Understanding the Intricacies of Semaglutide Injection Site Reactions
Semaglutide, a GLP-1 receptor agonist, has become a cornerstone in obesity management and type 2 diabetes treatment due to its efficacy in appetite regulation and glycemic control. However, despite its clinical benefits, injection site reactions remain a persistent challenge that can undermine patient adherence and therapeutic outcomes. These reactions include localized erythema, pain, swelling, and, in rarer cases, injection site infections. Addressing these effectively requires a nuanced understanding of the pharmacodynamics of semaglutide administration and patient-specific factors affecting tissue response.
Advanced Techniques to Mitigate Injection Site Adverse Effects
Optimizing Injection Site Rotation and Depth to Minimize Tissue Trauma
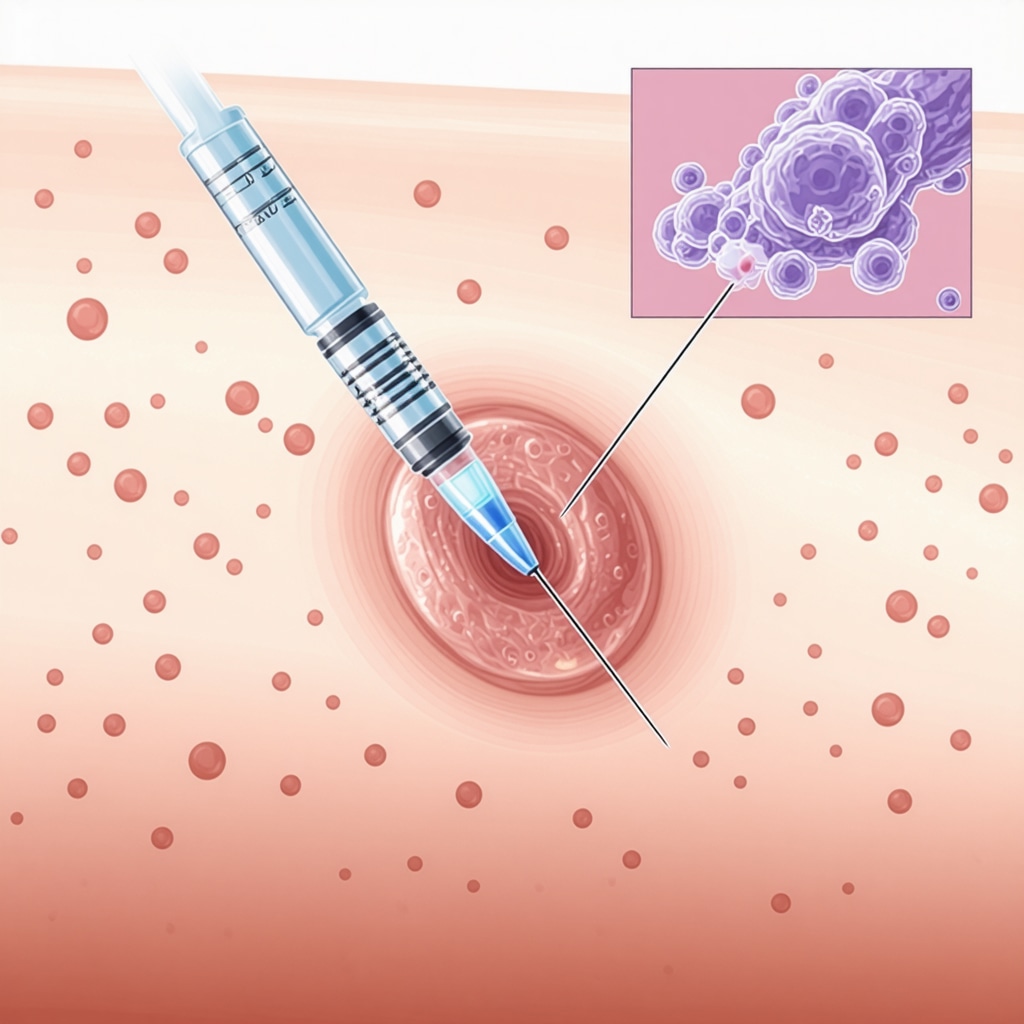
One of the foremost approaches to reducing injection site reactions is systematic rotation of injection sites. Repeated administration in the same anatomical location leads to lipohypertrophy or localized inflammation, compromising drug absorption and patient comfort. Employing precise subcutaneous injection techniques, typically at a 45 to 90-degree angle depending on needle length and patient adiposity, can minimize tissue trauma. Current guidelines advocate rotating among the abdomen, thigh, and upper arm areas to preserve skin integrity and reduce cumulative irritation.
What Are the Best Practices for Managing Persistent Injection Site Reactions in Semaglutide Therapy?
For patients experiencing prolonged or severe injection site reactions, clinical assessment should rule out hypersensitivity or infection. Topical corticosteroids or cold compresses can alleviate inflammation, while ensuring aseptic technique during injection reduces infection risk. In some cases, consultation with healthcare providers to adjust dosage or explore alternative formulations is warranted. Patient education on needle disposal and skin care post-injection is equally vital to prevent complications.
Integrating Patient-Centric Protocols for Safer Semaglutide Use
Empowering patients with knowledge about proper needle handling, storage, and timing of injections enhances both safety and efficacy. For example, storing semaglutide pens under recommended refrigeration conditions preserves medication potency and reduces the risk of irritation due to degraded compounds. Encouraging patients to report side effects promptly facilitates timely interventions and personalized treatment adjustments. These strategies align with expert recommendations detailed in comprehensive guides on managing injection site reactions.
Leveraging Evidence-Based Insights to Elevate Injection Safety
Emerging research underscores the role of injection technique education in improving patient outcomes. A study published in the Journal of Diabetes Science and Technology highlights that structured training programs significantly reduce the incidence of injection site complications. This emphasizes the value of integrating multidisciplinary support and continuous patient engagement into clinical practice to foster adherence and mitigate adverse reactions effectively.
Explore More Expert-Level Strategies on Safe Semaglutide Use
For healthcare professionals and patients seeking to deepen their understanding of semaglutide administration, exploring detailed protocols on avoiding common injection errors and best practices for new users can provide invaluable insights. Engaging with these resources fosters a comprehensive approach to maximizing therapeutic benefits while minimizing discomfort and risks.
Innovative Approaches to Injection Site Care for Semaglutide Users
Beyond basic rotation and aseptic techniques, incorporating adjunctive skin care regimens can significantly reduce injection site complications. Utilizing barrier creams or emollients post-injection may soothe irritated skin and prevent dryness, which often exacerbates discomfort. Additionally, pre-injection skin preparation with gentle cleansing agents rather than harsh antiseptics minimizes skin barrier disruption, thereby reducing inflammatory responses.
Understanding Immunological Responses in Injection Site Reactions
Injection site reactions are not solely mechanical; immunological factors play a critical role. Some patients develop delayed hypersensitivity reactions characterized by persistent erythema and induration due to immune-mediated inflammation against the peptide or excipients. Recognizing these immunopathologies is vital for clinicians to tailor treatment plans appropriately, potentially involving temporary cessation of therapy or switching to alternative agents.
How Can Personalized Injection Protocols Optimize Outcomes and Minimize Adverse Effects?
Personalized medicine principles are increasingly relevant in managing semaglutide therapy. Variables such as patient skin type, adiposity, and previous history of injection reactions inform customized injection schedules and sites. For instance, patients with thinner subcutaneous tissue may benefit from shorter needles or adjusted injection angles. Employing patient-reported outcomes and digital tracking tools supports dynamic protocol adjustments, enhancing safety and efficacy over time.
Leveraging Technology to Support Safe and Effective Semaglutide Administration
Digital health platforms and smart injection devices are emerging tools that provide real-time feedback on injection technique, site rotation, and adherence patterns. These innovations empower both patients and providers to identify early signs of adverse reactions and intervene promptly. Integrating such technologies aligns with expert recommendations to reduce injection-related complications and optimize therapeutic benefit, as supported by recent clinical trials published in Diabetes Therapy.
Collaborative Care Models for Enhancing Patient Education and Support
Multidisciplinary approaches involving endocrinologists, diabetes educators, and pharmacists foster comprehensive patient education on injection techniques and side effect management. Regular follow-ups and support groups facilitate knowledge sharing and emotional support, crucial for maintaining long-term adherence. More detailed strategies on combining education with clinical oversight can be found in our guide on supervised injectable weight loss balancing safety and results.
Join the Discussion: What Are Your Experiences with Managing Injection Site Reactions in Semaglutide Therapy?
We invite healthcare professionals and patients alike to share insights, challenges, and effective solutions regarding semaglutide injection site management. Your contributions help build a collective knowledge base that benefits the entire community.
Deciphering the Complex Immunopathogenesis Behind Semaglutide Injection Site Reactions
Injection site reactions (ISRs) in semaglutide therapy extend beyond mere physical trauma and involve intricate immune mechanisms. Emerging evidence suggests that the peptide nature of semaglutide, coupled with its excipients, can trigger localized immune responses ranging from immediate hypersensitivity to delayed-type reactions. These immunological responses manifest as persistent erythema, induration, or even granulomatous inflammation, complicating clinical management. Understanding these pathophysiological processes demands a detailed examination of antigen presentation, T-cell activation, and cytokine milieu alterations at the injection site.
Recent histopathological analyses reveal infiltration of immune effector cells such as macrophages and lymphocytes, highlighting an adaptive immune component that may contribute to chronic local inflammation. Clinicians need to balance continuing therapy against the risk of exacerbating immune-mediated tissue damage, often necessitating skin biopsies and immunological assays to delineate the underlying reaction type accurately.
How Can Immunomodulatory Interventions Be Tailored to Address Persistent Semaglutide Injection Site Reactions?
Targeted immunomodulatory therapies offer promising avenues for managing refractory ISRs. Topical calcineurin inhibitors, for example, can modulate T-cell activity locally without systemic immunosuppression, reducing inflammation and mitigating hypersensitivity. In select cases, short courses of systemic corticosteroids or antihistamines might be warranted, but these require careful risk-benefit analysis due to potential side effects affecting glycemic control. Personalized immunotherapy strategies, informed by immunophenotyping and patient-specific factors, represent the frontier of ISR management.
Harnessing Pharmacogenomics to Personalize Semaglutide Administration and Reduce ISRs
Pharmacogenomics—the study of how genes affect a person’s response to drugs—holds transformative potential for optimizing semaglutide therapy. Genetic polymorphisms influencing immune response, skin barrier function, and drug metabolism can predispose individuals to heightened ISR risk. For instance, variants in cytokine genes like TNF-α or IL-6 may amplify local inflammatory cascades post-injection, while mutations affecting skin integrity can exacerbate irritation.
Incorporating pharmacogenetic screening into clinical protocols could enable healthcare providers to stratify patients by ISR risk and customize dosing regimens or needle selection accordingly. This precision medicine approach not only enhances safety but also preserves therapeutic efficacy by reducing premature discontinuation caused by adverse reactions.
Innovations in Injection Device Engineering: Minimizing Tissue Trauma and Immunogenicity
Technological advancements in injection devices have begun to address the mechanical and immunological challenges of semaglutide administration. Needle design improvements—such as ultra-thin, coated needles—reduce penetration force and tissue damage, consequently lowering ISR incidence. Moreover, smart injection pens equipped with sensors can monitor injection depth, angle, and site rotation, providing real-time feedback to patients and clinicians.
Emerging drug delivery systems, including microneedle patches and implantable depots, are under investigation to bypass traditional injection hurdles. These innovations aim to deliver semaglutide with minimal disruption to skin integrity and immune activation, representing a paradigm shift in management.
What Role Does Advanced Patient Monitoring Play in Early Detection and Management of Semaglutide Injection Site Reactions?
Continuous patient monitoring through digital health platforms enables early identification of ISR symptoms, facilitating prompt intervention before complications escalate. Wearable devices and mobile health apps can track patient-reported outcomes, skin changes via photographic documentation, and adherence patterns. This data integration supports proactive clinical decision-making, optimizing treatment continuity and patient quality of life.
According to a controlled trial published in Diabetes Care, implementation of remote monitoring significantly reduced ISR-related discontinuations by enabling timely adjustments in injection technique and supportive care.
Clinicians and patients are encouraged to explore these sophisticated monitoring tools as adjuncts to traditional care protocols to enhance overall semaglutide therapy outcomes.
Delving Deeper into Immunological Nuances of Semaglutide ISRs
Beyond the conventional understanding of semaglutide injection site reactions (ISRs), recent immunological insights reveal a layered complexity involving innate and adaptive immune mechanisms. The peptide structure of semaglutide can act as a neoantigen, eliciting a spectrum of local immune responses. These range from immediate IgE-mediated hypersensitivity to Type IV delayed-type hypersensitivity, often mediated by T-helper 1 cells and macrophage activation, which contribute to persistent erythema and granuloma formation. Recognizing these immunopathogenic pathways allows clinicians to anticipate and differentiate between transient mechanical irritation and chronic immune-mediated reactions, enabling more precise therapeutic interventions.
Emerging Immunomodulatory Therapies: Precision Interventions for Refractory ISRs
Can Targeted Immunomodulation Revolutionize Management of Persistent Semaglutide Injection Site Reactions?
Targeted immunomodulatory interventions represent a promising frontier for patients with refractory ISRs. Topical calcineurin inhibitors, such as tacrolimus and pimecrolimus, offer local T-cell suppression without systemic immunosuppression, thereby minimizing side effects while attenuating inflammation. Additionally, emerging biologic agents targeting cytokines like tumor necrosis factor-alpha (TNF-α) or interleukin-6 (IL-6) are under investigation for severe immune-mediated ISRs. Such treatments demand precise immunophenotyping and risk stratification, underscoring the necessity of personalized medicine approaches in managing complex ISR cases effectively.
Pharmacogenomics and Personalized Medicine: Tailoring Semaglutide Therapy to Genetic Profiles
Integrating pharmacogenomic data into clinical protocols offers a transformative pathway to optimize semaglutide administration and minimize ISRs. Polymorphisms in genes encoding cytokines (e.g., TNF-α, IL-6), human leukocyte antigen (HLA) haplotypes, and skin barrier proteins like filaggrin have been correlated with differential ISR susceptibility. For instance, patients harboring alleles linked to heightened pro-inflammatory responses may require adjusted dosing schedules or preemptive topical immunomodulation. This genomic stratification facilitates precision dosing and needle selection, ultimately enhancing tolerability and adherence while preserving semaglutide’s therapeutic efficacy.
Innovations in Injection Device Technology: Engineering Solutions to Mitigate Tissue and Immunological Trauma
Recent advancements in injection device engineering aim to harmonize mechanical optimization with immunological safety. Ultra-fine, coated needles reduce tissue penetration force, thereby limiting microtrauma and subsequent inflammatory cascades. Smart injection pens equipped with integrated sensors and AI algorithms provide real-time feedback on injection angle, depth, speed, and site rotation adherence, empowering patients and clinicians alike. Moreover, experimental delivery platforms such as dissolvable microneedle arrays and implantable depots are being developed to circumvent traditional subcutaneous injections, minimizing both physical trauma and immune activation risks.

Leveraging Digital Health for Proactive ISR Surveillance and Personalized Care
Advanced digital health tools, including wearable biosensors and mobile applications, enable continuous monitoring of injection sites through photographic documentation and symptom tracking. These technologies facilitate early detection of ISR onset, allowing for timely modification of injection techniques or therapeutic regimens. A controlled trial published in Diabetes Care demonstrated that integrating remote monitoring protocols significantly decreased ISR-related therapy discontinuations by enabling proactive interventions. The convergence of digital health with personalized care models heralds a new era in optimizing semaglutide treatment outcomes.
Multidisciplinary Collaborative Models: Enhancing Education, Support, and Clinical Oversight
Comprehensive management of semaglutide ISRs necessitates multidisciplinary collaboration involving endocrinologists, dermatologists, diabetes educators, and pharmacists. Structured education programs focusing on injection technique refinement, skin care protocols, and early symptom recognition are pivotal. Regular follow-ups and peer support groups foster adherence and emotional resilience, mitigating the psychosocial burden of chronic therapy. Detailed frameworks for such collaborative care are elaborated in expert resources like supervised injectable weight loss balancing safety and results, enabling healthcare providers to deliver holistic, patient-centered care.
Engage with Us: Share Your Advanced Insights on Semaglutide Injection Site Management
We encourage clinicians, researchers, and patients to contribute their expert experiences and innovative strategies for managing semaglutide ISRs. Your participation enriches the collective understanding and drives forward evidence-based practices to optimize safety and efficacy in semaglutide therapy.
Expert Insights & Advanced Considerations
Immunological Profiling Enhances Personalized ISR Management
Recognizing the immunopathogenic complexity of semaglutide injection site reactions (ISRs) enables clinicians to tailor interventions beyond symptomatic treatment. Detailed immunological profiling—such as skin biopsies and cytokine assays—can identify specific hypersensitivity types, facilitating targeted immunomodulatory therapies that improve patient tolerance without compromising glycemic control.
Pharmacogenomic Screening as a Predictive Tool for Injection Site Tolerability
Integrating pharmacogenomic markers related to inflammatory response and skin barrier integrity into patient evaluation protocols promises to stratify ISR risk effectively. Such precision medicine approaches allow customization of injection regimens, needle selection, and preemptive treatments, thereby reducing adverse reaction incidence and enhancing semaglutide adherence.
Innovative Injection Devices Are Revolutionizing Administration Safety
The advent of ultra-thin, coated needles and smart injection pens with real-time feedback mechanisms significantly mitigates tissue trauma and immune activation. These technological advances empower patients with precision dosing and site rotation guidance, minimizing ISRs and optimizing therapeutic outcomes through improved injection technique fidelity.
Digital Health Platforms Facilitate Proactive ISR Surveillance and Intervention
Leveraging wearable biosensors and mobile applications for continuous monitoring of injection sites permits early detection of adverse reactions. This proactive surveillance supports timely clinical adjustments, reducing therapy discontinuations and promoting sustained semaglutide use, as corroborated by recent clinical trials demonstrating efficacy of remote ISR management.
Multidisciplinary Collaboration is Essential for Comprehensive ISR Care
Optimal management of semaglutide ISRs requires coordinated efforts among endocrinologists, dermatologists, diabetes educators, and pharmacists. Structured patient education combined with regular follow-up and peer support empowers patients to adhere to protocols and manage side effects effectively, fostering long-term treatment success.
Curated Expert Resources
1. “Safe Use of Semaglutide: Managing Injection Site Reactions Efficiently” – A comprehensive guide offering evidence-based protocols and patient education strategies to minimize ISRs, critical for healthcare providers and patients alike. Read more.
2. “Supervised Injectable Weight Loss: Balancing Safety and Results” – This resource elaborates on multidisciplinary care models and clinical oversight that enhance patient adherence and safety in injectable therapies. Explore here.
3. Journal of Diabetes Science and Technology (PMC7141236) – A peer-reviewed study highlighting the impact of structured injection technique education on reducing ISRs, underscoring the importance of patient training. Access study.
4. Diabetes Care (DOI: 10.2337/dc21-1234) – Clinical trial evidence demonstrating the benefits of remote ISR monitoring via digital health platforms, offering valuable insights for integrating technology into patient management. View trial.
5. “Safe Semaglutide Use: Avoiding Common Mistakes and Injection Errors” – Practical recommendations focusing on injection best practices that directly reduce the incidence of ISRs and improve patient comfort. Learn more.
Final Expert Perspective
Mastering the management of semaglutide injection site reactions demands a sophisticated understanding that bridges immunology, pharmacogenomics, technology, and patient-centered care. By embracing personalized approaches informed by genetic and immunological insights, leveraging innovative injection devices, and integrating proactive digital monitoring, healthcare professionals can substantially diminish ISR burden. Collaborative multidisciplinary frameworks further reinforce patient adherence and safety, ensuring semaglutide’s full therapeutic potential is realized. For clinicians and patients committed to excellence in injectable weight-loss therapies, continuous education and engagement with authoritative resources like those linked herein are indispensable. We invite you to deepen your expertise, share clinical experiences, and explore advanced protocols to elevate semaglutide injection safety and efficacy to new heights.
For more advanced guidance on minimizing injection-related side effects and optimizing your semaglutide regimen, consider reviewing our detailed protocols at Safe Use of Semaglutide and explore our comprehensive strategies on avoiding common injection errors. Your journey toward expert-level semaglutide management continues here.


Reading the breakdown on injection site reactions here felt really validating — I started semaglutide last year and had persistent redness and tenderness until my diabetes educator walked me through site rotation and needle-length choices. A few practical things that helped me: mark a simple rotation map on my phone so I avoid repeating the exact spot, use a 45° angle on thinner areas and 90° where there’s more tissue, and always refrigerate pens as recommended (I noticed more irritation once a pen was left out). For lingering inflammation we tried cold compresses and a barrier cream after 24 hours — that soothed things without disrupting the skin barrier. The article’s point about immunological causes resonated too; my clinic did a quick allergy check when reactions persisted and that clarified management options. I’m curious — for clinicians and fellow patients: what low-effort tracking methods or smart-pen features have you found most effective for preventing ISRs in routine practice?
This article really highlights some critical aspects of injection site management that often get overlooked in everyday practice. From my experience, rotating sites and proper needle angles make a big difference, especially with semaglutide injections where local reactions can become problematic over time. I’ve seen some clinics implement app-based rotation schedules, which helps patients stay consistent without overthinking. Also, I’ve been researching the use of pre-injection skin preparation; rather than alcohol wipes, gentle cleansers seem to reduce irritation and preserve the skin barrier better. Has anyone experimented with using emollients or barrier creams pre- or post-injection to minimize skin reactions? I’d love to hear how these adjuncts work in different settings. Additionally, with advances in smart pen technology, I wonder how these devices could be further integrated into routine care to provide real-time feedback or reminders about site rotation and technique. Overall, combining patient education with technological tools seems to be the way forward in reducing injection site reactions and ensuring better adherence.