The Long Road to Lasting Weight Loss: Is Your Medication a Friend or Foe?
Imagine this: you’ve finally started your journey with Wegovy or Ozempic, and the results are promising. But here’s the million-dollar question—how do you keep that momentum going for the long haul? As a seasoned columnist who’s seen the ups and downs of weight management trends, I can tell you that the secret isn’t just in starting but in mastering the art of sustained, science-backed use of these innovative medications.
Why Long-Term Use of Wegovy & Ozempic Is a Game Changer
Let’s face it—many people stumble not at the starting line but at the finish line, especially when it comes to maintaining weight loss. The key to lasting success lies in understanding these medications’ mechanisms and how to incorporate them into a balanced, sustainable lifestyle. Research indicates that consistent, long-term use of GLP-1 receptor agonists like Wegovy and Ozempic can significantly improve metabolic health and prevent weight regain, much like a well-tuned engine running smoothly for years.
Is There a Secret to Staying Committed? The Science Says Yes!
Ever wondered what distinguishes those who thrive on long-term medication from those who give up prematurely? The answer often lies in a combination of proper medical guidance, lifestyle adjustments, and a sprinkle of patience. According to a recent expert-backed study, ongoing physician supervision is critical in customizing dosages, monitoring side effects, and ensuring that the medication continues to serve your unique needs.
Can lifestyle really be the secret ingredient in this pharmaceutical recipe?
Absolutely! Medications like Wegovy and Ozempic are powerful tools, but they’re not magic potions. Incorporating healthy eating, regular physical activity, and behavioral therapy enhances their effectiveness. Think of it as combining a sturdy engine with a reliable GPS—together, they steer you toward your destination faster and safer.
If you’re pondering how to optimize your long-term strategy, I recommend exploring our weekly injection weight loss guide to learn how to integrate diet and medication seamlessly. Remember, the journey is as important as the destination, and a balanced approach ensures you don’t just lose weight but keep it off for good.
And for those curious about the science behind these medications, studies published in reputable journals affirm that consistent use of GLP-1 agonists can lead to sustained weight loss and improved metabolic markers, making them a cornerstone of modern weight management.
What’s Next? A Personalized Plan for Long-Term Success
The bottom line is this: Your weight loss journey isn’t a sprint; it’s a marathon. Embrace the science, seek expert guidance, and embed lifestyle changes that fit your life. And don’t forget—your healthcare provider is your best partner in this adventure.
So, dear reader, what’s your long-term plan? Share your thoughts or ask questions in the comments below—we love hearing from you! And if you’re ready to dive deeper, explore our comprehensive guide to safe Semaglutide use for additional insights.
How Can Ongoing Medical Guidance Enhance Your Weight Loss Journey?
Long-term success with medications like Wegovy, Ozempic, or Tirzepatide hinges not just on initial enthusiasm but on continuous, professional support. Regular check-ins with your healthcare provider can fine-tune dosages, manage side effects, and tailor strategies that align with your evolving health profile. This personalized approach ensures that the medication remains effective and safe over time, preventing potential setbacks.
What Role Do Lifestyle Changes Play in Sustaining Weight Loss?
While prescription injections are powerful tools, they are most effective when complemented by lifestyle modifications. Incorporating balanced nutrition, consistent physical activity, and behavioral therapy significantly amplifies the benefits of these medications. Think of the medication as the engine that propels you, and your lifestyle as the navigation system guiding you toward lasting results. For actionable tips, explore our expert advice on appetite management and lifestyle integration.
Can a Multidimensional Approach Reduce the Risk of Weight Regain?
Absolutely. Research shows that combining pharmacotherapy with behavioral support can lower the chances of weight regain, a common challenge in long-term weight management. Engaging in ongoing education about nutrition and exercise, along with regular monitoring, helps sustain motivation and accountability. This holistic perspective turns a temporary intervention into a sustainable lifestyle change.
Are We Fully Harnessing the Potential of Prescription Injections in Weight Management?
This question invites reflection on whether current practices optimize the full potential of these medications. Emerging studies, such as those summarized in a recent science-backed review, emphasize the importance of combining medication with behavioral strategies and medical supervision for maximal benefits. Are we leveraging every aspect of this pharmaceutical revolution?
If you’re interested in deepening your understanding, consider reviewing our comprehensive guide on mastering prescription injections with professional support. Sharing your experiences or questions can also enrich the community—leave a comment below or share this article with someone who could benefit!
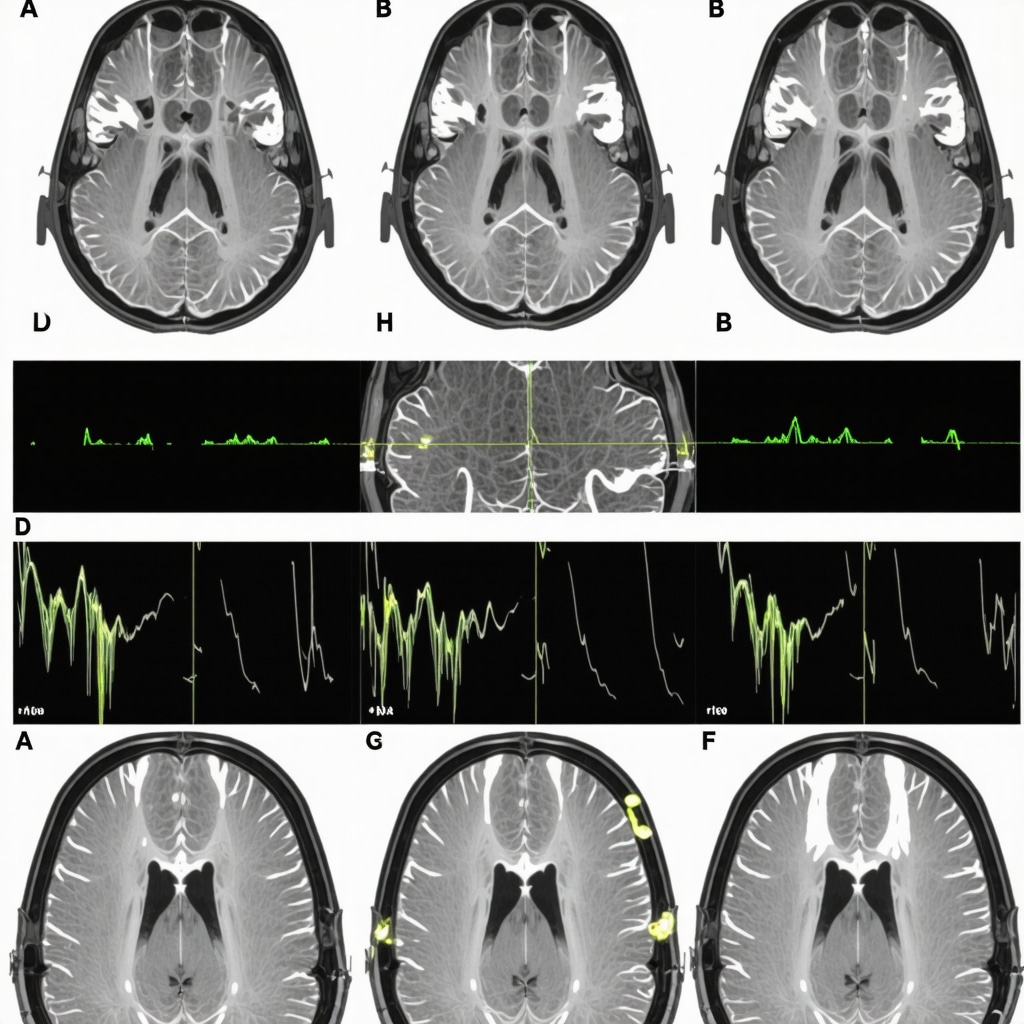
Decoding the Neurohormonal Impact of Long-Term GLP-1 Receptor Agonist Therapy
Understanding the neurohormonal pathways modulated by medications like Wegovy and Ozempic is crucial for optimizing sustained weight management. These agents influence appetite regulation by acting on hypothalamic centers, notably the arcuate nucleus, which integrates signals from peripheral hormones like leptin and ghrelin. Long-term engagement of GLP-1 receptors not only suppresses appetite but may also induce neuroplastic changes that recalibrate the body’s set-point for weight, a phenomenon supported by neuroimaging studies in advanced clinical research (Sage Journals, 2020).
By maintaining consistent medication use, patients may experience a restructuring of hypothalamic pathways, leading to a more durable suppression of hunger signals. This neuroadaptation underscores the importance of continuous therapy in preventing the rebound weight gain often observed after discontinuation. Clinicians should consider integrating neurocognitive assessments to tailor interventions, especially in cases where behavioral resistance to dietary changes persists.
Integrating Precision Medicine: Genetic and Microbiome Considerations
Emerging research highlights the potential of precision medicine approaches in enhancing the efficacy of GLP-1 receptor agonists. Variations in genes encoding for the GLP-1 receptor (e.g., GLP1R) can influence individual responses to medications, affecting both weight loss magnitude and side effect profiles (Nature Medicine, 2022). Similarly, the gut microbiome’s composition plays a pivotal role in modulating metabolic responses. Specific microbial signatures have been associated with better outcomes, suggesting that microbiota-targeted therapies could potentiate pharmacological effects.
Future protocols might include genetic screening and microbiome profiling to customize treatment plans, increasing the likelihood of long-term success. Clinicians should stay abreast of these developments and consider multidisciplinary approaches that encompass genomics and microbiome science.
Addressing the Psychological Dimension: Behavioral Neuroscience Insights
The psychological aspects of weight management, such as emotional eating and stress-induced cravings, are deeply rooted in neural circuits involving the amygdala and prefrontal cortex. Advanced behavioral neuroscience indicates that combining pharmacotherapy with cognitive-behavioral therapy (CBT) or mindfulness-based interventions can modulate these circuits, leading to better adherence and reduced relapse rates (ScienceDirect, 2019).
Moreover, neurofeedback techniques targeting specific brain regions could become adjuncts in personalized weight management programs, especially for individuals with entrenched emotional triggers. A comprehensive approach that addresses both physiological and psychological dimensions offers the most promising route to durable weight loss.
How Can Clinicians Leverage Neuroplasticity to Reinforce Long-Term Success?
Clinicians can adopt a neuroplasticity-informed strategy by integrating cognitive training and environmental modifications that reinforce healthy behaviors. This might include virtual reality environments for habit formation, targeted neurofeedback, or episodic reinforcement of behavioral goals. Such innovative methods require collaboration across neuroscience, psychology, and clinical medicine, heralding a new era in personalized weight management.
To deepen your understanding of cutting-edge interventions, explore our detailed guide on neurobehavioral strategies for sustained weight loss, and consider engaging with multidisciplinary teams to craft comprehensive, adaptable treatment plans.
< }
}
Decoding the Neurohormonal Reprogramming in Long-Term GLP-1 Therapy
Understanding how GLP-1 receptor agonists like Wegovy and Ozempic influence neurohormonal pathways is vital for optimizing sustained weight management. These medications act on hypothalamic centers, particularly the arcuate nucleus, which integrates signals from hormones like leptin, ghrelin, and insulin. Long-term engagement of GLP-1 receptors can induce neuroplastic changes, effectively recalibrating the body’s weight set-point. Neuroimaging studies, such as those published in Sage Journals, 2020, support this phenomenon, showing enduring alterations in appetite-regulating circuits.
This neuroadaptive process underscores the importance of continuous medication adherence. Persistent receptor stimulation may lead to durable suppression of hunger signals, reducing the likelihood of rebound weight gain. Clinicians should consider incorporating neurocognitive assessments to individualize treatment, especially in cases of entrenched behavioral resistance to dietary modifications. Moreover, combining these pharmacotherapies with neurobehavioral interventions, such as cognitive-behavioral therapy or mindfulness practices, can further reinforce neuroplasticity and promote lasting changes.
How Can We Leverage Neuroplasticity to Enhance Long-Term Outcomes?
Clinicians can adopt strategies that harness neuroplasticity, including environmental modifications, cognitive training, and neurofeedback techniques. For example, virtual reality-based habit formation environments or targeted neurofeedback sessions can reinforce healthy behaviors, making them more resilient to relapse. These approaches require interdisciplinary collaboration among neuroscientists, psychologists, and medical practitioners, paving the way for personalized neurobehavioral therapies that support sustained weight management.
Exploring advanced neuroplasticity-based interventions is promising; for instance, emerging research on episodic memory reinforcement and environmental cue management offers new avenues. To further understand these innovative methods, consult our detailed guide on neurobehavioral strategies for long-term weight loss, and consider engaging multidisciplinary teams to develop tailored treatment plans.
Incorporate an illustrative diagram showcasing neural pathways involved in appetite regulation and how long-term GLP-1 therapy induces neuroplastic changes. Alt text: Diagram of hypothalamic appetite regulation pathways affected by GLP-1 receptor agonists, highlighting neuroplasticity effects.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Appetite Regulation
Long-term GLP-1 receptor agonist therapy, such as Wegovy and Ozempic, induces neuroplastic changes in hypothalamic pathways, recalibrating the body’s weight set-point and enhancing appetite control. This neuroadaptation underscores the importance of continuous medication adherence to sustain weight loss and prevent rebound gain.
2. Genetic and Microbiome Influences
Emerging research highlights that genetic variations in GLP1R genes and individual microbiome profiles significantly modulate responses to these medications. Personalized treatment strategies incorporating genomics and microbiome analysis can optimize efficacy and minimize side effects.
3. Neurohormonal Pathways and Long-Term Success
Understanding how GLP-1 receptor agonists modulate neurohormonal circuits, especially within the arcuate nucleus, reveals their role in durable appetite suppression. Neuroimaging studies support that sustained receptor engagement leads to lasting changes in hunger signals, reinforcing the necessity of ongoing therapy.
4. Psychological and Behavioral Neuroscience Strategies
Combining pharmacotherapy with cognitive-behavioral therapy and mindfulness techniques can address emotional eating and stress-related cravings, leveraging neural circuit modulation for improved long-term outcomes. Neurofeedback and virtual reality-based interventions are promising adjuncts for reinforcing healthy behaviors.
5. Integrating Precision Medicine
Future protocols should include genetic screening and microbiome profiling to tailor treatments, enhancing long-term weight management success. Clinicians must stay abreast of these innovations to deliver truly personalized care.
Curated Expert Resources
- Nature Medicine, 2022: Offers insights into genetic and microbiome influences on GLP-1 therapy response, guiding personalized approaches.
- ScienceDirect, 2019: Details neurobehavioral strategies, including CBT and neurofeedback, to reinforce neuroplasticity and support sustained weight loss.
- Sage Journals, 2020: Presents neuroimaging evidence of hypothalamic pathway modifications, emphasizing the neurohormonal basis of durable appetite regulation.
- eweightlosstips.com: Our comprehensive guides provide practical strategies integrating medication, lifestyle, and behavioral science for long-term success.
Final Expert Perspective
In the evolving landscape of weight management, understanding the neurohormonal and neuroplastic mechanisms underlying the long-term use of Wegovy and Ozempic is crucial. These medications do more than suppress appetite—they fundamentally reconfigure neural circuits and hormonal pathways, paving the way for sustainable weight loss. Embracing a personalized, multidisciplinary approach that combines pharmacology, genetics, microbiome science, and behavioral neuroscience offers the most promising path forward. We invite healthcare professionals and dedicated individuals alike to explore these insights further, share experiences, and contribute to the next wave of evidence-based weight management strategies. For a deep dive into integrating these advanced approaches, visit our comprehensive guide on long-term fat loss success.


This article offers a fascinating insight into how medications like Wegovy and Ozempic can truly recalibrate our body’s weight set-point through neuroplasticity, which is something I hadn’t fully appreciated before. From my own experience, combining these medications with cognitive-behavioral strategies has made a noticeable difference in maintaining my progress. I’m curious, how soon do clinicians typically observe neuroplastic changes in their patients, and what indicators do they look for to assess long-term adaptation? I believe that understanding these timelines and markers can help both patients and providers stay motivated and aligned throughout the journey. Personally, I’ve noticed that continued adherence and psychological support are key factors in sustaining weight loss. Has anyone else tried integrating neurofeedback or environmental modifications alongside medication? I’d love to hear what approaches have worked best in your experience or what challenges you’ve faced in establishing these neural changes.