Unlocking the Power of Prescription Weight Loss Injections: Avoiding Pitfalls
Prescription injections for weight loss, such as semaglutide and tirzepatide, have transformed obesity management by offering effective appetite suppression and metabolic benefits. Yet, their success hinges on correct usage — injection mistakes can compromise results and even cause unwanted side effects. Understanding expert tips for preventing common errors can empower patients to maximize benefits safely.
Precision Matters: Choosing the Right Injection Site and Technique
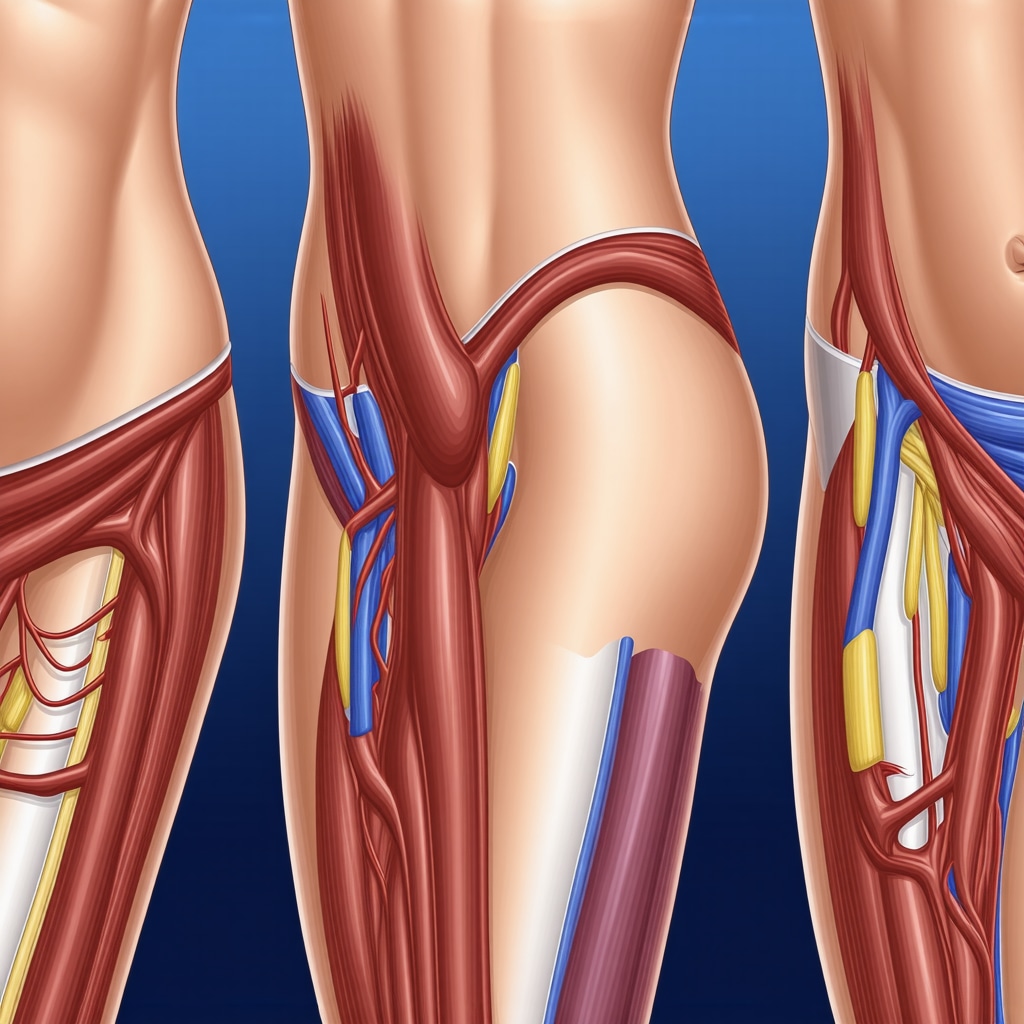
Injection site selection is crucial for optimal absorption and minimizing discomfort. Commonly recommended sites include the abdomen, thigh, or upper arm, rotating locations regularly to avoid tissue damage or lipodystrophy. Using a new, sterile needle each time and injecting at the correct angle (usually 90 degrees for subcutaneous injections) ensures medication is delivered properly beneath the skin. Incorrect technique, such as intramuscular injection or reusing needles, can lead to inconsistent dosing or infections.
Timing and Dosage: The Subtle Art of Consistency
Maintaining a consistent injection schedule aligned with prescribed dosage is essential. Skipping doses or injecting at irregular intervals disrupts steady-state medication levels, reducing effectiveness. Some patients struggle with injection anxiety or forgetfulness, which can be mitigated through reminders or support systems. Also, never adjust doses without professional guidance, as improper dosing risks side effects or suboptimal weight loss.
What Are the Most Frequent Injection Mistakes and How Can I Avoid Them?
Among common errors are injecting too quickly, failing to cleanse the site properly, and neglecting post-injection care. Injecting rapidly may cause pain or bruise formation. Cleaning the skin with alcohol swabs before injection reduces infection risk. Additionally, after injection, gently pressing the site without rubbing helps medication absorption and minimizes irritation. Patients should also be aware of signs of adverse reactions, such as persistent redness or swelling, and seek medical advice promptly.
Integrating Medical Guidance and Lifestyle for Sustainable Success
Expert supervision is indispensable. Medical professionals tailor injection plans, monitor progress, and adjust treatment to individual needs, which prevents errors and enhances outcomes. Combining injections with balanced nutrition and physical activity amplifies weight loss and promotes long-term health. For comprehensive advice on combining diet with injectable weight loss treatments, see our detailed guide on combining diet with injections.
Building Confidence: Overcoming Injection Anxiety and Ensuring Safety
Injection anxiety is a common barrier. Techniques such as deep breathing, distraction, or gradual exposure can ease apprehension. Learning proper injection methods through demonstration or supervised practice builds confidence. Safety protocols, including proper disposal of sharps and adherence to storage instructions, protect both the patient and others. Resources like doctor-approved advice on overcoming injection anxiety offer practical strategies.
For those seeking in-depth, physician-guided insights on fat loss injections and key safety tips, explore our resource on physician-guided fat loss injections.
Ready to enhance your injection technique and boost your weight loss journey? Share your experiences or questions below to join a community committed to safe, effective weight management!
According to a study published in the Journal of Obesity, proper injection technique significantly improves medication efficacy and reduces adverse events in GLP-1 receptor agonist therapies. This underscores the importance of patient education and professional oversight in prescription injection weight loss treatments.
Personal Lessons: How I Improved My Injection Routine
When I first started my journey with semaglutide injections, I was overwhelmed by the details—where to inject, when, and how to manage side effects. I remember missing doses early on because of forgetfulness and feeling anxious about the needle. But gradually, I developed a routine that worked for me. I set phone reminders to keep my schedule consistent, and I made sure to rotate injection sites to avoid soreness. These small adjustments made a world of difference—not just in my weight loss progress but also in my confidence using the medication.
Listening to Your Body: Managing Side Effects and Adjustments
One of the subtle yet critical aspects I learned was the importance of tuning into my body’s reactions. For instance, I noticed mild nausea during the first weeks, which is a common side effect with GLP-1 receptor agonists like semaglutide and tirzepatide. Instead of pushing through blindly, I consulted my healthcare provider who advised me on dosage adjustments and dietary changes to ease the symptoms. This personalized approach allowed me to stay on track without feeling discouraged. If you want detailed tips on managing gastrointestinal symptoms while using semaglutide safely, check out this guide to managing side effects.
How Can We Stay Motivated When Progress Plateaus or Challenges Arise?
Weight loss journeys are rarely linear, and plateaus can be frustrating. One thing I found helpful was focusing on non-scale victories like increased energy and improved mood. I also reminded myself that consistency in injections and lifestyle habits matters more than perfection. Joining online communities and reading success stories helped me stay motivated. For those experiencing plateaus, resources on overcoming weight loss plateaus with weekly injections offer practical strategies that complement medical treatment.
Combining Science and Support: Why Professional Guidance Matters
Scientific studies, such as one featured in the Journal of Obesity, emphasize that proper injection technique and medical supervision significantly improve outcomes with GLP-1 therapies. This resonated with my personal experience—working closely with my doctor to tailor dosages and address concerns kept me safe and effective throughout my weight loss journey. If you’re considering injectable treatments, partnering with a healthcare provider ensures your plan is customized and monitored for best results.
Encouraging Community: Let’s Share and Learn Together
Have you tried prescription weight loss injections, or are you curious about starting? What challenges or successes have you experienced? Sharing stories helps demystify the process and can motivate others to stay committed. Feel free to comment below with your experiences or questions. You might also find our article on doctor-approved tips for overcoming injection anxiety helpful if needles are a concern. Together, we can build a supportive community focused on safe, effective weight management.
Decoding Pharmacokinetics: How Injection Site Influences Drug Absorption and Efficacy
The pharmacokinetic profile of GLP-1 receptor agonists like semaglutide is profoundly affected by the chosen injection site due to differences in local blood flow, fat composition, and lymphatic drainage. For example, abdominal injections often yield faster absorption compared to thigh or upper arm sites, but this can also increase the risk of localized irritation. Understanding the nuanced interplay between regional tissue characteristics and drug delivery can empower patients to select injection sites that balance efficacy with tolerance. Experts recommend a systematic rotation schedule—not only to prevent lipohypertrophy but also to optimize consistent plasma drug levels, thereby stabilizing appetite suppression and metabolic responses.
What Are the Biochemical Implications of Injection Site Variability on Semaglutide’s Therapeutic Action?
Injection site variability can alter the rate at which semaglutide enters systemic circulation, impacting peak plasma concentration and half-life. Research published in Clinical Pharmacokinetics reveals that subcutaneous absorption kinetics differ significantly between abdominal and thigh administration, influencing both onset and duration of drug action. Clinicians must consider these pharmacodynamic nuances when advising patients, especially those with comorbid conditions that can affect subcutaneous tissue perfusion, such as diabetes or peripheral vascular disease.
Mitigating Immunogenicity and Injection Site Reactions Through Advanced Techniques
Immunogenicity, although rare with modern GLP-1 analogs, can manifest as injection site reactions including erythema, pruritus, or induration. Advanced injection techniques—such as ensuring slow, steady administration and avoiding repeated trauma to one site—reduce antigenic stimulation and inflammation. Employing pre-injection protocols like warming the medication to room temperature can also minimize discomfort and enhance absorption. In certain resistant cases, adjunctive topical therapies may be warranted under medical supervision to alleviate persistent reactions without compromising treatment adherence.
Integrating Continuous Glucose Monitoring (CGM) Data to Personalize Injection Timing and Dosage
Emerging evidence suggests that leveraging CGM technology can refine weight loss injection regimens by correlating glycemic patterns with appetite and metabolic shifts. For patients with insulin resistance or type 2 diabetes, synchronizing semaglutide administration with glycemic fluctuations may potentiate weight loss and improve glucose homeostasis. This precision medicine approach requires close collaboration between endocrinologists, dietitians, and patients to interpret CGM metrics and adjust dosing schedules dynamically.
Psychoneuroimmunology of Injection Anxiety: Beyond Behavioral Coping Strategies
Injection anxiety transcends mere fear of needles; it encompasses complex psychoneuroimmunological pathways that can influence immune responses and treatment outcomes. Chronic stress linked to injection apprehension may elevate pro-inflammatory cytokines, potentially exacerbating injection site reactions and systemic side effects. Integrative interventions—combining cognitive-behavioral therapy, mindfulness-based stress reduction, and biofeedback—have shown promise in modulating these pathways, enhancing patient adherence and satisfaction. Exploring these modalities with healthcare providers can transform the injection experience from distressing to empowering.
Call to Action: Engage with Expert-Led Forums to Elevate Your Injection Mastery
If you’re navigating the complexities of prescription weight loss injections, consider joining specialized forums and webinars hosted by endocrinologists and obesity medicine experts. These platforms provide opportunities to ask nuanced questions, share real-world experiences, and stay abreast of cutting-edge research. Your proactive engagement can catalyze a tailored, effective, and sustainable weight loss journey.
Decoding Pharmacokinetics: How Injection Site Influences Drug Absorption and Efficacy
The pharmacokinetic profile of GLP-1 receptor agonists like semaglutide is profoundly affected by the chosen injection site due to differences in local blood flow, fat composition, and lymphatic drainage. For example, abdominal injections often yield faster absorption compared to thigh or upper arm sites, but this can also increase the risk of localized irritation. Understanding the nuanced interplay between regional tissue characteristics and drug delivery can empower patients to select injection sites that balance efficacy with tolerance. Experts recommend a systematic rotation schedule—not only to prevent lipohypertrophy but also to optimize consistent plasma drug levels, thereby stabilizing appetite suppression and metabolic responses.
What Are the Biochemical Implications of Injection Site Variability on Semaglutide’s Therapeutic Action?
Injection site variability can alter the rate at which semaglutide enters systemic circulation, impacting peak plasma concentration and half-life. Research published in Clinical Pharmacokinetics reveals that subcutaneous absorption kinetics differ significantly between abdominal and thigh administration, influencing both onset and duration of drug action. Clinicians must consider these pharmacodynamic nuances when advising patients, especially those with comorbid conditions that can affect subcutaneous tissue perfusion, such as diabetes or peripheral vascular disease.
Mitigating Immunogenicity and Injection Site Reactions Through Advanced Techniques
Immunogenicity, although rare with modern GLP-1 analogs, can manifest as injection site reactions including erythema, pruritus, or induration. Advanced injection techniques—such as ensuring slow, steady administration and avoiding repeated trauma to one site—reduce antigenic stimulation and inflammation. Employing pre-injection protocols like warming the medication to room temperature can also minimize discomfort and enhance absorption. In certain resistant cases, adjunctive topical therapies may be warranted under medical supervision to alleviate persistent reactions without compromising treatment adherence.
Integrating Continuous Glucose Monitoring (CGM) Data to Personalize Injection Timing and Dosage
Emerging evidence suggests that leveraging CGM technology can refine weight loss injection regimens by correlating glycemic patterns with appetite and metabolic shifts. For patients with insulin resistance or type 2 diabetes, synchronizing semaglutide administration with glycemic fluctuations may potentiate weight loss and improve glucose homeostasis. This precision medicine approach requires close collaboration between endocrinologists, dietitians, and patients to interpret CGM metrics and adjust dosing schedules dynamically.
Psychoneuroimmunology of Injection Anxiety: Beyond Behavioral Coping Strategies
Injection anxiety transcends mere fear of needles; it encompasses complex psychoneuroimmunological pathways that can influence immune responses and treatment outcomes. Chronic stress linked to injection apprehension may elevate pro-inflammatory cytokines, potentially exacerbating injection site reactions and systemic side effects. Integrative interventions—combining cognitive-behavioral therapy, mindfulness-based stress reduction, and biofeedback—have shown promise in modulating these pathways, enhancing patient adherence and satisfaction. Exploring these modalities with healthcare providers can transform the injection experience from distressing to empowering.
Call to Action: Engage with Expert-Led Forums to Elevate Your Injection Mastery
If you’re navigating the complexities of prescription weight loss injections, consider joining specialized forums and webinars hosted by endocrinologists and obesity medicine experts. These platforms provide opportunities to ask nuanced questions, share real-world experiences, and stay abreast of cutting-edge research. Your proactive engagement can catalyze a tailored, effective, and sustainable weight loss journey.
Frequently Asked Questions (FAQ)
What are prescription weight loss injections and how do they work?
Prescription weight loss injections, such as semaglutide and tirzepatide, are medications that mimic or enhance hormones regulating appetite and metabolism. They work primarily by activating GLP-1 receptors, which suppress appetite, slow gastric emptying, and improve insulin sensitivity, thereby aiding in sustained weight loss when combined with lifestyle changes.
Why is rotating injection sites important?
Rotating injection sites prevents localized tissue damage like lipodystrophy and ensures consistent absorption. Different sites have varying blood flow and fat composition, impacting drug uptake. Regular rotation fosters optimal efficacy and reduces discomfort or injection site reactions.
How can I minimize injection site reactions?
To reduce reactions such as redness or swelling, use a new sterile needle each time, inject slowly and steadily, and avoid injecting into the same spot repeatedly. Warming the medication to room temperature before injection and properly cleansing the skin can also help. If reactions persist, consult your healthcare provider for possible topical treatments or technique adjustments.
What should I do if I miss a dose?
If you miss a dose, follow your prescribing physician’s guidance. Generally, take the next scheduled injection at the regular time rather than doubling doses. Maintaining consistent timing supports steady medication levels and effectiveness.
How does injection site choice affect semaglutide’s effectiveness?
Different sites like the abdomen, thigh, or upper arm have unique absorption rates due to local blood flow and tissue differences. Abdominal injections often lead to faster absorption but may increase irritation risk. Understanding these nuances helps tailor injection site selection to balance efficacy and tolerability.
Can continuous glucose monitoring (CGM) improve injection timing?
For patients with insulin resistance or type 2 diabetes, CGM data can guide injection timing by correlating blood glucose fluctuations with medication effects, potentially enhancing weight loss and glucose control. This approach requires collaboration with healthcare professionals for personalized dosing schedules.
How can I overcome injection anxiety?
Injection anxiety involves psychological and physiological factors. Techniques such as deep breathing, mindfulness, gradual exposure, cognitive-behavioral therapy, and biofeedback can reduce stress and immune-related side effects. Learning proper technique under supervision also builds confidence and safety.
Are there risks of immunogenicity with these injections?
Modern GLP-1 receptor agonists have low immunogenicity risk, but rare injection site reactions may occur. Proper technique and site rotation minimize immune responses. Persistent or severe reactions should be evaluated by healthcare providers.
Why is professional medical guidance essential when using weight loss injections?
Medical supervision ensures correct dosing, monitors side effects, adjusts treatment plans, and integrates lifestyle modifications. This tailored approach maximizes safety and long-term weight loss success.
Trusted External Sources
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides authoritative insights into obesity treatments and GLP-1 receptor agonist therapies, supporting evidence-based understanding of weight loss injections.
- Journal of Obesity: Offers peer-reviewed research on injection techniques, pharmacokinetics, and clinical outcomes related to prescription weight loss medications.
- Clinical Pharmacokinetics Journal: Contains detailed studies on absorption variability and pharmacodynamics of injectable agents like semaglutide, informing expert clinical recommendations.
- American Association of Clinical Endocrinologists (AACE): Publishes guidelines and consensus statements on obesity management, including injectable therapies and patient safety protocols.
- Obesity Medicine Association (OMA): A professional body providing education and resources on safe, effective obesity treatments and emerging technologies such as CGM integration.
Conclusion
Prescription weight loss injections represent a powerful tool in the battle against obesity, offering scientifically backed mechanisms to reduce appetite and improve metabolism. However, their success is intricately linked to meticulous injection technique, consistent scheduling, and professional oversight. Understanding the biochemical and pharmacokinetic nuances—such as injection site selection and absorption variability—empowers patients to optimize therapeutic outcomes while minimizing side effects. Moreover, addressing psychological aspects like injection anxiety through integrative approaches enhances adherence and satisfaction. Combining these injections with lifestyle modifications and leveraging advanced monitoring tools such as CGM can personalize treatment further. Ultimately, engaging with healthcare providers and expert communities fosters a safer, more effective, and sustainable weight loss journey. We invite you to share your experiences, ask questions, and explore our related expert content to deepen your knowledge and confidence in managing weight with prescription injections.


This article really highlights the significance of proper injection technique in maximizing the benefits of prescription weight loss injections like semaglutide and tirzepatide. When I started using semaglutide, I underestimated how crucial site rotation was to avoid soreness and ensure consistent absorption. I also learned that injecting too quickly can lead to bruising and discomfort, something that wasn’t immediately obvious. The suggestion to gently press the site afterward without rubbing made a noticeable difference in reducing irritation for me.
Another aspect that resonated was the challenge of maintaining consistency, which I struggled with at first due to forgetfulness. Setting phone reminders and involving a family member for accountability helped me stay on track. Also, the psychological side—overcoming injection anxiety—was a hurdle I faced, and I found that simple deep-breathing exercises before injections helped ease my nerves.
I’m curious, have others found particular injection sites more comfortable or effective based on their own experience, especially considering the pharmacokinetic differences mentioned in the article? Also, how do you manage side effects like mild nausea early on without feeling discouraged? Sharing these insights could really support others navigating this journey.
This article really emphasizes the importance of technique and consistency when it comes to injection-based weight loss treatments like semaglutide. I’ve personally experienced how crucial it is to rotate sites properly, not just for comfort but to prevent issues like lipodystrophy. I also found that injecting slowly and using a new sterile needle every time significantly reduced discomfort and minimized the risk of infection. One challenge I encountered early on was managing injection anxiety, especially with the fear of needles; I discovered that practicing deep breathing and using distraction techniques helped me feel more at ease. Interestingly, I’ve noticed that the abdominal area tends to be the most comfortable for me and provides quicker absorption, aligning with pharmacokinetic insights I read about recent. Have others found that certain injection sites work better for their absorption or comfort? Also, how do you cope with initial side effects like nausea without feeling discouraged? Hearing different experiences could really help new users stay motivated and find their best routine.