Harnessing Ozempic’s Power: Understanding How It Shapes Appetite
Ozempic (semaglutide) has revolutionized weight management by targeting the GLP-1 receptors that regulate hunger and satiety. Unlike traditional diets, it works by modulating the brain’s appetite center, helping users feel fuller for longer and reducing caloric intake naturally. However, to truly optimize weight loss, understanding how to synergize Ozempic’s pharmacological effects with lifestyle adjustments is crucial.
Creative Strategies to Manage Appetite Beyond Medication
While Ozempic suppresses appetite, many users still face cravings and hunger pangs, especially in social or stress-induced contexts. Employing mindful eating techniques, such as savoring meals slowly and engaging all senses, can enhance satiety signals. Incorporating high-fiber, protein-rich meals supports prolonged fullness, complementing the medication’s effects. Additionally, staying hydrated often curbs false hunger cues.
What Are the Most Effective Natural Methods to Curb Cravings While on Ozempic?
Natural craving control methods are vital adjuncts for Ozempic users. Strategies like balanced meal timing to prevent blood sugar dips, using low-calorie snacks like nuts or Greek yogurt, and distraction techniques such as short walks or deep breathing exercises can mitigate impulses. Research highlights that combining these behavioral tactics with Ozempic’s appetite suppression fosters sustainable eating habits and prevents rebound overeating (source: NIH study on appetite regulation).
Optimizing Meal Timing and Composition for Enhanced Fat Loss
Strategic meal timing aligns closely with Ozempic’s pharmacodynamics. Consuming balanced meals with a focus on low glycemic index carbohydrates stabilizes blood glucose levels and prolongs energy release. Splitting daily intake into smaller, nutrient-dense meals can prevent overwhelming hunger and support metabolic efficiency. This approach complements Ozempic’s mechanism, ensuring appetite control is consistent throughout the day.
Integrating Physical Activity to Amplify Appetite Management
Exercise not only accelerates calorie burning but also influences hormones involved in hunger regulation. Moderate aerobic activities combined with resistance training can enhance leptin sensitivity and reduce ghrelin levels, hormones pivotal to appetite modulation. For Ozempic users, a carefully tailored exercise regimen maximizes weight loss benefits and mitigates cravings by stabilizing energy demands and hormonal balance.
Expert Insights: Navigating Challenges and Enhancing Results
Weight loss with Ozempic is a journey requiring personalized strategies. Collaborating with healthcare providers ensures dosage and dietary plans are optimized for individual needs, minimizing side effects and enhancing effectiveness. Moreover, psychological support to address emotional eating and stress-related cravings can be transformative. For a comprehensive guide on safe and effective Ozempic use, explore expert-backed resources such as this detailed Ozempic safety guide.
If you’ve found these insights helpful, consider sharing your experiences or questions in the comments below to build a supportive community focused on effective and safe weight loss journeys.
My Journey with Ozempic: Learning to Listen to My Body’s Signals
When I first started using Ozempic, I quickly realized that while the medication did curb my appetite, it wasn’t a magic bullet. It required me to tune in more closely to my body’s natural hunger cues and adjust my habits accordingly. For example, I began paying attention to the difference between true hunger and emotional cravings, which was a game changer. This awareness helped me avoid unnecessary snacking and stay more consistent with my eating schedule.
Adapting Meal Plans: Finding What Truly Works for Me
One of the biggest lessons I learned was that not all low-calorie foods are equal when it comes to satisfaction. Incorporating whole foods like vegetables, lean proteins, and healthy fats helped me feel fuller for longer. I also experimented with meal timing, discovering that smaller, more frequent meals prevented the intense hunger spikes I used to experience. This approach worked harmoniously with Ozempic’s appetite suppression mechanisms, leading to smoother days without constant hunger.
How Can You Personalize Your Diet to Complement Ozempic Effects?
Personalization is key. What worked for me might not work exactly the same for you, so I encourage everyone to explore their own preferences while keeping the core principles in mind. For instance, some people find intermittent fasting helpful alongside Ozempic, while others do better with regular meals. Consulting with a registered dietitian or your healthcare provider can provide tailored guidance to optimize your plan safely. I found resources like combining injectables and nutrition especially enlightening.
Dealing with Setbacks: Staying Patient and Adjusting Expectations
Weight loss journeys are rarely linear, and I experienced my fair share of plateaus and moments of frustration. During these times, I reminded myself that consistency beats perfection. Adjusting my injectable dosage under medical supervision and tweaking my diet helped me overcome these hurdles. It’s important to recognize that the body sometimes needs time to recalibrate, especially when medications like Ozempic are involved. Staying connected with healthcare professionals made these adjustments feel safe and manageable.
Incorporating Exercise: More Than Just Burning Calories
Adding regular physical activity not only supported my weight loss but also improved my mood and energy levels. I found that a mix of brisk walking, yoga, and light strength training balanced well with my Ozempic regimen. Exercise seemed to complement the medication’s appetite control by regulating hunger hormones and improving metabolic health. If you’re curious about integrating exercise effectively, this guide on combining exercise with injectable treatments offers great practical advice.
What Are the Best Ways to Stay Motivated When Appetite Suppression Isn’t Enough?
Motivation can wane, especially when hunger still creeps in or progress slows down. For me, setting small, achievable goals and celebrating non-scale victories—like increased energy or better sleep—kept me going. Connecting with a community, whether online or in-person, helped me share challenges and gather encouragement. I often wonder how others find their motivation during tough days. What strategies have you found effective?
Feel free to share your experiences or questions below! Your insights might be the encouragement someone else needs on their weight loss journey.
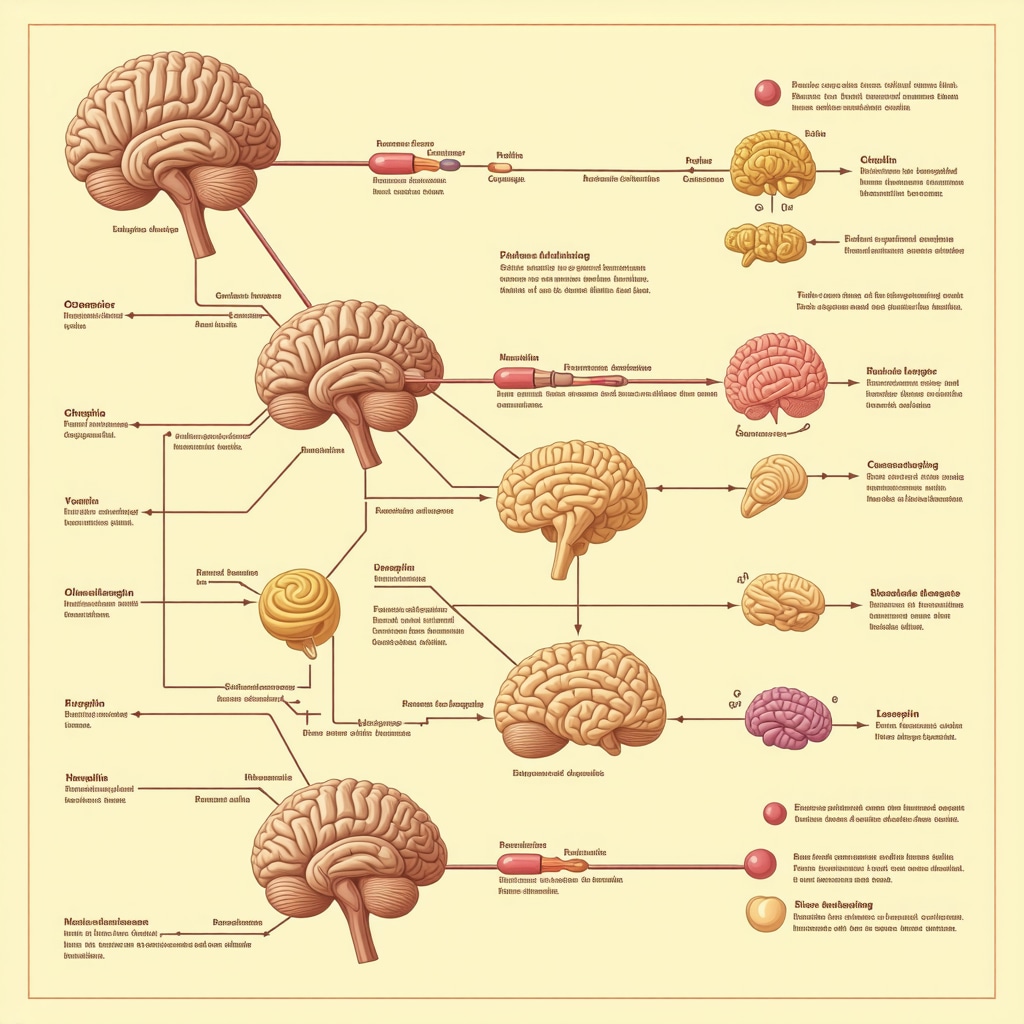
Decoding the Neuroendocrine Symphony: How Ozempic Interacts with Hunger Hormones Beyond GLP-1
While Ozempic’s primary mechanism involves GLP-1 receptor agonism to curb appetite, its influence extends much deeper into the neuroendocrine system. Emerging research reveals that semaglutide indirectly modulates key appetite-related hormones such as ghrelin and leptin. Ghrelin, often dubbed the “hunger hormone,” typically rises before meals to stimulate appetite, whereas leptin signals satiety. Ozempic appears to attenuate ghrelin secretion and enhance leptin sensitivity, creating a more balanced hormonal environment conducive to sustained appetite suppression.
This intricate hormonal interplay underscores the importance of a holistic approach to weight management. Targeting GLP-1 receptors pharmacologically sets the stage, but integrating lifestyle factors that naturally modulate ghrelin and leptin—like sleep hygiene, stress reduction, and tailored nutrition—can amplify Ozempic’s efficacy.
How Does Sleep Quality Influence Ozempic’s Effectiveness in Appetite Regulation?
Sleep profoundly impacts the hormonal milieu regulating hunger. Poor sleep elevates ghrelin levels while reducing leptin, leading to increased appetite and cravings, which may counteract Ozempic’s pharmacological suppression. Conversely, adequate restorative sleep complements Ozempic by stabilizing these hormones, enhancing satiety signals, and reducing impulsive food intake.
Studies published in the Journal Sleep demonstrate that sleep extension interventions improve leptin sensitivity and reduce ghrelin concentrations, thereby synergizing with GLP-1 receptor agonists to optimize appetite control. This evidence invites clinicians and patients alike to prioritize sleep as a critical adjunct in weight loss regimens involving Ozempic.
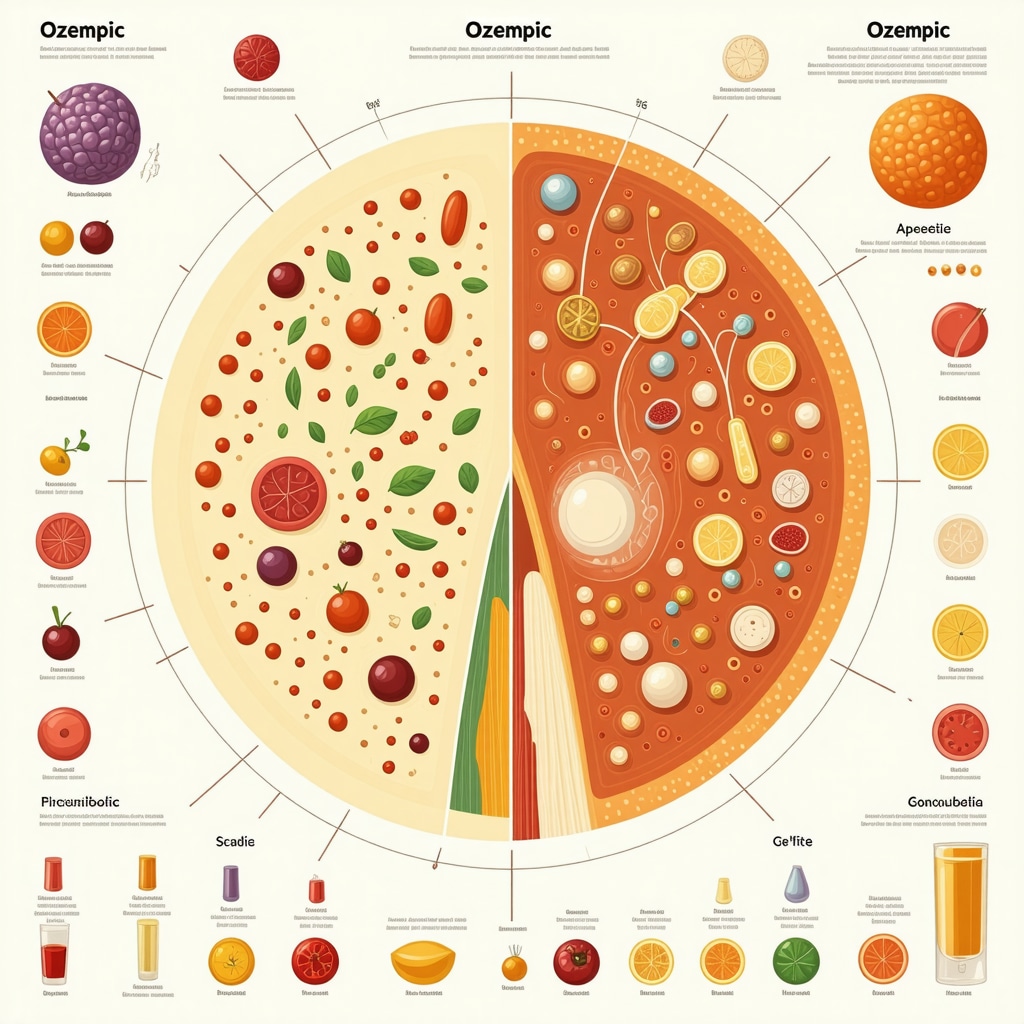
Precision Nutrition: Leveraging Macronutrient Timing and Composition to Complement Ozempic
Beyond general meal timing, the macronutrient composition of each meal plays a pivotal role in modulating hunger and satiety, especially while on Ozempic. Protein intake, in particular, stimulates the release of peptide YY and glucagon-like peptide-1, both of which enhance fullness signals. Incorporating 25-30% of daily calories from high-quality protein sources—such as lean poultry, legumes, or fish—can potentiate Ozempic’s appetite-suppressing effects.
Moreover, strategic carbohydrate consumption emphasizing low-glycemic index foods mitigates rapid glucose spikes and insulin surges, preventing reactive hypoglycemia-induced hunger. Fat, especially from sources rich in medium-chain triglycerides (MCTs), may also aid in enhancing satiety and energy metabolism. These nuanced nutritional strategies require personalized adjustments based on metabolic health, preferences, and lifestyle.
Integrating Behavioral Neuroscience: Harnessing Cognitive Techniques to Sustain Appetite Control
Pharmacotherapy alone, even as potent as Ozempic, cannot fully address the psychosocial complexities of eating behavior. Cognitive-behavioral interventions targeting mindful eating, stress management, and impulse control are instrumental in reinforcing the medication’s effects.
Practices such as stimulus control—modifying the environment to reduce exposure to high-calorie temptations—and cognitive restructuring—challenging and reframing dysfunctional thoughts about food—can mitigate emotional and habitual eating triggers. Neuroimaging studies show that GLP-1 agonists reduce activity in brain reward centers linked to food cravings, yet reinforcing these changes through behavioral interventions ensures longer-term success (Nature Communications on GLP-1 and reward pathways).
What Are the Most Effective Cognitive-Behavioral Strategies to Complement Ozempic’s Appetite Suppression?
Effective cognitive-behavioral strategies include mindful eating exercises that heighten awareness of hunger and satiety cues, stress reduction techniques such as mindfulness meditation, and planning for high-risk situations like social gatherings. Incorporation of acceptance and commitment therapy (ACT) can further empower individuals to manage cravings without relapse.
For healthcare professionals, integrating these psychological tools alongside Ozempic prescriptions can enhance adherence and mitigate the risk of compensatory overeating.
Synergizing Pharmacology with Lifestyle: A Multidisciplinary Approach to Long-Term Weight Loss Maintenance
Maximizing Ozempic’s benefits demands a comprehensive, multidisciplinary framework. Collaboration between endocrinologists, dietitians, behavioral therapists, and exercise physiologists ensures that pharmacologic appetite suppression is supported by tailored nutrition, psychological resilience, and metabolic conditioning.
Regular monitoring and adaptive modifications in medication dosing, meal planning, and physical activity regimens are vital to counteract physiological adaptations and weight plateaus. Furthermore, patient education about the neurobiological underpinnings of appetite and the expected trajectory of weight loss can foster realistic expectations and sustained motivation.
If you are navigating your own weight loss journey with Ozempic or considering its use, exploring these advanced strategies can provide invaluable support. Engaging with expert healthcare providers to develop a personalized, integrative plan will empower you to harness the full potential of this groundbreaking therapy. Share your experiences or questions below to contribute to a dynamic community dedicated to evidence-based weight management.
Exploring the Gut-Brain Axis: Unlocking Ozempic’s Full Potential Through Microbiome Interactions
Recent advances in obesity research highlight the pivotal role of the gut microbiome in regulating energy balance and appetite. Ozempic’s GLP-1 receptor agonism may modulate gut microbial composition, promoting beneficial bacteria associated with improved metabolic profiles. These changes can potentiate appetite regulation and insulin sensitivity beyond the direct pharmacologic effects.
Integrating prebiotic and probiotic interventions alongside Ozempic therapy might enhance therapeutic outcomes by fostering a gut environment conducive to weight loss and appetite control. Targeted dietary fibers and fermented foods can support this synergy, exemplifying a cutting-edge frontier in precision obesity management.
How Can Modulating the Gut Microbiota Enhance Ozempic’s Weight Loss Outcomes?
Modulating the gut microbiota presents a promising adjunct strategy to amplify Ozempic’s effects. Specific strains like Akkermansia muciniphila have been linked to improved metabolic health and reduced adiposity. Supplementing with probiotics or dietary components that encourage these microbes may enhance GLP-1 secretion and improve gut barrier function, thereby supporting sustained appetite suppression and metabolic benefits. Clinical trials are underway to elucidate these mechanisms further (source: NIH review on gut microbiome and obesity).
Precision Pharmacogenomics: Tailoring Ozempic Therapy for Individual Variability
Genetic factors significantly influence individual responses to GLP-1 receptor agonists like Ozempic. Polymorphisms affecting drug metabolism, receptor sensitivity, and neuroendocrine pathways may dictate efficacy and side effect profiles. Pharmacogenomic testing holds promise to optimize dosing strategies and predict responders versus non-responders, minimizing adverse events and maximizing therapeutic benefit.
As personalized medicine advances, integrating genomic data with clinical parameters will become essential for crafting individualized weight loss plans incorporating Ozempic.
Advanced Nutritional Timing: Chrononutrition to Support Ozempic-Induced Appetite Changes
Chrononutrition—the alignment of eating patterns with circadian rhythms—can significantly influence hormonal regulation and metabolic efficiency. Scheduling meals during daylight hours while avoiding late-night eating optimizes leptin and insulin sensitivity, complementing Ozempic’s action. Time-restricted feeding frameworks synchronized with the circadian clock may improve appetite control and fat oxidation, fostering more consistent weight loss trajectories.
Leveraging Digital Health Tools to Enhance Adherence and Behavioral Change
Emerging digital platforms utilizing artificial intelligence provide personalized feedback, meal logging, and behavioral nudges tailored to individuals on Ozempic therapy. These tools can track medication adherence, monitor appetite fluctuations, and deliver cognitive-behavioral interventions in real time, bridging gaps between clinic visits.
Such integration of technology empowers users to sustain lifestyle modifications and optimize pharmacotherapy outcomes through data-driven insights and continuous support.
What Role Do Wearable Devices and AI Apps Play in Supporting Ozempic Users?
Wearables measuring parameters like heart rate variability, glucose levels, and sleep patterns offer objective data to detect physiological states influencing appetite and metabolism. AI-driven apps analyze these data streams to customize recommendations for meal timing, activity, and stress management, synergizing with Ozempic’s pharmacodynamics. These innovations represent the cutting edge of personalized obesity treatment strategies.
Engage with Experts: Harness Multidisciplinary Insights for Sustainable Success
To truly capitalize on Ozempic’s capabilities, engaging a multidisciplinary team encompassing endocrinologists, dietitians, behavioral psychologists, and digital health specialists is paramount. This collaborative approach ensures that pharmacologic, nutritional, behavioral, and technological modalities are harmonized for maximal efficacy.
Are you ready to elevate your weight loss journey with Ozempic? Connect with healthcare professionals and leverage these advanced strategies to unlock lasting transformation. Share your questions or experiences below to contribute to this expert-driven community and empower others navigating similar paths.
Frequently Asked Questions (FAQ)
How does Ozempic specifically suppress appetite beyond just reducing hunger?
Ozempic acts as a GLP-1 receptor agonist, which not only slows gastric emptying but also influences brain centers that regulate hunger and satiety. Additionally, it modulates neuroendocrine hormones like ghrelin and leptin, reducing hunger signals and enhancing fullness, resulting in a multifaceted appetite suppression effect.
Can lifestyle factors like sleep and stress impact the effectiveness of Ozempic?
Absolutely. Poor sleep elevates hunger hormones such as ghrelin and lowers satiety hormones like leptin, potentially counteracting Ozempic’s appetite suppression. Chronic stress can trigger emotional eating and hormonal imbalances. Prioritizing restorative sleep and stress management enhances Ozempic’s efficacy by stabilizing appetite-regulating hormones.
What dietary strategies best complement Ozempic to optimize weight loss?
Incorporating high-quality protein (25-30% of daily intake), low-glycemic carbohydrates, and healthy fats supports prolonged satiety and metabolic balance. Timing meals to align with circadian rhythms (chrononutrition) and dividing intake into smaller, nutrient-dense portions can synergize with Ozempic’s pharmacodynamics for enhanced appetite control.
How important is exercise in conjunction with Ozempic therapy?
Exercise plays a critical role by improving hormonal sensitivity (e.g., leptin), reducing hunger-inducing hormones (e.g., ghrelin), and enhancing metabolic rate. Combining aerobic and resistance training maximizes weight loss outcomes and mitigates cravings, complementing the medication’s appetite-suppressing effects.
Are there cognitive or behavioral techniques that enhance Ozempic’s appetite control?
Yes, cognitive-behavioral strategies such as mindful eating, stress reduction (meditation, deep breathing), stimulus control, and acceptance and commitment therapy (ACT) help manage emotional and habitual eating. These approaches reinforce pharmacologic effects and support long-term behavioral change.
Can gut microbiome modulation improve outcomes when using Ozempic?
Emerging evidence suggests that promoting beneficial gut bacteria through prebiotics, probiotics, and dietary fibers can enhance GLP-1 secretion and metabolic health. This gut-brain axis interplay may potentiate Ozempic’s efficacy in appetite suppression and weight management.
What role do genetics play in individual responses to Ozempic?
Genetic variations affecting drug metabolism, receptor sensitivity, and neuroendocrine pathways influence how individuals respond to Ozempic. Pharmacogenomic testing could enable personalized dosing and therapy optimization, reducing side effects and improving efficacy.
How can digital health tools support adherence and behavioral changes during Ozempic treatment?
Wearable devices and AI-driven apps track physiological data (sleep, glucose, activity) and provide personalized feedback, reminders, and behavioral nudges. These tools help users maintain medication adherence, monitor appetite fluctuations, and sustain lifestyle modifications to maximize treatment benefits.
Is Ozempic a standalone solution for weight loss?
No. While Ozempic is a powerful pharmacologic agent, sustainable weight loss requires an integrated approach combining medication, personalized nutrition, physical activity, behavioral strategies, and often multidisciplinary healthcare support.
What should patients do if they experience plateaus or setbacks during Ozempic therapy?
Plateaus are common and may require dosage adjustments under medical supervision, dietary recalibration, or increased physical activity. Maintaining patience, consistent habits, and consulting healthcare professionals ensures safe navigation through challenges.
Trusted External Sources
- National Institutes of Health (NIH) – Appetite Regulation Research: Provides comprehensive studies on hormonal control of hunger and the mechanisms of GLP-1 receptor agonists, foundational for understanding Ozempic’s pharmacology.
- Journal Sleep (Oxford Academic): Offers in-depth research on sleep’s impact on appetite hormones like ghrelin and leptin, highlighting the importance of sleep hygiene in weight management.
- Nature Communications – GLP-1 and Reward Pathways Study: Explores neuroimaging evidence on how GLP-1 agonists modulate brain reward centers, informing behavioral intervention strategies.
- NIH Review on Gut Microbiome and Obesity: Details the role of gut bacteria in metabolic regulation and potential synergy with GLP-1 therapies like Ozempic.
- American Diabetes Association (ADA): Provides clinical guidelines and evidence-based recommendations for the use of GLP-1 receptor agonists in obesity and diabetes management.
Conclusion
Ozempic represents a groundbreaking advancement in appetite regulation and weight management by leveraging GLP-1 receptor pathways and influencing complex neuroendocrine systems. Its efficacy is maximized when integrated into a holistic approach encompassing precision nutrition, tailored exercise, behavioral neuroscience, and emerging modalities like gut microbiome modulation and digital health tools. Personalized strategies addressing individual variability, lifestyle factors, and psychological components are essential for sustainable success. Engaging multidisciplinary expertise and leveraging innovative technologies empower patients to harness Ozempic’s full potential safely and effectively. Whether you are beginning your journey or seeking to optimize ongoing therapy, embracing a comprehensive, expert-driven approach will enhance outcomes and foster lasting transformation. Share your experiences and questions to contribute to a community united in advancing evidence-based weight loss with Ozempic.


I find the way Ozempic works on the brain’s appetite center fascinating, especially how it not only reduces hunger but also modifies hormones like ghrelin and leptin to create a balanced hormonal environment. From my own experience, combining Ozempic with mindful eating has been crucial. Slowing down to really savor each bite helped me recognize true hunger versus emotional cravings, something the post touches on. Also, focusing on meals rich in protein and fiber while staying consistent with balanced meal timing made a huge difference in managing those stubborn cravings that sometimes pop up, especially in social settings.
One challenge I’ve encountered is integrating exercise in a way that complements the medication without overexerting myself, as my energy levels can fluctuate. I’m curious how other Ozempic users tailor their physical activity routines to support appetite control and weight loss without feeling drained? Have you found particular types of exercise or timing that work best with Ozempic’s effects?
Reading through this comprehensive overview, I can relate to how balancing medication with lifestyle adjustments truly makes a difference in long-term weight management. I’ve personally started emphasizing sleep hygiene and stress reduction strategies, recognizing their impact on hunger hormones like ghrelin and leptin. Since poor sleep often triggers increased cravings, integrating a consistent sleep schedule has helped me feel more in control, especially during periods when my appetite feels harder to manage.
On the nutritional front, experimenting with meal timing and macronutrient composition—focusing on high-protein, fiber-rich foods—has been a game-changer. It complements Ozempic’s effects nicely by keeping me fuller longer and preventing those awful
This post resonates with me because I’ve found that integrating moderate exercise along with mindful eating significantly supports my weight management on Ozempic. I’ve been focusing on brisk walking and yoga, especially during the times I notice increased hunger cues. These activities seem to complement the medication well by maintaining hormonal balance and reducing stress, which is crucial because stress-related cravings can still pop up despite the appetite suppression. I also pay close attention to meal composition—prioritizing protein and fiber—and timing, to maximize fullness and stability throughout the day.
Regarding the exercise routines, I’d love to hear from others about what has worked best for them—do you find that morning workouts help, or do you prefer evening sessions? Also, how do you adjust your activity levels if you’re feeling more fatigued during certain phases of your medication? Finding the right balance can be tricky, but sharing experiences might help us all develop more effective strategies.