifactorial strategies, Ozempic users can transcend simplistic hunger management and engage in a deeply informed, holistic journey toward lasting weight loss.
Chronobiology Meets Pharmacotherapy: Timing Ozempic for Peak Appetite Suppression
Emerging insights from chronobiology underscore the significance of synchronizing Ozempic administration with endogenous circadian rhythms to potentiate its anorexigenic effects. The GLP-1 hormone secretion naturally fluctuates throughout the day, influencing metabolic processes and hunger cues. By aligning semaglutide dosing with these physiological peaks, patients may experience enhanced satiety and reduced caloric intake.
Clinical observations reveal that morning injections often correspond with improved daytime appetite regulation, while evening dosing might attenuate nocturnal cravings, a common stumbling block in weight management. This bespoke approach demands meticulous self-monitoring and collaboration with healthcare providers to tailor injection schedules that harmonize with individual metabolic and lifestyle patterns.
How Can Understanding Ozempic’s Hormonal Crosstalk Refine Personalized Weight Loss Protocols?
Ozempic’s pharmacodynamics extend beyond GLP-1 receptor agonism, intricately modulating a network of appetite-regulating hormones including ghrelin, leptin, peptide YY (PYY), and cholecystokinin (CCK). Its capacity to suppress ghrelin diminishes hunger signals, while enhancing leptin sensitivity promotes satiety. Concurrently, modulation of PYY and CCK further signals meal termination, orchestrating a comprehensive hormonal milieu conducive to reduced food intake.
Harnessing this complexity, clinicians can refine treatment plans by integrating hormonal assessments and behavioral strategies, optimizing patient-specific weight loss trajectories. This multifactorial modulation exemplifies why Ozempic, combined with lifestyle interventions, yields superior and sustainable results.
Behavioral Economics and Neurocognitive Strategies: Elevating Craving Management Beyond Pharmacology
The intersection of behavioral economics and neurocognitive therapies offers potent adjuncts to Ozempic’s physiological effects. Utilizing “nudging” principles, such as pre-commitment to specific meal plans, reduces impulsive eating by minimizing decision fatigue. Cognitive bias modification and mindfulness-based cognitive therapy retrain reward pathways, attenuating hedonic responses to palatable food cues.
When incorporated alongside semaglutide therapy, these interventions foster enhanced self-regulation and resilience against environmental and emotional triggers, addressing the psychological underpinnings of overeating that pharmacotherapy alone cannot fully resolve.
Microbiome Modulation: A Frontier for Enhancing Semaglutide’s Therapeutic Efficacy
Cutting-edge research reveals the gut microbiota’s pivotal role in modulating semaglutide’s efficacy on appetite and metabolism. Variations in microbial diversity influence nutrient absorption, bile acid metabolism, and production of short-chain fatty acids, all integral to host energy balance and drug response.
Preliminary clinical studies suggest that targeted probiotic and prebiotic supplementation may optimize gut flora composition, potentially amplifying Ozempic’s appetite-suppressing effects. While this avenue remains experimental, it heralds a personalized medicine paradigm where microbiome profiling could inform individualized therapy enhancements.
Deciphering the Neuroendocrine Nexus: Stress Mitigation as a Pillar of Weight Loss Success
Stress-induced hyperphagia, driven by HPA axis activation and cortisol elevation, can undermine Ozempic’s appetite control benefits. Integrating stress reduction modalities such as mindfulness meditation, biofeedback, and adaptive coping mechanisms complements pharmacotherapy by addressing neuroendocrine drivers of emotional eating.
Understanding these complex interactions enables a holistic approach, combining biochemical and psychological resilience-building strategies that sustain long-term appetite regulation and weight management.
For a comprehensive exploration of neuroendocrine influences on appetite amidst stress, consult the authoritative NCBI article on neuroendocrine regulation of appetite and stress.
Engage with Cutting-Edge Insights to Transform Your Ozempic Journey
Delving into the sophisticated interplay of circadian biology, hormonal networks, cognitive behavioral strategies, and microbiome science unveils a multifaceted framework for maximizing Ozempic’s efficacy. By embracing these advanced concepts and collaborating closely with healthcare professionals, you can elevate your weight loss regimen beyond conventional paradigms.
We invite you to share your experiences, questions, or insights in the comments below and join a community dedicated to evidence-based, progressive approaches to appetite regulation and sustainable weight management.
Frequently Asked Questions (FAQ)
How does Ozempic specifically suppress appetite?
Ozempic (semaglutide) acts as a GLP-1 receptor agonist, mimicking the incretin hormone GLP-1. It slows gastric emptying, enhances satiety signals in the brain, reduces ghrelin (the hunger hormone), and improves leptin sensitivity, collectively leading to decreased appetite and reduced caloric intake.
Can adjusting the timing of Ozempic injections improve weight loss results?
Yes. Aligning Ozempic injections with your body’s circadian rhythms can enhance its appetite-suppressing effects. Morning injections may better control daytime hunger, while evening dosing can reduce nocturnal cravings. Personalization with medical guidance is key to optimize timing based on individual hunger patterns and lifestyle.
What lifestyle modifications complement Ozempic to manage hunger effectively?
Integrating a high-protein, high-fiber diet, consistent hydration, quality sleep, and regular physical activity synergizes with Ozempic’s pharmacology. Behavioral approaches like mindful eating, stress management, and cognitive strategies also play critical roles in sustaining appetite control and preventing emotional or environmental triggers.
How does stress impact hunger and how can Ozempic users mitigate this?
Stress elevates cortisol, which can trigger emotional eating and increase appetite. While Ozempic modulates appetite pathways, incorporating stress reduction techniques such as mindfulness meditation, biofeedback, and adaptive coping mechanisms is essential to counteract stress-induced hyperphagia effectively.
What role does the gut microbiome play in Ozempic’s effectiveness?
The gut microbiota influences nutrient metabolism, drug response, and appetite regulation. Variations in microbial composition can affect semaglutide’s efficacy. Emerging research suggests probiotic and prebiotic interventions might enhance drug response, though clinical evidence is still developing.
Is it necessary to distinguish between physiological hunger and emotional cravings when on Ozempic?
Absolutely. Ozempic primarily targets physiological hunger signals. Recognizing emotional eating triggers and addressing them through journaling, cognitive behavioral therapy, and environmental modifications prevents non-hunger related food intake and supports sustainable weight loss.
Can behavioral economics and neurocognitive techniques improve craving management?
Yes. Techniques such as pre-commitment, nudging, cognitive bias modification, and mindfulness-based cognitive therapy retrain reward pathways, reduce impulsivity, and enhance self-regulation, complementing Ozempic’s physiological effects for more effective appetite control.
How important is medical supervision during Ozempic treatment?
Medical supervision is vital to tailor dosing, optimize injection timing, monitor side effects, and integrate lifestyle strategies safely. Healthcare providers can personalize treatment plans and provide support for challenges encountered during the weight loss journey.
Trusted External Sources
- National Center for Biotechnology Information (NCBI) – Offers comprehensive peer-reviewed articles on semaglutide’s pharmacodynamics, clinical trials, and neuroendocrine regulation of appetite and stress, providing foundational scientific insights.
- Mayo Clinic – Provides evidence-based guidance on behavioral and environmental influences on hunger and weight management, essential for integrating lifestyle modifications with medication.
- Endocrine Society – Delivers expert consensus on hormone interactions related to appetite regulation, including GLP-1, ghrelin, leptin, and gut peptides, supporting clinical decision-making.
- American Psychological Association (APA) – Offers resources on cognitive-behavioral therapies and neurocognitive approaches to eating behavior, informing psychological adjuncts to pharmacotherapy.
- International Society of Microbiota – Explores emerging research on gut microbiota’s role in metabolism and drug efficacy, highlighting potential personalized interventions.
Conclusion
Effectively managing hunger cravings while using Ozempic involves more than medication alone; it requires a sophisticated blend of pharmacological understanding, behavioral strategies, and lifestyle optimization. By aligning injection timing with circadian rhythms, embracing nutrient-dense diets, prioritizing hydration and sleep, engaging in mindful movement, and addressing psychological and microbiome factors, users can significantly enhance appetite control and foster sustainable weight loss. Collaborative medical support remains indispensable to personalize these approaches safely and successfully.
Embrace this holistic framework and share your journey to inspire and support others navigating their weight loss with Ozempic. Explore related expert content and continue deepening your knowledge to transform your health outcomes with confidence.


I really appreciated the detailed exploration of how Ozempic interacts with different appetite hormones like ghrelin and leptin. In my experience, the medication definitely curbs physical hunger, but the emotional hunger cues and environmental triggers remain a challenge. I’ve found that journaling my cravings and stress levels has been quite helpful to distinguish what’s physiological hunger versus emotional eating impulses. Also, the point on synchronizing injections with circadian rhythms intrigued me—I experimented with switching my weekly dose to the morning instead of the evening and noticed better control over daytime hunger pangs, which made meal planning smoother.
Another insight from the post that resonated is the role of hydration and sleep. I underestimated how much dehydration could mimic hunger signals; simply drinking a glass of water before grabbing a snack helped reduce needless calories. The emphasis on balanced meal timing and nutrient-dense food composition provides excellent practical advice to complement Ozempic’s pharmacology.
I’m curious about others’ experiences with behavioral economic strategies like “nudging” or pre-commitment techniques for managing cravings alongside Ozempic. What small habit changes have you found effective in reducing impulsive eating? It seems combining these subtle cognitive tweaks with medical treatment can create a sustainable path to weight loss.
I completely agree with the insights shared here about balancing Ozempic’s pharmacological effects with mindful lifestyle habits. One thing I found particularly empowering was integrating mindful eating practices alongside the medication. For example, using the hunger scale to check in on my body’s actual need for food before reaching for a snack really shifted how I responded to cravings. I also noticed that chronic stress was a big contributor to emotional eating, which Ozempic alone couldn’t fully manage. Incorporating short meditation sessions and regular gentle movement like yoga helped reduce stress-induced hunger significantly.
As for behavioral strategies like ‘nudging’ or pre-commitment, I found planning meals and snacks ahead of time crucial to avoid impulsive eating, especially during busy or stressful days. Something as simple as prepping healthy snacks in portioned containers made it easier to stick to choices that complement Ozempic’s appetite suppression.
I’m curious, has anyone explored how adjusting meal frequency or macro composition influenced their hunger control while on Ozempic? I personally benefited from spacing smaller protein-rich meals throughout the day rather than traditional larger meals, which helped maintain steady energy and reduced spikes in cravings. What approaches have worked best for others in syncing their eating patterns with Ozempic’s effects?
I really appreciate the comprehensive approach this article takes on managing hunger cravings with Ozempic. One thing that stood out for me is the synergy between the medication’s pharmacological effects and behavioral strategies like mindful eating and stress management. While Ozempic effectively suppresses physiological hunger, I’ve found that addressing emotional and environmental triggers is equally crucial. For example, incorporating short walks or engaging in hobbies when a craving strikes helps me redirect my focus and prevent unnecessary snacking.
Additionally, the mention of aligning injection timing with circadian rhythms piqued my interest. I tried adjusting my injection to mornings after reading about potential benefits, and it did help reduce late-morning hunger that I used to struggle with. Combined with balanced meals rich in protein and fiber, this has made staying within my calorie goals more manageable.
I’m curious about others’ experiences with hydration strategies mentioned here. Have you experimented with drinking water before meals, and if so, did it make a noticeable difference in appetite control? Also, managing sleep quality has been a game-changer for me in reducing cravings, but it’s often overlooked. Would love to hear how fellow Ozempic users integrate sleep hygiene into their routine for better hunger management.