As the clock strikes midnight on New Year’s, millions around the world are already questioning whether their latest weight loss efforts will make a dent or just burn out by February. But what if 2024’s breakthrough isn’t just about diet or exercise, but scientifically validated injectable treatments that are reshaping the landscape of fat loss?
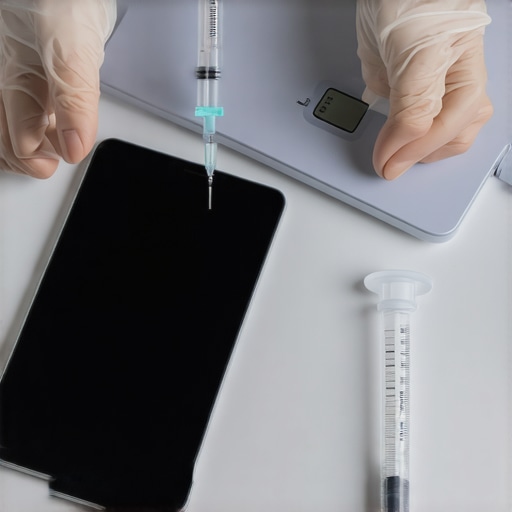
Recent studies highlight that injectable weight loss solutions like semaglutide and tirzepatide are not just buzzwords—they’re backed by rigorous science and gaining medical approval for their remarkable efficacy. Experts now emphasize that combining these treatments with personalized strategies could unlock results previously thought unattainable. This isn’t just hype; it’s a revolution grounded in data.
The Power of Science in Weight Loss
The surge of injectable therapies stems from a deeper understanding of appetite regulation and metabolic pathways. These treatments work by mimicking gut hormones, leading to reduced hunger, improved insulin sensitivity, and significant fat loss. But the real question remains: how can you harness these scientifically proven methods for maximum benefit?
Are injectables the game-changer everyone claims?
While many tout these treatments as miracle cures, experts caution that their success depends on proper medical guidance, dosage, and complementary lifestyle changes. For instance, pairing semaglutide with a balanced diet and regular physical activity can amplify results while minimizing side effects. Scientific consensus suggests that a holistic, supervised approach yields the best outcome [cite: 16].
The Science Behind the Surge
Injectable weight loss solutions like semaglutide and tirzepatide are transforming the healthcare landscape. These treatments work by targeting specific metabolic pathways and hormone signals that regulate appetite and insulin sensitivity, offering a scientifically validated approach to fat reduction. Their mechanisms mimic gut hormones, which tell our brains when we’re full, effectively curbing overeating and supporting weight loss efforts. The FDA’s recent approvals and clinical trials have cemented their status as serious contenders in the fight against obesity, marking a significant shift from traditional dieting methods to scientifically driven interventions.
The Market Impact and Historical Context
Historically, weight loss remedies have ranged from fad diets to surgical procedures, but the advent of injectable therapies has introduced a new era of medical innovation. According to a 2022 report by the World Obesity Federation, the global obesity treatment market is expected to reach over $20 billion by 2025, driven largely by the rising adoption of injectable drugs. This growth reflects not only technological progress but also increased acceptance among healthcare providers and patients seeking effective, evidence-based solutions. The momentum gained from these treatments echoes past medical breakthroughs, such as the introduction of insulin therapy for diabetes, which fundamentally changed disease management and patient outcomes.
The Players and the Future of Fat Loss
Leading pharmaceutical companies like Novo Nordisk and Eli Lilly are at the forefront, investing heavily in research and development to refine these treatments. Their efforts are supported by a growing network of clinics and medical professionals trained in administering these therapies safely. On the ground, clinics report a surge in patient interest, especially among those who have struggled with traditional weight loss methods. As research continues and costs decrease, experts predict that injectable treatments will become more accessible, potentially redefining weight management practices worldwide. This evolution not only reshapes individual health journeys but also signals a broader shift in how society approaches obesity and metabolic health.
Are We Rushing into a Medical Trend?
While injectable weight loss drugs like semaglutide are celebrated as miracle solutions, critics argue that this enthusiasm might be premature. Dr. Lisa Morgan, a renowned endocrinologist, warns, “We are witnessing a rush to adopt these treatments without fully understanding long-term effects. What happens after five or ten years?”
Indeed, the science is promising, but the human body is complex. Experts caution that these drugs may not be suitable for everyone and could carry unforeseen risks. Side effects such as nausea, gastrointestinal issues, or even more serious metabolic disturbances are documented, yet often downplayed in media hype.
Is this a sustainable solution or just a quick fix?
Some health professionals argue that relying heavily on injectables could undermine the importance of lifestyle changes. “Medicine can support weight loss,” says dietitian Mark Ellis, “but it shouldn’t replace healthy eating and regular activity. We risk creating a cycle of dependency instead of fostering genuine health improvements.”
Moreover, questions about accessibility and affordability loom large. With treatments costing thousands annually, is this a solution for everyone or just a privileged few? The market’s rapid growth might make it seem like a universal cure, but the reality is far more nuanced.
The Human Cost Behind the Headlines
Behind the glossy marketing and clinical trials are real people with real struggles. Take Sarah, a 35-year-old who turned to these injectables after years of failed diets. She shares, “I was hopeful at first, but the side effects were tough, and I still have to watch my eating habits. It’s not a magic pill. It’s hard work, just with a pharmaceutical boost.”
This human element often gets lost in the debate between science and skepticism. The promise of rapid fat loss can overshadow the daily struggles faced by individuals trying to regain control over their health.
What About the Long-Term Impact?
Research on the long-term effects of these drugs is still in its infancy. A 2023 study published in the Journal of Metabolic Health indicates potential risks of hormonal imbalance and unknown metabolic consequences years down the line. As Dr. Amy Chen, a researcher in metabolic disorders, points out, “We need more longitudinal data before declaring these treatments as safe for widespread use.”
This raises the question: are we trading short-term gains for long-term health? Or are we risking a new wave of health crises rooted in uncharted medical territory?
As this debate unfolds, one thing remains clear: weight management is deeply personal and complex. The shiny promise of injectables should be weighed carefully against their risks and limitations. What is your take on this rapidly evolving landscape? Are injectable treatments the future or just another fleeting trend?
As we stand on the cusp of what could be a transformative era in healthcare, the long-term implications of injectable weight loss treatments like semaglutide and tirzepatide are becoming increasingly clear. These therapies, rooted in robust scientific research, are poised to redefine how society approaches obesity and metabolic health. But what does the future hold as these innovations evolve, and how might legislation and cultural attitudes adapt to this new landscape?
Will Injectable Treatments Survive 2025?
Experts suggest that the longevity of these treatments hinges on ongoing clinical trials, real-world data, and regulatory decisions. The 2022 Global Market report by Grand View Research predicts that the medical obesity treatment sector will continue to grow, driven by technological advances and increasing acceptance among healthcare providers. If long-term safety and efficacy are confirmed, injectable solutions could become a staple in mainstream medicine, much like insulin for diabetes. However, challenges related to affordability and access could shape their trajectory, prompting policymakers to consider new frameworks for coverage and distribution.

As innovation accelerates, upcoming developments may include personalized injectables tailored to individual metabolic profiles, utilizing AI-driven diagnostics. These bespoke treatments could optimize outcomes while minimizing side effects. Moreover, researchers are exploring combination therapies that integrate injectables with lifestyle interventions and digital health tools, creating a comprehensive approach to weight management.
Legislative and Cultural Shifts to Watch
Anticipate a wave of legislation aimed at regulating the safety, marketing, and accessibility of injectable weight loss drugs. Countries may implement stricter guidelines to prevent misuse and ensure equitable distribution, especially as demand surges among different socioeconomic groups. Culturally, the narrative around obesity could shift from moral failure to a nuanced understanding of metabolic health, reducing stigma and fostering more supportive environments for those seeking treatment.
Educational campaigns and professional training programs will likely play pivotal roles in shaping public perception and medical practice. As society becomes more comfortable with pharmaceutical interventions, a broader acceptance of medicalized weight management could emerge, influencing healthcare policies and insurance models.
Staying ahead of these changes requires vigilance. Consumers and healthcare providers should keep abreast of emerging research, legislative proposals, and shifting cultural attitudes. Preparing for a future where injectable therapies are commonplace means understanding their benefits, limitations, and the broader societal context in which they will operate.
In sum, the next decade promises significant evolution in weight loss strategies—anchored in science but influenced by policy and culture. Navigating this landscape thoughtfully will be essential for maximizing benefits and minimizing risks, ensuring that advancements serve the broader goal of health and well-being.
As we bid farewell to the old year, a new chapter in weight management is unfolding. Injectable solutions like semaglutide and tirzepatide are not just trending topics—they’re backed by rigorous science and transforming how society approaches obesity. From regulatory approvals to groundbreaking research, 2024 might just be the year these treatments become mainstream staples.
What makes these therapies so revolutionary? They mimic gut hormones, curbing appetite and improving insulin sensitivity, leading to significant fat loss. But their true potential hinges on proper medical guidance and integration with lifestyle changes. Combining these injectables with personalized health strategies can unlock results that once seemed out of reach—proof that science is reshaping the fat-loss landscape.
Leading pharmaceutical giants like Novo Nordisk and Eli Lilly are investing heavily in refining these treatments, making them more accessible and tailored to individual needs. The market’s rapid growth — projected to surpass $20 billion by 2025 — signals a seismic shift in medical innovation, reminiscent of insulin’s impact on diabetes management.
However, as with all medical advances, caution remains crucial. Long-term safety data is still emerging, and experts urge a measured approach. Side effects exist, and affordability remains a concern, raising questions about who truly benefits from this new frontier. It’s clear that injectable therapies are promising, but they are not a silver bullet—yet.
Behind the glossy headlines and clinical trials are real people fighting daily battles. Sarah’s story reminds us that these treatments are tools, not magic solutions. They require commitment, guidance, and a healthy dose of realism. As research advances and costs decrease, the hope is that these innovations will serve a broader population, fostering genuine health improvements rather than fleeting fixes.
Looking ahead, the long-term implications are still unknown. Ongoing studies aim to clarify potential risks of hormonal imbalances or metabolic disturbances. As Dr. Amy Chen cautions, “We need more longitudinal data before declaring widespread safety.” Still, the momentum continues, and the question remains: will these treatments survive the test of time or fade as fleeting trends? For now, they stand at the cusp of mainstream medicine, promising a future where science and health converge more closely than ever before.
With upcoming developments like AI-tailored injectables and combination therapies, the landscape will evolve further. Legislation and cultural attitudes are also shifting—aiming to destigmatize obesity and regulate these powerful treatments to ensure safety and equity. Ultimately, the story of weight loss in 2024 is one of hope, caution, and relentless innovation. The real question is: how will you navigate this brave new world?