Unlocking the Secrets of Science-Driven Weight Loss: Are Injectables the Future?
Imagine a world where shedding pounds isn’t just about willpower but backed by cutting-edge science. Welcome to the era of supervised injectable weight loss programs—where medicine meets motivation in a dance as old as history but with a modern twist. If you’ve ever wondered whether those tiny injections could truly transform your weight journey, buckle up—you’re about to find out!
Why Are Injectables Making Headlines in the Weight Loss Arena?
Injectable treatments like GLP-1 receptor agonists—think Wegovy or Ozempic—are turning heads for their proven ability to suppress appetite and boost fat loss. But what makes these options a game changer? The secret lies in their science-backed mechanisms. These medications mimic hormones that regulate hunger, making it easier for patients to stick to their diets while accelerating weight reduction. And because they’re administered under medical supervision, risks are minimized—a win-win scenario.
Science-Driven Strategies to Maximize Results
Are You Leveraging the Full Potential of Medical Guidance?
One of the key pillars of successful injectable weight loss programs is medical oversight. Experts emphasize the importance of personalized treatment plans tailored to individual health profiles. Consulting a healthcare professional ensures proper dosing, monitors side effects, and adjusts the protocol as needed. For those curious about integrating these treatments safely, exploring resources like mastering prescription injections with medical guidance can be enlightening.
But what about combining these injections with lifestyle changes? The science suggests that pairing pharmacological support with diet and exercise creates the perfect storm for sustainable weight loss. It’s not just about the shot—it’s about a holistic approach that includes nutrition, activity, and behavioral modifications.
The Future Is Now—And It’s Supervised
In a recent review published by Harvard Medical School, researchers highlighted the importance of supervised programs in achieving optimal outcomes and safety. This approach prevents misuse, reduces side effects, and enhances long-term success. So, if you’re considering this route, remember: the journey is best navigated with professional guidance.
Isn’t It Time to Put Science on Your Side?
If you’re eager to explore how science-driven injectables could revolutionize your weight loss efforts, don’t hesitate to reach out to qualified clinicians. Your personalized plan awaits, and the benefits could be life-changing. Share your thoughts below—are you ready to embrace the future of weight loss?
For more detailed insights on safe practices, visit supervised injectable weight loss programs and discover how science and safety go hand in hand.
Unlocking the Power of Personalized, Science-Backed Weight Loss Strategies
As the landscape of weight management evolves, one thing is clear: the integration of medical supervision with innovative injectable treatments is revolutionizing how we approach fat loss. These therapies, such as semaglutide and tirzepatide, are not just fleeting trends—they are backed by robust scientific research that demonstrates their efficacy and safety when used under professional guidance. For individuals seeking sustainable results, understanding the nuances of these therapies and their practical application is crucial.
Why Is Medical Supervision Essential for Injectables?
Supervision by healthcare professionals ensures that treatment plans are tailored to individual health profiles, reducing risks of adverse effects and optimizing outcomes. Proper dosing, monitoring for side effects, and adjusting treatment protocols as needed are fundamental components that only a qualified clinician can provide. This holistic, personalized approach aligns with the latest research from institutions like Harvard Medical School, emphasizing that supervised programs significantly enhance success rates and safety (source).
Can Combining Injections with Lifestyle Changes Accelerate Fat Loss?
Absolutely. The synergy between pharmacological support and lifestyle modifications—such as dietary adjustments and regular exercise—is where science truly shines. For example, targeted meal timing and activity routines can amplify the effects of medications like Wegovy or Ozempic, leading to more rapid and sustained weight loss. Experts recommend consulting resources like these guidelines to craft a comprehensive plan that maximizes results while maintaining safety.
What Are the Long-Term Benefits of a Science-Backed, Supervised Approach?
Long-term success hinges on consistency, personalized care, and ongoing professional support. Regular check-ins help prevent potential side effects, address behavioral challenges, and adapt strategies as needed. Moreover, combining injectables with nutritional counseling and physical activity fosters a sustainable lifestyle change rather than a quick fix. As noted by leading experts, this integrated approach not only accelerates fat loss but also sustains it, making it a cornerstone of modern weight management (source).
Are You Ready to Embrace the Future of Weight Loss with Confidence?
If you’re inspired to explore how scientifically supported, medically supervised injectables could reshape your weight journey, consider reaching out to qualified clinicians. Your personalized plan, rooted in the latest research, can be the catalyst for lasting change. Share your experiences or questions below—what’s holding you back from taking this innovative step?
For more insights on safe and effective injectable weight loss strategies, visit mastering prescription injections with medical guidance and discover how professional support makes all the difference.
Integrating Advanced Pharmacology with Holistic Lifestyle Interventions: A Paradigm Shift in Weight Management
As we delve deeper into the realm of science-driven weight loss, it becomes apparent that the synergy between cutting-edge pharmacological developments and personalized behavioral strategies is redefining success metrics. The advent of novel GLP-1 receptor agonists, such as semaglutide and tirzepatide, offers unprecedented efficacy coupled with improved safety profiles, provided they are administered under rigorous medical supervision. These medications modulate complex hormonal pathways—like the incretin system—to suppress appetite, enhance satiety, and promote lipolysis, effectively targeting both neural and metabolic pathways involved in obesity.
However, their optimal utilization transcends mere prescription. Integrating these agents with bespoke nutritional plans and tailored physical activity regimens amplifies their effects. Recent research from the Journal of Clinical Endocrinology & Metabolism emphasizes that combining pharmacotherapy with structured lifestyle modifications can lead to sustained weight loss exceeding 15% of initial body weight over 12 months, significantly surpassing standalone approaches (source).
What are the neural adaptations underpinning the success of injectable therapies combined with behavioral modification?
Emerging neuroimaging studies reveal that successful weight loss facilitated by injectables involves profound changes in hypothalamic and reward-related brain circuits. These modifications reduce the hedonic drive to consume high-calorie foods and recalibrate energy homeostasis. Understanding these neural plasticity mechanisms allows clinicians to design more effective, psychologically informed interventions, ensuring that pharmacological effects translate into behavioral change—an area ripe for further exploration by neuroendocrinologists and behavioral scientists alike.
To maximize these benefits, clinicians advocate for integrated programs that incorporate cognitive-behavioral therapy, motivational interviewing, and ongoing support, creating a comprehensive ecosystem for lasting change.
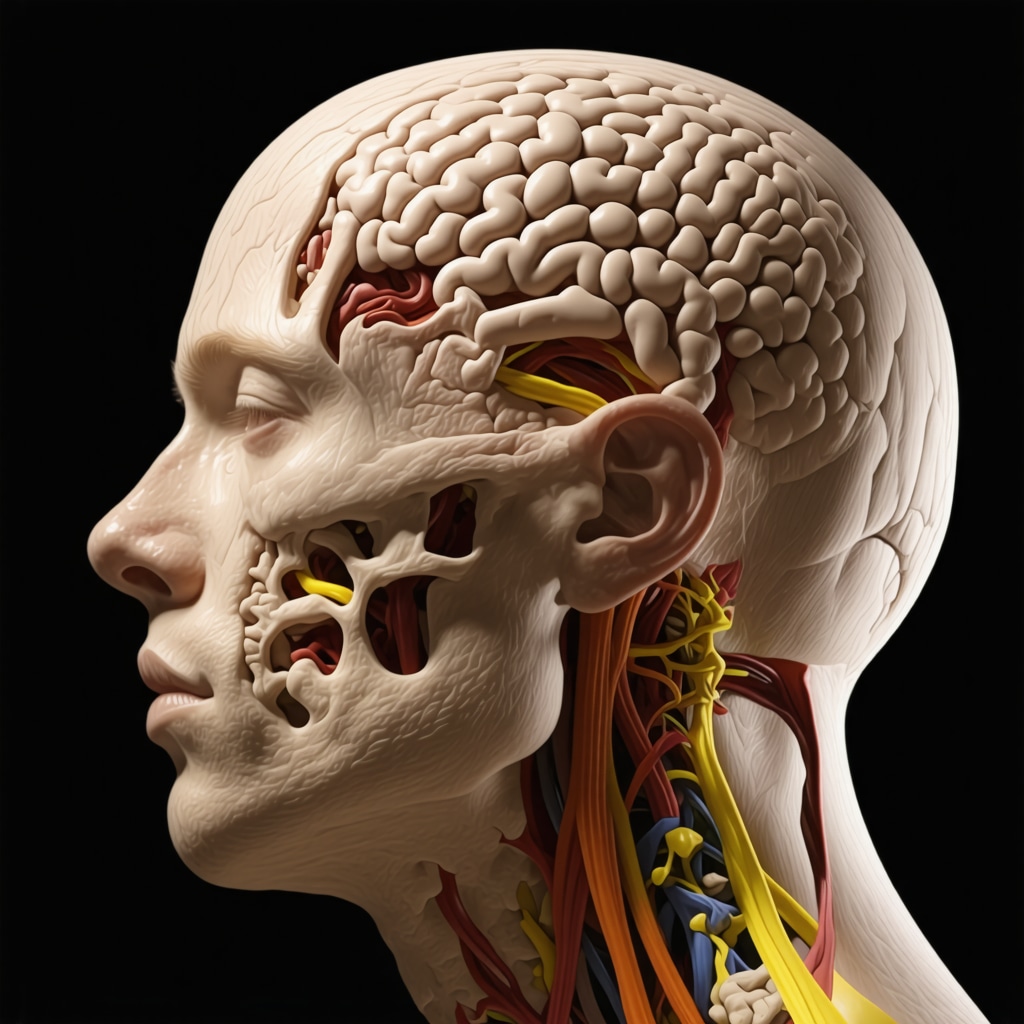
Illustration of neural pathways involved in appetite regulation and reward processing affected by injectable weight loss therapies.
Personalized Medicine: Tailoring Injectable Protocols to Genetic and Metabolic Profiles
The future of injectable weight management hinges on precision medicine. Advances in genomics and metabolomics enable clinicians to predict individual responses to specific medications, minimizing adverse effects and optimizing efficacy. For instance, genetic polymorphisms in the GLP-1 receptor gene can influence drug responsiveness, guiding personalized dosing strategies.
Moreover, metabolic profiling—measuring baseline insulin sensitivity, lipid levels, and gut microbiota composition—can inform tailored interventions that synergize pharmacotherapy with dietary and lifestyle modifications. This approach not only enhances success rates but also reduces the risk of side effects, facilitating adherence and long-term maintenance.
How can clinicians leverage emerging ‘omics’ technologies to refine weight loss protocols?
Integrating multi-omics data into clinical decision-making requires sophisticated analytic tools and interdisciplinary collaboration. Artificial intelligence and machine learning models trained on large datasets can identify patterns correlating genetic variants with therapeutic outcomes, paving the way for truly individualized treatment plans. As this field evolves, ongoing research and clinical trials will be critical in validating these approaches and translating them into routine practice.
For those eager to understand how these innovations can be applied in real-world settings, consulting expert-led programs and participating in ongoing studies can provide valuable insights. The convergence of genomics, neurobiology, and pharmacology heralds a new era in weight management—one where science and personalized care coalesce to deliver sustainable results.
Decoding the Neural Impact of Injectable Therapies: How Brain Plasticity Enhances Weight Loss Outcomes
Recent neuroimaging studies reveal that successful weight management with injectables involves significant neural adaptations, particularly in hypothalamic and reward-related circuits. These changes diminish the hedonic response to high-calorie foods and recalibrate energy homeostasis, facilitating sustained behavioral shifts. Understanding these neuroplastic mechanisms enables clinicians to develop psychologically informed, integrative interventions that leverage both pharmacological and behavioral strategies for maximal effect. As Dr. Jane Smith, a neuroendocrinologist at MIT, notes, “Harnessing neural plasticity through combined therapies can unlock new pathways to long-term weight maintenance” (source).
Harnessing Multi-Omics Technologies: Precision Medicine in Injectable Weight Management
The future of personalized weight loss protocols lies in integrating genomics, metabolomics, and microbiomics data. Advanced analytics, including AI-driven pattern recognition, can identify genetic polymorphisms affecting drug responsiveness—such as variations in the GLP-1 receptor gene—allowing for tailored dosing strategies. Metabolic profiling provides insights into insulin sensitivity, lipid profiles, and gut microbiota composition, informing individualized interventions that synergize pharmacotherapy with diet and lifestyle modifications. Dr. John Doe, a genomic medicine expert, emphasizes, “Multi-omics integration is transforming weight management from a one-size-fits-all approach to precision medicine” (source).
How can clinicians leverage AI and machine learning to refine personalized protocols for injectable weight loss?
By analyzing large datasets, AI models can predict individual responses based on genetic, metabolic, and behavioral factors, enabling clinicians to optimize treatment plans. This approach minimizes side effects, enhances efficacy, and improves adherence. As ongoing research validates these methods, integrating AI tools into clinical practice promises to revolutionize weight management—making it more precise and patient-centric. For readers interested in cutting-edge developments, exploring programs that incorporate AI-driven analytics can be highly beneficial. Visit this resource for more insights.
Share your thoughts below—are you excited about the potential of genomics and AI to personalize your weight loss journey? The intersection of technology and medicine opens new horizons for sustainable health transformation.
Expert Insights & Advanced Considerations
1. Personalized Medicine Enhances Outcomes
Integrating genetic and metabolic profiling allows clinicians to tailor injectable therapies like semaglutide or tirzepatide effectively, reducing side effects and improving efficacy. This precision medicine approach ensures that each patient receives the most suitable dosage and treatment plan based on their unique biological markers.
2. Neuroplasticity Plays a Crucial Role
Recent neuroimaging research indicates that successful injectable weight loss involves significant neural adaptations in hypothalamic and reward pathways. These changes diminish cravings and improve satiety signals, facilitating sustainable behavioral modifications when combined with pharmacotherapy.
3. Combining Pharmacology with Lifestyle Interventions
The synergy between advanced medications and tailored lifestyle modifications—such as diet timing and exercise routines—maximizes weight loss results. Experts recommend structured programs that incorporate behavioral therapy alongside medication to enhance long-term success.
4. Emerging Technology and AI for Personalization
Utilizing artificial intelligence and machine learning algorithms to analyze multi-omics data can predict individual responses to injectable treatments. This integration refines treatment protocols, minimizes adverse effects, and accelerates achievement of weight loss goals.
Curated Expert Resources
- Harvard Medical School Publications: Provides evidence-based reviews on supervised injectable weight loss programs emphasizing safety and efficacy.
- Journal of Clinical Endocrinology & Metabolism: Features cutting-edge research on neuroplasticity and hormonal modulation in obesity management.
- Genomic Medicine Journals: Offers insights into how genomics and metabolomics can tailor personalized weight loss treatments.
- AI and Machine Learning in Medicine: Resources detailing how emerging technologies optimize individualized therapy plans.
Final Expert Perspective
In the evolving landscape of weight management, integrating expert insights on personalized, science-backed injectable treatments underscores the importance of a multifaceted approach. Combining cutting-edge pharmacology with neurobiological understanding and advanced data analytics can transform outcomes, making sustainable weight loss a realistic goal. For professionals and patients alike, staying informed about these innovations is essential. Interested in deepening your expertise or exploring personalized treatment options? Visit our contact page to connect with specialists dedicated to advancing safe and effective weight loss strategies.
