Unlocking the Art of Dosage: Why Precision Matters in Prescription Injection Weight Loss
Prescription injections for weight loss, such as semaglutide and tirzepatide, have revolutionized obesity management by offering potent, hormone-based therapies that suppress appetite and enhance metabolism. However, the key to harnessing their full potential lies in expertly balancing the dosage. A carefully calibrated dose not only maximizes fat loss but also minimizes side effects and sustains long-term success.
Understanding the intricate interplay between medication dosage, individual physiology, and lifestyle factors is essential. This demands a personalized approach guided by medical expertise, as improper dosing can lead to suboptimal results or unwanted complications. This article delves into advanced strategies for balancing prescription injection weight loss dosages effectively, backed by clinical insights and real-world experience.
Personalized Titration: Navigating the Fine Line Between Efficacy and Tolerance
One of the most critical components in managing prescription injection weight loss is individualized titration—the gradual adjustment of dosage tailored to the patient’s response. Starting at a low dose and incrementally increasing allows the body to adapt, reducing gastrointestinal discomfort or injection site reactions common with GLP-1 receptor agonists.
For example, a patient beginning semaglutide therapy might start at 0.25 mg weekly, progressing every 4 weeks to a maintenance dose of 1 mg or higher as tolerated. This approach balances efficacy with safety, enabling better adherence and improved appetite control.
Synergizing Dosage with Lifestyle: The Role of Diet and Physical Activity
While prescription injections act as powerful metabolic modulators, their effectiveness is magnified when integrated with tailored diet and exercise regimens. Adjusting dosage without considering caloric intake or physical activity levels can blunt results or increase side effects.
Evidence suggests that combining optimal dosing with a balanced, nutrient-rich diet and regular moderate exercise enhances fat loss and preserves lean muscle mass. Patients should collaborate closely with healthcare providers to align injection schedules and dosages with lifestyle changes for sustainable outcomes. For further guidance, explore our detailed guide on combining diet with injectable weight loss.
How Can Patients and Physicians Collaborate to Adjust Dosage Safely and Effectively?
Open communication and continuous monitoring are paramount. Patients should track their progress, noting changes in appetite, weight, side effects, and overall wellbeing. Physicians can then make informed dosage adjustments based on these insights, laboratory data, and clinical judgment.
Regular follow-ups, possibly supported by digital health tools or weekly injection guides, empower precise dose optimization. This dynamic partnership ensures that the treatment evolves with the patient’s changing needs, maximizing safety and efficacy. Learn more about weekly injection weight loss guides to stay consistent and informed.
Expert Tips for Minimizing Side Effects While Maximizing Results
Side effects like nausea, vomiting, and injection site irritation can hinder adherence. To counter this, experts recommend slow dose escalation, proper injection techniques, and timing injections with meals to reduce gastrointestinal distress.
Additionally, hydration and avoiding sudden dietary changes can further ease side effects. For comprehensive safety practices, visit our resource on avoiding side effects in prescription injection weight loss.
Practical experience shows that patients who embrace these strategies report higher satisfaction and better weight loss outcomes, underscoring the importance of a holistic, medically supervised approach.
For more expert insights on managing your prescription injection journey, feel free to contact us or share your experience in the comments below. Your journey to balanced, effective weight loss is unique—let’s navigate it together.
For authoritative clinical information on GLP-1 receptor agonists and their role in weight loss, refer to the National Institutes of Health review on semaglutide therapy.
Listening to Your Body: The Subtle Art of Dose Adjustment
In my experience with prescription injections like tirzepatide, I found that learning to listen to my body’s signals was a game-changer. When I first began, the initial doses felt manageable, but as increments happened, slight nausea or fatigue crept in. Instead of pushing through blindly, I started keeping a journal to track how each dose affected my appetite, energy, and mood. This simple habit allowed me and my physician to tailor the dosage more precisely, ensuring I stayed within a comfort zone that still promoted fat loss.
This personal trial-and-error journey echoed findings in a comprehensive NIH review highlighting the importance of individualized titration to balance efficacy and side effects. It’s a reminder that no two people respond identically, and patience is key.
Incorporating Mindful Eating with Injection Timing
One insight I never expected was how much the timing of injections influenced my hunger cues. Injecting semaglutide or tirzepatide well before meals helped me experience reduced cravings and smaller portion sizes naturally. Pairing this with mindful eating practices—such as savoring flavors and eating slowly—amplified the medication’s appetite-suppressing effects.
For those wondering how to best synchronize injection timing with lifestyle, exploring resources like our guide on safe semaglutide use can offer practical tips that blend medical advice with everyday habits.
How Do You Know When It’s Time to Adjust Your Dose?
This question often comes up among people on injectable weight loss treatments. From my perspective, it’s a mix of monitoring physical reactions and progress milestones. If side effects become overwhelming or weight loss plateaus for several weeks, it might be time to consult your healthcare provider about adjusting your dose. Likewise, if you feel better and side effects diminish, some patients might maintain their dose longer before increasing.
Open dialogue with your doctor is crucial, especially when navigating these nuances. Using tools like weekly injection guides can help keep track of these patterns systematically.
Why Professional Guidance Is Non-Negotiable
While self-awareness is powerful, relying on professional guidance ensures safety and maximizes results. Medical supervision includes necessary lab tests, potential dose adjustments, and managing any emerging health concerns. I’ve found that my doctor’s insights, combined with my own observations, made my weight loss journey smoother and more sustainable.
If you’re considering or currently using prescription injection therapies, I highly recommend partnering with a knowledgeable healthcare provider. Their expertise can help you avoid common pitfalls and customize your plan to your unique needs—something I’ve personally benefited from and continue to trust.
For a comprehensive look at physician-guided injection plans, check out this resource on physician-guided fat loss injections.
I’d love to hear about your experiences or questions regarding dosage adjustments or managing your weight loss injections. Feel free to share in the comments below or explore more expert tips on effective tirzepatide use to manage appetite and boost your journey.
Decoding Pharmacodynamics: How Drug Absorption and Metabolism Influence Dosage Precision
To optimize prescription injection weight loss therapies such as semaglutide and tirzepatide, a nuanced understanding of pharmacodynamics and pharmacokinetics is indispensable. These drugs, primarily GLP-1 receptor agonists, exhibit complex absorption patterns and metabolic pathways that directly affect their bioavailability and efficacy.
For instance, semaglutide has a long half-life, enabling once-weekly dosing, but interindividual variations in hepatic metabolism and renal clearance can alter systemic drug levels. Such variability necessitates dose individualization beyond standard titration protocols to achieve sustained appetite suppression without provoking intolerable side effects.
Advanced monitoring approaches, including plasma drug concentration assays and pharmacogenomic profiling, are emerging tools that can inform precise dosage adjustments tailored to the patient’s metabolic profile. Incorporating these cutting-edge diagnostics into clinical practice can transform the dosing paradigm from reactive to predictive and personalized.
Integrating Real-Time Digital Health Data to Refine Dose Adjustments
With the advent of wearable technology and mobile health applications, clinicians and patients now have unprecedented access to continuous biometric data such as heart rate variability, glucose levels, and activity patterns. Leveraging this data can provide dynamic feedback on how the patient responds to a given dose of weight loss injections.
For example, subtle shifts in glucose trends or energy expenditure might indicate an optimal window for dose escalation or stabilization. Conversely, early detection of adverse physiological responses can prompt timely dose reduction, minimizing risk and discomfort.
Integrating machine learning algorithms to analyze these data streams promises to automate and enhance dosage personalization. A recent study published in Nature Medicine demonstrated the feasibility of AI-driven dose optimization in metabolic therapies, underscoring the potential of this approach.
What Are the Challenges and Solutions in Implementing Pharmacogenomics for Injection Dose Personalization?
Pharmacogenomics offers a frontier for individualized dosing by elucidating genetic variations that influence drug response. However, real-world implementation faces hurdles such as cost, limited clinician familiarity, and the complexity of interpreting genetic data within the context of multifactorial obesity.
Solutions include developing standardized genetic panels focused on GLP-1 receptor pathway genes, integrating decision-support tools into electronic health records, and fostering interdisciplinary collaboration between geneticists, endocrinologists, and primary care providers.
Moreover, educating patients about the benefits and limitations of genetic testing can enhance engagement and adherence to personalized treatment plans. As this field matures, pharmacogenomics could become a cornerstone for optimizing injection dosages, reducing trial-and-error approaches, and improving long-term outcomes.
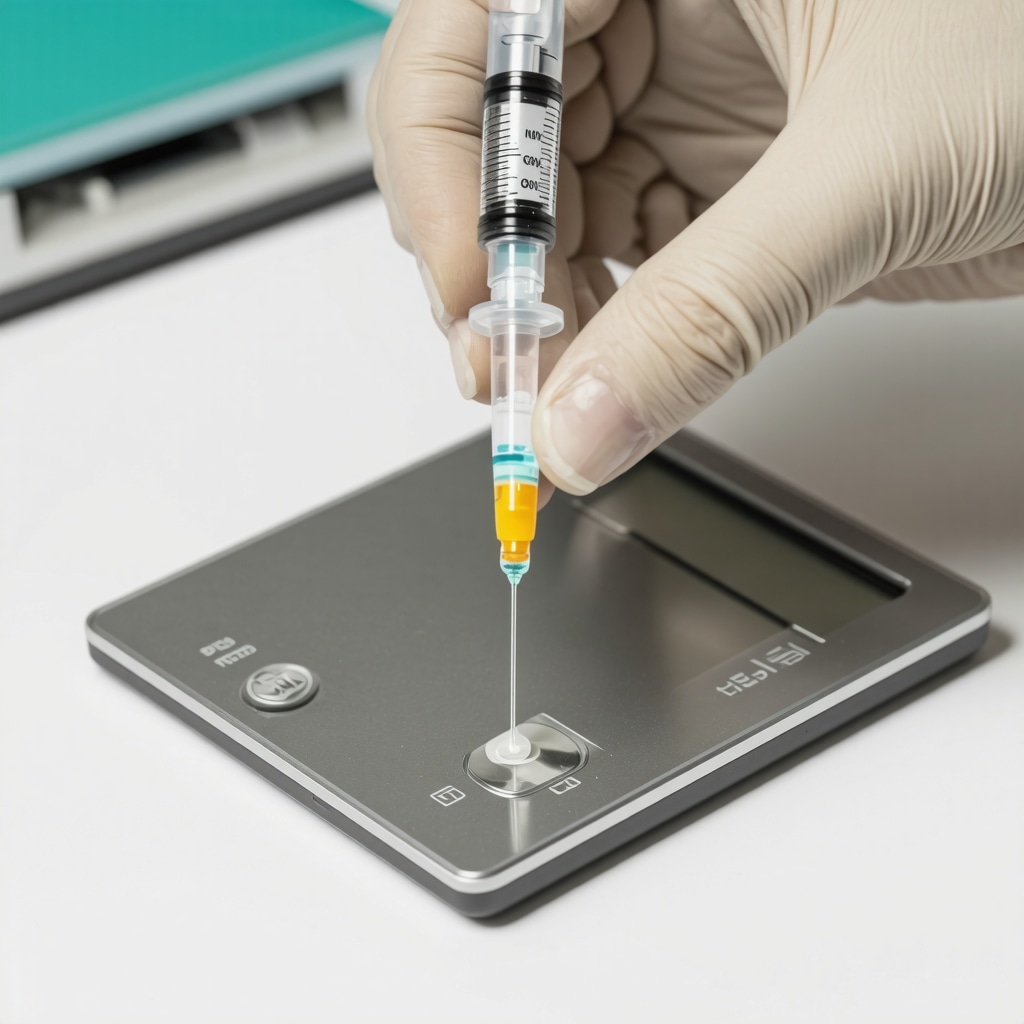
Beyond Dosage: Addressing Injection Technique and Site Selection for Maximal Drug Efficacy
While dosage calibration is critical, the efficacy of prescription injections is also influenced by proper administration techniques. Variations in injection site (abdomen, thigh, or upper arm), needle angle, and depth can affect drug absorption rates and patient comfort.
Professional training for patients on aseptic techniques, rotation of injection sites to prevent lipodystrophy, and selection of appropriate needle length can mitigate complications and ensure consistent pharmacological effects.
Emerging innovations such as microneedle patches and auto-injectors aim to standardize administration, reduce discomfort, and improve adherence, thereby complementing dosage optimization strategies.
For a detailed exploration of advanced injection techniques and their impact on weight loss efficacy, visit our comprehensive resource on Advanced Injection Techniques for Weight Loss.
Harnessing Pharmacogenomics: Tailoring Dosage through Genetic Insights
As the landscape of weight loss injections evolves, integrating pharmacogenomic data offers an unprecedented opportunity to refine dosing strategies beyond conventional titration. Genetic polymorphisms affecting GLP-1 receptor expression, drug metabolism enzymes like CYP450 isoforms, and transport proteins can dramatically influence individual responses to agents such as semaglutide and tirzepatide.
By identifying these genetic markers through targeted panels, clinicians can predict efficacy and side effect profiles more accurately, reducing the trial-and-error cycles that often prolong patient discomfort and suboptimal outcomes. This precision medicine approach not only enhances therapeutic success but also aligns with emerging standards of personalized obesity care.
Leveraging Digital Biometrics for Dynamic Dose Modulation
The integration of real-time biometric data, including continuous glucose monitoring and wearable metabolic trackers, empowers a responsive dosing framework that adapts to physiological fluctuations. This method transcends static dosing schedules by incorporating feedback loops that detect early signs of reduced efficacy or adverse reactions, enabling preemptive dose recalibrations.
Artificial intelligence algorithms analyzing longitudinal data streams can pinpoint patterns correlating with optimal drug plasma levels and metabolic responses, thereby enhancing adherence and clinical outcomes. This interplay between technology and pharmacotherapy heralds a new era of data-driven weight management.
What Are the Clinical Implications of Injection Site Variability on Drug Absorption and Patient Outcomes?
Injection site selection critically impacts the pharmacokinetics of GLP-1 receptor agonists. Studies indicate that abdominal injections generally yield faster absorption compared to thigh or upper arm sites, potentially influencing peak plasma concentrations and therapeutic effects.
Moreover, repetitive injections in the same area can provoke lipohypertrophy, altering drug uptake and causing discomfort. Educating patients on systematic site rotation and proper injection techniques is essential to maintaining consistent drug bioavailability and minimizing local adverse events.
For comprehensive guidelines on optimizing injection practices, consult the Journal of Clinical Endocrinology & Metabolism, which provides evidence-based recommendations on administration site impact.
Innovations in Delivery Systems: Microneedle Patches and Beyond
Emerging delivery technologies such as microneedle patches offer promising alternatives to traditional injection methods, potentially improving patient acceptance and adherence. These minimally invasive devices facilitate controlled release and enhanced bioavailability while reducing pain and injection-site reactions.
Clinical trials exploring these novel systems are underway, signaling a paradigm shift in how obesity pharmacotherapy might be administered in the near future.

Empowering Patients: Collaborative Dose Adjustment and Monitoring
Empowering patients through education and digital tools fosters a proactive approach to dose management. Digital diaries, symptom trackers, and telemedicine consultations enable timely communication between patients and healthcare providers, facilitating individualized dose modifications aligned with evolving clinical and lifestyle factors.
This collaborative model not only enhances safety but also optimizes therapeutic efficacy, underscoring the importance of patient engagement in advanced weight loss injection regimens.
Ready to elevate your weight loss journey with precision dosing and expert guidance? Connect with our specialists today and unlock tailored strategies that maximize your success.
Frequently Asked Questions (FAQ)
What factors determine the optimal dosage for prescription weight loss injections like semaglutide and tirzepatide?
The optimal dosage depends on individual physiology, including metabolic rate, hepatic and renal function, genetic makeup influencing drug metabolism, and tolerance to side effects. Lifestyle factors such as diet and exercise also play a significant role. Personalized titration guided by healthcare providers ensures dose adjustments that maximize efficacy while minimizing adverse effects.
How long does it typically take to reach an effective maintenance dose during titration?
Most protocols start with a low initial dose, such as 0.25 mg of semaglutide weekly, gradually increasing every 4 weeks based on tolerance and response. It often takes 12 to 16 weeks to reach a maintenance dose that balances effectiveness and safety, but this timeline can vary depending on individual adaptation and side effect profile.
Can injection site selection affect the absorption and effectiveness of these medications?
Yes, injection sites like the abdomen generally allow faster absorption compared to the thigh or upper arm. Rotating injection sites is crucial to avoid lipohypertrophy, which can impair drug uptake and cause discomfort. Proper technique and site rotation contribute to consistent drug bioavailability and improved patient outcomes.
Are there emerging technologies that improve dosing precision and patient experience?
Innovations such as microneedle patches and auto-injectors aim to standardize dosing, reduce discomfort, and enhance adherence. Additionally, integrating digital health tools and real-time biometric data enables dynamic dose adjustments tailored to physiological responses, moving towards a more personalized treatment approach.
How does pharmacogenomics influence dosing strategies in weight loss injections?
Pharmacogenomics identifies genetic variations affecting drug metabolism and receptor sensitivity, enabling clinicians to predict individual responses and side effect risks. This information supports personalized dosing regimens, reducing trial-and-error adjustments and improving therapeutic outcomes.
What role do lifestyle factors play in conjunction with prescription weight loss injections?
Dietary habits and physical activity significantly impact the effectiveness of injections. Combining optimized dosing with balanced nutrition and regular exercise enhances fat loss, preserves lean muscle, and reduces side effects. Collaboration between patients and healthcare providers to integrate lifestyle changes is vital for sustainable success.
How can patients actively participate in safe and effective dose adjustments?
Patients can maintain detailed symptom and progress journals, utilize digital tracking tools, and maintain open communication with their healthcare providers. Monitoring appetite changes, side effects, and weight trends supports informed dose modifications and safer therapy management.
When should a patient consult their physician about adjusting their injection dose?
If side effects become intolerable, weight loss plateaus for several weeks, or if there are new health concerns, patients should seek medical advice. Timely professional evaluation ensures appropriate dose adjustments and maintains treatment safety and efficacy.
What are best practices to minimize side effects from weight loss injections?
Slow dose escalation, proper injection technique, timing injections with meals, adequate hydration, and avoiding sudden dietary changes help reduce nausea, vomiting, and injection site irritation. Patient education on these practices supports better adherence and outcomes.
Is professional supervision necessary throughout the injection therapy?
Yes, continuous medical supervision is essential to monitor health parameters, manage dosing, and address side effects or complications. Physician guidance ensures personalized, safe, and effective treatment tailored to evolving patient needs.
Trusted External Sources
- National Institutes of Health (NIH) – Semaglutide Therapy Review: Provides comprehensive clinical data on semaglutide’s efficacy, safety profiles, and titration protocols, serving as a foundational resource for understanding GLP-1 receptor agonists in obesity management.
- Journal of Clinical Endocrinology & Metabolism: Offers peer-reviewed research on injection site pharmacokinetics and administration techniques that influence drug absorption and patient outcomes, essential for optimizing injection practices.
- Nature Medicine – AI-Driven Dose Optimization Study: Details cutting-edge research on integrating artificial intelligence and real-time biometric data to personalize metabolic therapy dosing, highlighting the future of precision medicine in weight loss injections.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Provides evidence-based guidelines on obesity pharmacotherapy, including clinical best practices for injection-based weight loss treatments and multidisciplinary patient management.
- Pharmacogenomics Journal: Explores genetic influences on drug metabolism and receptor activity relevant to GLP-1 receptor agonists, supporting the integration of genetic data into personalized dosing strategies.
Conclusion
Mastering prescription injection weight loss hinges on the precise calibration of dosage tailored to individual metabolic profiles, genetic factors, and lifestyle habits. This article has illuminated how personalized titration, informed by pharmacodynamics and enhanced by digital health innovations, fosters maximal fat loss with minimal side effects. Emphasizing collaborative patient-provider relationships and emerging technologies like pharmacogenomics and AI-driven monitoring heralds a new era of precision obesity care.
By integrating expert injection techniques, mindful lifestyle synchronization, and dynamic dose adjustments, patients can achieve sustainable, effective weight loss outcomes. As this field rapidly evolves, staying informed and engaged with healthcare specialists is paramount.
Embark on your tailored weight loss journey today—share your experiences, consult with professionals, and explore our expert resources to unlock the full potential of prescription injection therapies.

I appreciate how this article highlights the complexity behind dosing for prescription injection weight loss therapies like semaglutide and tirzepatide. Having spoken to a friend who’s on semaglutide, they emphasized how important it was to progress slowly with dosage adjustments to avoid side effects like nausea and fatigue. What stood out to me is the mention of integrating lifestyle factors—diet and exercise—into dosage planning. It seems that without tailoring the medicine to one’s individual physiology and habits, the effectiveness could be compromised.
Also, the idea of keeping a detailed journal to communicate with the doctor about how the body responds to each dose feels so practical. It made me wonder, though: For people who struggle with maintaining consistent follow-up or don’t have access to frequent medical check-ins, how can they best ensure safe dose titration? Are digital tools or telemedicine consultations as effective in supporting those adjustments compared to in-person visits?
I’d be interested in hearing experiences of readers who have navigated this balance—how did you collaborate with your healthcare providers to find a dosage that works for you? Did lifestyle changes substantially impact your treatment progress?
Replying to Megan’s thoughtful points: While in-person visits are ideal for initial prescription injection weight loss dosage adjustments due to the nuanced monitoring required, I’ve personally found that telemedicine combined with digital health tools can be quite effective for ongoing titration—especially for those with limited access to specialists. Using digital diaries and symptom trackers to log appetite changes, side effects, and weight fluctuations lets patients provide their physicians with detailed, real-time data. This continuous flow of information can guide safety-conscious dose escalations or modifications without frequent office visits.
However, the success of remote management hinges on the patient’s commitment to detailed tracking and clear communication. It’s also important that healthcare providers are proactive about scheduling virtual check-ins to discuss progress and concerns. Additionally, integrating biometric data from wearables could soon enhance this remote titration process by adding objective physiological metrics.
On the lifestyle front, aligning dosage with personalized diet and exercise routines is crucial. For example, during periods of increased physical activity, some patients might experience different appetite responses, potentially necessitating dosage fine-tuning.
Has anyone else embraced telehealth for injection dose management? What digital tools or strategies did you find most helpful in maintaining safe and effective titration? Also, how closely did your lifestyle modifications impact your dosing journey?
Reading this comprehensive article really highlighted for me just how crucial individualized titration is in managing weight loss injections effectively. I’ve always been fascinated by how much patient-specific factors like metabolism, genetics, and lifestyle habits influence medication responses. It makes perfect sense that starting low and incrementally adjusting doses not only improves tolerance but also fosters long-term adherence.
One aspect I found particularly interesting was the connection between injection timing and mindful eating. I’ve noticed in some anecdotal reports that synchronizing injections before meals can help with appetite control through natural cues rather than forcing restrictions. This seems like an important yet sometimes overlooked piece of the puzzle.
However, I wonder how many patients truly receive thorough education about injection techniques and the importance of site rotation. Improper administration can jeopardize absorption and increase side effects, which could undermine the whole therapy.
Has anyone experienced challenges mastering injection methods or found specific training resources especially helpful? Also, how do healthcare providers ensure patients stay engaged and informed over time, especially when treatment spans several months? It would be insightful to hear practical strategies others have found effective in blending medical guidance with patient empowerment in this area.
I find it fascinating how this article emphasizes the need for precise and personalized dosing when it comes to prescription injection weight loss treatments like semaglutide and tirzepatide. What’s particularly striking is the integration of pharmacogenomics and digital health data into dosage decisions. It makes me wonder how widely accessible these advanced tools are in everyday clinical practice, especially in rural or underserved areas. From my understanding, while genetic testing and continuous biometric monitoring can revolutionize how doses are tailored, barriers such as cost and availability might limit their use.
On the topic of injection technique and site selection, I’ve noticed that many patients overlook how critical these factors are in drug absorption and overall efficacy. I once spoke with someone who experienced unexpected variations in their results simply because they hadn’t rotated injection sites properly, which caused localized tissue changes that affected absorption.
Given these complexities, I’d be curious to hear how other patients or providers ensure that education on injection best practices remains consistent throughout long-term treatment. Are there particular resources or training methods that have proven effective in keeping patients well-informed and engaged? How do clinicians balance the technical aspects of dose individualization with practical, day-to-day guidance that patients can realistically follow?
This article does a fantastic job highlighting the importance of precision in dosing prescription injections like semaglutide and tirzepatide. From my own experience supporting a family member on semaglutide, one thing that became clear was how crucial the combination of medication with lifestyle—particularly diet and exercise—is for meaningful, sustainable results. Without adjusting calorie intake and activity levels, the medication’s efficacy can plateau or side effects become more challenging to manage.
Also, I found the section on monitoring side effects and progress extremely valuable. Keeping a daily health journal proved instrumental in our case for communicating subtle changes with the healthcare provider. It allowed for timely dosage adjustments that balanced effectiveness with fewer adverse effects. I’m intrigued by the potential of integrating real-time biometric data from wearables to further personalize dosing; this could be a game-changer for patients who can’t attend frequent in-person visits.
One challenge I’ve seen is that some patients underestimate the learning curve around proper injection techniques and site rotation, which can inadvertently affect absorption. Does anyone have recommendations on where to find clear, ongoing education resources or how providers can better support patients in mastering these practical skills? Also, how do clinicians realistically incorporate pharmacogenomic insights into everyday dosage decisions in current practice?