Unlocking the Power of Ozempic: Beyond the Injection
Ozempic, a GLP-1 receptor agonist, has revolutionized weight management for many struggling with obesity and metabolic conditions. However, the injection alone is not a magic bullet. To truly harness its benefits, users must integrate essential lifestyle hacks that enhance its fat loss potential while supporting overall health. This article dives into expert-backed strategies tailored specifically for Ozempic users seeking sustainable and effective weight loss.
Synergizing Diet and Ozempic for Optimal Fat Loss
While Ozempic naturally curbs appetite and slows gastric emptying, pairing it with a nutrient-dense, balanced diet amplifies results. Emphasizing whole foods such as lean proteins, fiber-rich vegetables, and healthy fats helps maintain satiety and stabilize blood sugar levels. Avoiding highly processed carbohydrates reduces insulin spikes that can counteract weight loss efforts. This dietary synergy with Ozempic aligns with evidence-based nutritional principles, enhancing metabolic efficiency and promoting steady fat reduction (source).
Integrating Smart Exercise: Moving Beyond Calories Burned
Physical activity is a cornerstone of weight management but demands a nuanced approach when combined with Ozempic. Given that the medication modulates appetite, users might experience less energy intake, necessitating carefully planned exercise routines to prevent muscle loss. Resistance training paired with moderate aerobic activity fosters lean muscle preservation, which is critical for maintaining a healthy metabolic rate. Additionally, exercise enhances insulin sensitivity, complementing Ozempic’s glucose-regulating effects for improved metabolic health.
Mastering Hunger Control: How Does Ozempic Influence Cravings?
How Can Ozempic Users Effectively Manage Hunger and Cravings?
Ozempic’s mechanism reduces hunger by mimicking incretin hormones, yet the psychological and habitual aspects of cravings remain. Strategies such as mindful eating, regular meal schedules, and hydration are crucial. For example, practicing mindfulness during meals helps users recognize true hunger cues versus emotional triggers. Furthermore, spacing meals to prevent excessive hunger can reduce overeating episodes. Combining these behavioral hacks with Ozempic’s pharmacological effects leads to better appetite regulation and sustained fat loss (source).
Prioritizing Sleep and Stress Management: Invisible Pillars of Weight Loss
Often overlooked, quality sleep and stress reduction significantly influence weight loss outcomes. Poor sleep disrupts hunger hormones like ghrelin and leptin, increasing appetite and cravings, potentially undermining Ozempic’s effects. Similarly, chronic stress elevates cortisol levels, promoting fat storage, especially visceral fat. Integrating relaxation techniques such as meditation, deep breathing, or gentle yoga supports hormonal balance, thus complementing the medication’s benefits.
Why Is Personalized Medical Guidance Crucial When Using Ozempic?
How Can Regular Medical Supervision Enhance Weight Loss Success with Ozempic?
Each individual’s response to Ozempic varies, making tailored medical oversight essential. Physicians can adjust dosage, monitor side effects, and optimize injection timing to maximize efficacy. Moreover, comprehensive weight loss plans that include behavioral counseling and nutrition adjustments are often more successful. According to peer-reviewed research, combining pharmacotherapy with personalized lifestyle interventions yields superior long-term outcomes.
For those seeking expert advice on optimizing their Ozempic journey, exploring medically supervised programs can offer structured support and accountability (source).
Engage with us: Have you tried any lifestyle hacks alongside Ozempic? Share your experiences or questions in the comments below to help build a supportive community focused on effective, sustainable weight loss.
Embracing the Journey: Personal Reflections on Consistency and Patience
From my own experience with Ozempic, one of the most valuable lessons I’ve learned is that consistency is key. It’s tempting to expect rapid results, but weight loss—especially when combining medication with lifestyle changes—is a gradual process. I found that sticking to a steady routine, whether it was my injection schedule, meal planning, or exercise, helped build momentum. Patience with my body’s response was just as important as the actions themselves. This mindset shift made the journey feel less like a race and more like sustainable transformation.
Hydration and Its Subtle Influence on Weight Management
Another practical tip that often flies under the radar is the role of proper hydration. Ozempic users might notice changes in appetite and digestion, which can sometimes lead to dehydration if not mindful. Drinking enough water throughout the day not only supports metabolic processes but also helps manage hunger cues, as sometimes thirst is mistaken for hunger. I personally started carrying a reusable water bottle everywhere, turning hydration into an effortless habit that complemented my overall regimen.
Addressing Common Challenges: Navigating Side Effects Without Losing Momentum
Like many, I encountered mild side effects such as nausea and occasional fatigue when starting Ozempic. What helped me was open communication with my healthcare provider and gradual dose adjustments. Incorporating lighter meals during initial periods and focusing on nutrient-dense, easy-to-digest foods also made a difference. These strategies prevented discouragement and kept me motivated. For those interested, resources like avoiding side effects in prescription injection weight loss provide excellent guidance on managing these nuances.
Curious: How Do You Stay Motivated When Progress Slows?
Weight loss journeys are rarely linear, and slowing progress can be frustrating. Reflecting on this, I realized that celebrating small victories—like improved energy or better sleep—helped me stay positive. Also, mixing up my routine with new recipes or varied workouts kept things fresh. I’d love to hear how you maintain motivation during plateaus or challenges. Sharing your stories might inspire others navigating similar paths!
Combining Ozempic with Behavioral Techniques: A Winning Formula
Beyond the biological effects of Ozempic, I found incorporating behavioral methods like journaling my food intake and emotions helpful. This practice brought awareness to triggers and patterns that I might otherwise overlook. It also highlighted how stress or social settings influenced my eating habits. Coupling these insights with medication made my approach more holistic and effective. If you want to explore this further, check out doctor-backed weight loss combining injections with lifestyle for comprehensive strategies.
Leveraging Neurobehavioral Insights: Enhancing Ozempic’s Appetite Suppression Through Cognitive Techniques
Understanding the neurobehavioral mechanisms behind appetite regulation allows Ozempic users to amplify the medication’s physiological effects. Ozempic acts on GLP-1 receptors to modulate hunger signals centrally, but integrating cognitive behavioral therapy (CBT) strategies can disrupt conditioned eating patterns, emotional triggers, and reward circuits involved in overeating. Techniques such as stimulus control, cognitive restructuring, and mindfulness-based stress reduction create a mental environment conducive to sustained appetite control.
For example, stimulus control involves identifying and modifying environmental cues that prompt unnecessary eating—like avoiding keeping high-calorie snacks within reach or creating designated eating zones. Cognitive restructuring challenges irrational thoughts about food and body image, fostering healthier attitudes and reducing emotional eating episodes. These methods synergize with Ozempic’s pharmacodynamics, creating a robust defense against relapse into unhealthy eating behaviors.
Fine-Tuning Gut Microbiota: Emerging Evidence on Microbiome Modulation to Support Ozempic Efficacy
The gut microbiome’s role in obesity and metabolic health is an exciting frontier relevant to Ozempic users. Recent studies suggest that the composition and diversity of intestinal microbes influence GLP-1 secretion and responsiveness, potentially affecting the drug’s effectiveness. Incorporating prebiotic-rich foods like inulin, resistant starches, and fermented products such as kimchi or kefir may enhance GLP-1 receptor activity and improve insulin sensitivity.
Moreover, personalized microbiome analysis could guide dietary adjustments tailored to optimize Ozempic response. This precision nutrition approach aligns with the concept of individualized medicine, recognizing that one-size-fits-all diets rarely achieve maximal outcomes. Complementary probiotics supplementation, particularly strains like Akkermansia muciniphila and Lactobacillus rhamnosus, has shown promise in modulating metabolic pathways linked to weight regulation (Nature Medicine, 2020).
What Are the Best Practices for Combining Behavioral Therapy with Ozempic Treatment?
Integrating behavioral therapy with pharmacological treatment requires a multidisciplinary approach. Optimal practices involve regular sessions with a psychologist or counselor trained in weight management, focusing on habit formation, emotional regulation, and relapse prevention. Setting SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals improves adherence and motivation. Digital health platforms can augment this process by offering real-time feedback and tracking.
Importantly, this integrated approach must be dynamic, adapting to individual progress and challenges. Collaboration between prescribing physicians, dietitians, and behavioral specialists ensures a coherent, patient-centered plan that maximizes Ozempic’s benefits while addressing psychological components of obesity.
Advanced Nutrient Timing: Synchronizing Meal Patterns with Ozempic Pharmacokinetics
Precision in meal timing relative to Ozempic injection can substantially influence fat loss outcomes. Ozempic exhibits peak plasma concentrations approximately 1 to 3 days post-injection, with steady-state achieved after 4 to 5 weeks. Aligning higher protein and fiber intake during peak drug activity periods can optimize satiety and glucose regulation.
Furthermore, intermittent fasting protocols such as time-restricted feeding (e.g., 16:8) may be particularly effective when synchronized with Ozempic’s pharmacodynamics. This approach exploits prolonged periods of low insulin and enhanced lipolysis, capitalizing on the medication’s appetite suppression and gastric emptying delay. However, individualized assessment is necessary to avoid hypoglycemia or nutritional deficiencies.
For those interested in a deeper dive into nutrient timing strategies, consulting with a registered dietitian familiar with GLP-1 receptor agonist therapies is strongly recommended.
Ready to elevate your Ozempic journey? Explore our comprehensive guides and expert consultations designed to integrate behavioral, nutritional, and pharmacological strategies for sustainable fat loss.
Decoding the Synergistic Effects of Ozempic and Circadian Nutrition
Emerging research underscores the importance of circadian rhythms in metabolic regulation, presenting a compelling case for aligning Ozempic administration and meal timing with the body’s internal clock. Chrononutrition—eating in harmony with circadian biology—can potentiate Ozempic’s efficacy by optimizing glucose metabolism and hormonal secretions involved in appetite control. For instance, consuming the majority of daily calories earlier in the day when insulin sensitivity peaks can enhance fat oxidation during Ozempic’s pharmacological window.
Precision Pharmacotherapy: Tailoring Ozempic Dosage Through Pharmacogenomic Insights
Pharmacogenomics offers a promising frontier in customizing Ozempic therapy. Genetic polymorphisms affecting GLP-1 receptor sensitivity and drug metabolism may explain interindividual variability in therapeutic response. By integrating genotypic data, clinicians can refine dosing strategies to maximize weight loss while minimizing adverse effects. Although still nascent, this approach exemplifies personalized medicine’s potential to elevate treatment outcomes beyond standard protocols.
How Can Pharmacogenomic Testing Inform Ozempic Treatment Plans for Enhanced Weight Loss?
Pharmacogenomic testing deciphers genetic variants influencing drug response pathways, including those related to GLP-1 receptor signaling and hepatic metabolism enzymes. Identifying these variants allows healthcare providers to anticipate differential efficacy or side effect profiles, facilitating dose adjustments or alternative therapies. For example, patients with reduced receptor sensitivity may require higher or adjunctive dosing, while those with metabolic enzyme polymorphisms might benefit from modified administration intervals. Integrating such precision diagnostics into clinical practice demands collaboration between genetic counselors, endocrinologists, and pharmacologists to tailor Ozempic therapy effectively.
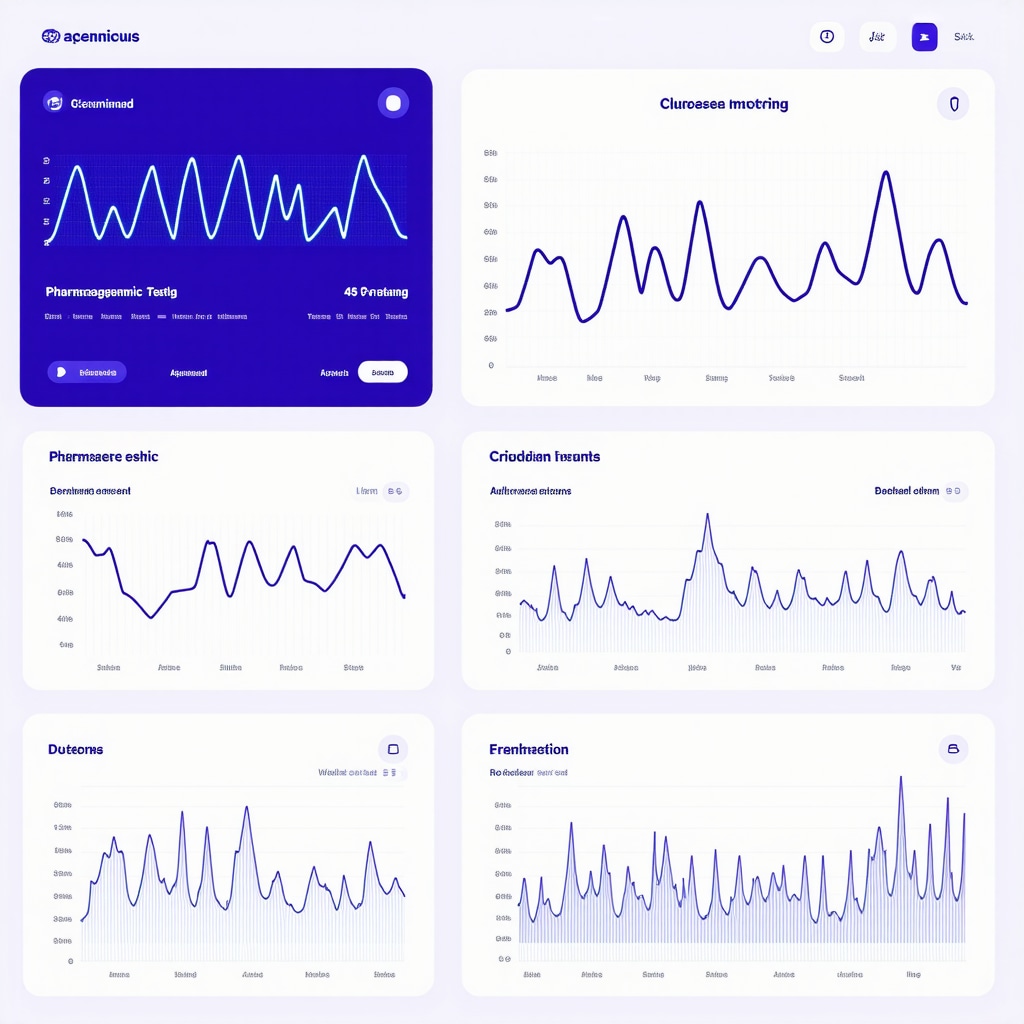
Advanced Monitoring: Utilizing Continuous Metabolic Tracking Technologies
Adopting continuous glucose monitoring (CGM) and wearable metabolic sensors can provide real-time insights into glycemic variability, energy expenditure, and behavioral patterns. These data empower Ozempic users and clinicians to fine-tune lifestyle interventions and medication schedules responsively. For instance, CGM trends may reveal postprandial hyperglycemia or hypoglycemia, guiding dietary adjustments to maintain metabolic stability. Wearable devices tracking heart rate variability and sleep quality further contextualize physiological stressors that impact weight loss trajectories.
Integrating such digital health tools aligns with the latest recommendations from the American Diabetes Association on CGM utilization, emphasizing personalized feedback loops to optimize therapeutic outcomes.
What Are the Cutting-Edge Behavioral Interventions Complementing Ozempic Therapy?
High-level behavioral interventions, including digital cognitive-behavioral therapy (CBT) platforms and virtual coaching, are transforming weight management paradigms. These modalities leverage artificial intelligence to deliver adaptive, evidence-based support focused on habit modification, stress resilience, and emotional regulation. For Ozempic users, integrating such tailored behavioral tools enhances adherence, mitigates psychological barriers, and fosters sustainable lifestyle changes that amplify pharmacological benefits.
Combining these interventions with traditional clinical oversight creates a multifaceted support system critical for long-term success in obesity treatment.
Engage with Cutting-Edge Ozempic Optimization Strategies
Unlock the full spectrum of Ozempic’s potential by embracing these advanced strategies—circadian-aligned nutrition, pharmacogenomic-informed dosing, continuous metabolic monitoring, and innovative behavioral therapies. Connect with our expert team to personalize your approach and navigate the complexities of weight loss with precision and confidence. Start your tailored consultation today and transform your Ozempic journey into a sustainable success story.
Frequently Asked Questions (FAQ)
What is Ozempic and how does it aid in weight loss?
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist primarily prescribed for type 2 diabetes but also effective for weight loss. It works by enhancing insulin secretion, slowing gastric emptying, and reducing appetite, thereby promoting fat loss when combined with lifestyle changes.
Can I lose weight on Ozempic without changing my diet or exercise routine?
While Ozempic suppresses appetite and can induce weight loss independently, combining it with a balanced diet and regular physical activity significantly enhances and sustains fat loss results. Relying solely on the medication without lifestyle modifications often limits long-term success.
How should I time my meals in relation to Ozempic injections?
Optimizing meal timing around Ozempic’s pharmacokinetics—peak plasma levels occurring 1 to 3 days post-injection—can enhance satiety and glucose control. Incorporating higher protein and fiber intake during this window supports metabolic benefits. Time-restricted eating protocols may also synergize well but should be personalized.
What behavioral strategies complement Ozempic therapy?
Behavioral interventions such as cognitive-behavioral therapy (CBT), mindful eating, journaling, and stimulus control help manage emotional eating and cravings. These approaches disrupt habitual overeating patterns and work synergistically with Ozempic’s appetite suppression to promote sustainable lifestyle change.
Are there genetic factors that influence how effective Ozempic is for me?
Yes, pharmacogenomic variations affecting GLP-1 receptor sensitivity and drug metabolism can influence individual responses. Genetic testing can guide personalized dosing strategies to maximize efficacy and minimize side effects, although this is an emerging area requiring clinical collaboration.
How can I manage common side effects like nausea when starting Ozempic?
Starting with a low dose and gradually titrating up helps mitigate nausea and fatigue. Eating smaller, nutrient-dense, easily digestible meals and maintaining open communication with your healthcare provider are essential strategies to maintain momentum during initial adjustment periods.
Is continuous glucose monitoring beneficial while on Ozempic?
Continuous glucose monitoring (CGM) provides real-time data on blood sugar trends that can inform dietary choices and medication timing. It helps identify postprandial glucose spikes or hypoglycemia risks, enabling tailored lifestyle adjustments to optimize metabolic control alongside Ozempic therapy.
What role does the gut microbiome play in Ozempic’s effectiveness?
The gut microbiome influences GLP-1 secretion and receptor responsiveness. Consuming prebiotic-rich and fermented foods, and potentially probiotic supplementation with specific strains, may enhance Ozempic’s metabolic effects by modulating microbiota composition and improving insulin sensitivity.
How important is sleep and stress management when using Ozempic?
Quality sleep and stress reduction are critical as they regulate hormones like ghrelin, leptin, and cortisol that affect appetite and fat storage. Integrating relaxation techniques supports hormonal balance, reinforcing Ozempic’s appetite-suppressing benefits and improving overall weight loss outcomes.
Should I seek professional support during my Ozempic weight loss journey?
Yes, personalized medical supervision including regular check-ins, behavioral counseling, and nutritional guidance significantly improves success. Multidisciplinary approaches ensure dose optimization, side effect management, and sustained lifestyle adherence for long-term fat loss.
Trusted External Sources
- National Institutes of Health (NIH) – PubMed Central: Offers peer-reviewed clinical studies on GLP-1 receptor agonists like Ozempic, providing evidence-based insights on efficacy, safety, and pharmacology.
- American Diabetes Association (ADA): Provides authoritative guidelines on diabetes medications, including CGM recommendations and comprehensive metabolic management relevant to Ozempic users.
- Nature Medicine: Publishes cutting-edge research on gut microbiome interactions with metabolic therapies, crucial for understanding microbiome modulation in weight loss.
- Obesity Society: A leading professional organization offering expert consensus on obesity treatment, behavioral strategies, pharmacotherapy integration, and emerging precision medicine approaches.
- Endocrine Society: Offers clinical practice guidelines and pharmacogenomic research data pertinent to optimizing GLP-1 receptor agonist therapies including Ozempic.
Conclusion
Harnessing Ozempic’s full weight loss potential requires a multifaceted and personalized strategy that transcends injection alone. Integrating evidence-based dietary modifications, smart exercise regimens, behavioral therapies, and emerging precision tools such as pharmacogenomics and continuous metabolic monitoring empowers users to achieve sustainable fat loss. Prioritizing sleep, stress management, and gut microbiome health further amplifies therapeutic outcomes. Medical supervision remains indispensable to tailor dosing, manage side effects, and adapt interventions dynamically. Ultimately, embracing an informed, patient-centered approach transforms Ozempic from a standalone medication into a cornerstone of effective, long-lasting obesity management. We encourage you to share your experiences, explore our expert guides, and consult healthcare professionals to unlock your personalized path to success with Ozempic.


I’ve been using Ozempic for several months, and I’ve noticed that its appetite-suppressing effects are most beneficial when paired with a structured routine rather than just relying on the medication alone. The post rightly emphasizes how crucial it is to integrate smart exercise like resistance training to preserve lean muscle—something I initially overlooked and regretted when the scale stalled despite a reduced appetite. Additionally, hydration often gets underestimated; I’ve found that staying well-hydrated not only helps with hunger cues but also supports overall digestion and energy during workouts.
What I find particularly interesting is the integration of behavioral therapies discussed here. Mindful eating practices, especially recognizing emotional versus true hunger, have helped me avoid slipping into old snacking habits that could sabotage progress even with Ozempic. Personalizing meal timing in alignment with the drug’s pharmacokinetics seems promising, though I haven’t tried that aspect yet.
I’m curious about others’ experiences balancing reduced calorie intake with sufficient energy for exercise. How do you maintain stamina during workouts when appetite is significantly suppressed? Have you adapted your nutrition or exercise plans to accommodate this? I’d love to hear strategies that have worked in conjunction with Ozempic to keep active and preserve muscle without feeling drained.
Lydia, your insight about balancing reduced calorie intake with exercise while on Ozempic really resonates with me. I’ve also experienced appetite suppression that made it tempting to cut back too much on fuel for workouts, which often led to low energy and reduced exercise intensity initially. What worked for me was focusing on nutrient timing, particularly consuming a small, protein-rich snack about 30 to 60 minutes before exercising. This gave me enough energy without triggering excessive hunger later on. Additionally, incorporating resistance training with moderate aerobic sessions helped preserve lean muscle mass, as the article suggests. From experience, hydration is another critical piece — sometimes fatigue is exacerbated by dehydration, especially when appetite dips and fluid intake decreases. One strategy I found helpful was setting reminders to drink water throughout the day to avoid that. I’m curious if others have tried targeted pre-workout nutrition or specific supplements alongside Ozempic to help sustain workout performance? Also, has anyone experimented with adjusting exercise timing to coincide with peak Ozempic activity to optimize energy and fat oxidation? Would love to hear what approaches have helped others maintain stamina and muscle while benefitting from Ozempic’s appetite control.
Great points, Lydia and Marcus — wanted to add a few practical tweaks that helped me keep energy and preserve muscle while on Ozempic. For pre-workout fuel I aim for a small, easily digestible snack 30–60 minutes before resistance sessions: examples that work are 1) 3/4 cup Greek yogurt with a few berries (12–18 g protein + some carbs), 2) a 6–8 oz protein shake with a small banana, or 3) whole-grain toast with a thin spread of almond butter. Those ~150–250 kcal options give usable energy without blowing appetite suppression.
On supplements: creatine monohydrate (3–5 g/day) has good evidence for preserving strength and lean mass and is safe for most people; low-dose caffeine (100 mg) can boost short workouts but test tolerance first. I’d be cautious with stimulants if you have BP/glucose concerns and always check with your clinician.
About timing: some people schedule harder resistance workouts on days when they feel less nauseous or slightly hungrier (everyone’s 1–3 day post-injection window differs). Tracking energy, CGM trends if available, and simple food/workout logs helped me fine-tune timing.
Has anyone else found a specific snack or supplement that reliably preserves workout intensity on Ozempic?
I can relate to the importance of combining lifestyle adjustments with Ozempic for better results. In my experience, focusing on small, nutrient-dense snacks before workouts has really helped maintain energy levels, especially during the initial weeks when appetite suppression is strongest. I started using low-fat Greek yogurt with a handful of berries or a small protein shake, which kept me energized without feeling too full. What fascinates me is the role of timing—aligning meals and snacks with Ozempic’s peak activity seems like a promising way to optimize fat oxidation and maintain stamina. Has anyone experimented with specific timing strategies to enhance workout performance while on Ozempic? Also, I wonder if incorporating certain supplements like BCAAs or electrolytes could further support muscle preservation during this process. It’s encouraging to hear how others are navigating this balance—luckily, sharing these experiences helps us all find what works best!