When Medication Meets Appetite—A Tale of Unexpected Allies
Imagine this: your stomach growls at 3 PM sharp, as punctual as a Swiss watch, despite your best intentions to eat light and healthy. We’ve all been there, wrestling with those relentless hunger pangs that seem to mock our willpower. Enter the world of appetite-managing medications—where science lends a hand to tame the beast within. But is popping a pill the magic fix, or is there more nuance lurking beneath?
Doctors Weigh In: Medications as Partners, Not Puppeteers
Leading endocrinologists and nutrition experts emphasize that medications designed to manage appetite are sophisticated tools, not shortcuts. Drugs like GLP-1 receptor agonists (think: semaglutide or tirzepatide) work by modulating hormones that influence hunger and satiety, effectively rewiring your body’s signals. This isn’t about suppressing hunger willy-nilly but rather restoring balance where it’s been disrupted.
Can Medication Really Outsmart Your Cravings?
It’s a fair question. While these medications can blunt the intensity of cravings and reduce overall food intake, they don’t operate in a vacuum. Lifestyle factors—stress, sleep quality, and emotional triggers—continue to play starring roles. For instance, a 2022 study published in the Journal of Clinical Endocrinology & Metabolism highlights how GLP-1 therapies improve appetite control by enhancing satiety signals but advises a comprehensive approach including diet and behavioral changes.
Expert Tips for Navigating Medication and Appetite Control
Doctors recommend pairing medication with mindful eating strategies and personalized nutrition plans to maximize benefits. One effective approach involves scheduling meals and snacks to harmonize with medication timing, thereby preventing dips in blood sugar that often trigger hunger spikes. Curious about practical guidance? Check out this insightful expert advice on balancing energy and appetite with tirzepatide.
Remember, appetite management medications are not one-size-fits-all. Close collaboration with healthcare providers ensures dosing and treatment plans are tailored for your unique physiology and lifestyle, minimizing side effects and enhancing outcomes.
The Human Side of Appetite Management
Beyond the science and prescriptions lies a deeply human story. Managing appetite with medication can lift the fog of constant hunger that saps motivation and confidence. It’s not just about weight loss; it’s reclaiming control over your relationship with food. So, how are you managing your appetite journey? Share your stories and questions—sometimes, the best insights come from real-life experiences.
Beyond the Prescription: The Vital Role of Lifestyle in Appetite Management
While medications such as semaglutide and tirzepatide represent groundbreaking advancements in appetite regulation, their effectiveness is significantly amplified when combined with intentional lifestyle choices. Experts caution that relying solely on injectable therapies without addressing dietary habits, physical activity, and psychological factors often leads to suboptimal results. This holistic approach not only supports sustainable weight loss but also fosters lasting behavioral change.
Incorporating regular physical activity, for example, has been shown to improve insulin sensitivity and modulate hunger hormones, synergizing with the pharmacological action of GLP-1 receptor agonists. Additionally, stress management techniques—ranging from mindfulness meditation to structured cognitive behavioral therapy—can mitigate emotional eating triggers that often undermine medication efficacy.
Precision Timing: How Synchronizing Meals with Medication Can Optimize Appetite Control
Timing is more than just a convenience; it’s a strategic element in appetite management therapy. Aligning meal schedules with injection times can help stabilize blood glucose levels, preventing the metabolic dips that provoke overeating. For patients using weekly injections like semaglutide, clinicians often recommend establishing consistent eating windows that correspond with peak drug activity.
Moreover, careful planning around injection days—such as opting for nutrient-dense, low-glycemic snacks—can reduce gastrointestinal discomfort and nausea, common side effects that might otherwise disrupt adherence. For tailored guidance, explore our detailed insights on meal planning strategies to support injection days.
What Are the Latest Clinical Insights on Combining Medication and Behavioral Interventions for Appetite Control?
Emerging clinical evidence increasingly supports a dual-pronged approach combining pharmacotherapy with behavioral interventions to achieve superior appetite regulation and weight loss outcomes. A 2023 review in Obesity Reviews analyzed randomized controlled trials demonstrating that patients who received GLP-1 receptor agonists alongside cognitive behavioral therapy or structured dietary counseling experienced more significant reductions in hunger and better long-term adherence than those on medication alone.
These findings underscore the importance of personalized, physician-guided treatment plans that integrate medication, nutrition, physical activity, and psychological support. Such comprehensive strategies not only optimize appetite control but also enhance metabolic health and quality of life.
Engage and Share Your Journey
Your experience matters. How have you integrated appetite-managing medication with lifestyle changes? Share your insights or questions in the comments below to foster a community of informed support and practical wisdom. If you’re interested in deepening your understanding, consider reading our expert article on the importance of personalized treatment plans in medically supervised weight loss.
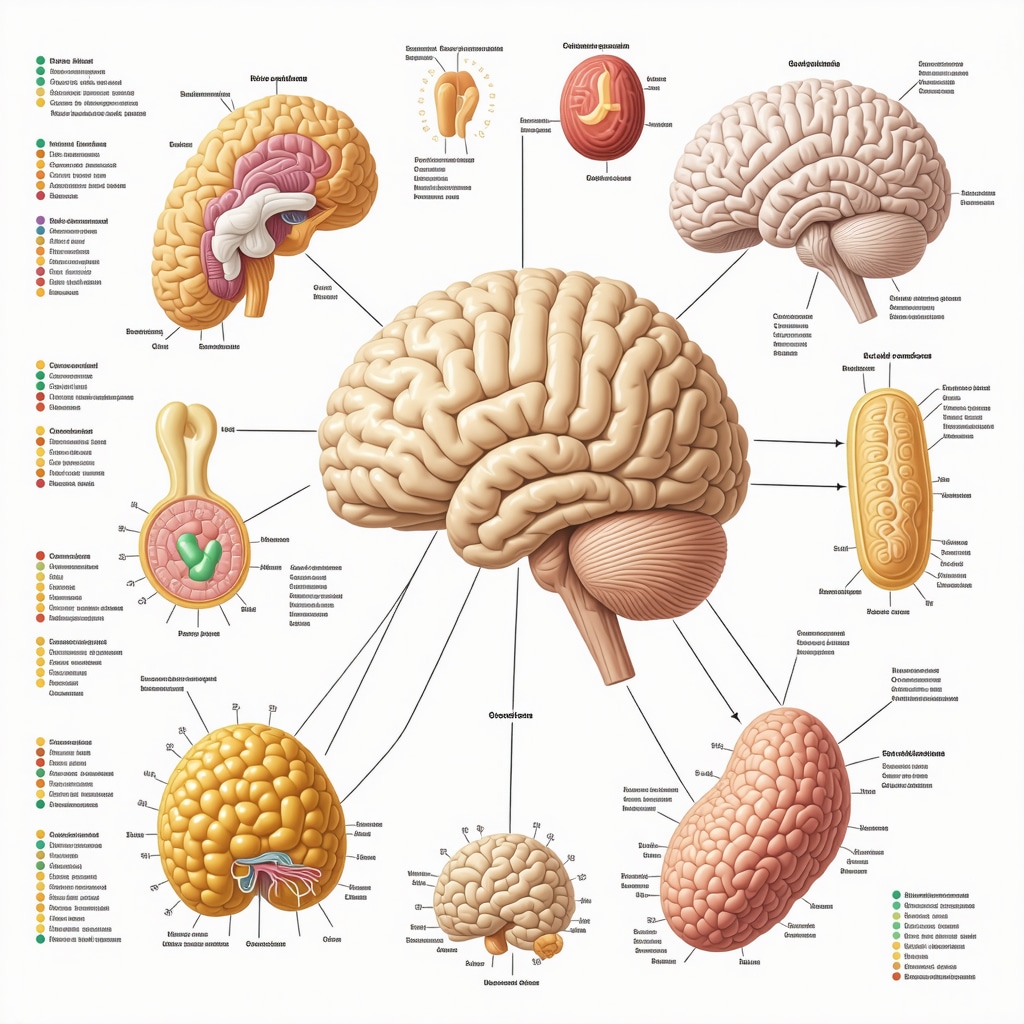
Decoding the Neuroendocrine Symphony: How Appetite Medications Interface with Brain Circuits
Understanding the complex neuroendocrine pathways modulated by appetite-suppressing medications reveals why these treatments are far more than simple appetite blockers. GLP-1 receptor agonists, for instance, not only activate satiety centers in the hypothalamus but also influence reward pathways linked to dopamine signaling. This dual action helps modulate both homeostatic hunger and hedonic cravings, addressing the multifaceted nature of eating behavior.
Recent neuroimaging studies demonstrate that patients on semaglutide exhibit reduced activity in the insula and orbitofrontal cortex—key brain regions implicated in food cue reactivity—thereby attenuating the impulsive drive to consume palatable foods. Such findings highlight the medication’s role in recalibrating neural circuits rather than merely suppressing appetite mechanically.
How Do Appetite Medications Affect Long-Term Neuroplasticity and Eating Behavior?
Emerging evidence suggests that beyond acute pharmacological effects, appetite medications may facilitate neuroplastic changes conducive to healthier eating habits. A 2024 study published in Neuroscience Letters investigated synaptic remodeling in hypothalamic neurons following prolonged GLP-1 receptor agonist treatment. Results indicated enhanced synaptic strength and altered receptor expression patterns, which could underpin sustained improvements in appetite regulation and metabolic homeostasis.
This neuroplastic potential opens avenues for combining pharmacotherapy with cognitive-behavioral interventions aimed at reinforcing adaptive eating behaviors, suggesting a window for synergistic therapeutic strategies.
Personalized Nutrition Meets Pharmacogenomics: Tailoring Appetite Management at the Molecular Level
Pharmacogenomic profiling is rapidly emerging as a transformative tool in optimizing appetite medication regimens. Variations in genes encoding GLP-1 receptors, dopamine transporters, and serotonin pathways can influence individual responses to medications like semaglutide and tirzepatide. Integrating genetic insights with detailed dietary phenotyping enables clinicians to customize treatment plans that maximize efficacy and minimize adverse effects.
For example, patients with polymorphisms linked to reduced GLP-1 receptor sensitivity may require adjusted dosing or adjunctive therapies to achieve desired satiety effects. Meanwhile, nutritional genomics can identify specific macronutrient preferences or intolerances, allowing dietitians to design meal plans that complement pharmacotherapy by stabilizing glycemic responses and supporting gut microbiome diversity.
What Role Does the Gut Microbiome Play in Mediating Appetite Medication Effectiveness?
The gut microbiome has surfaced as a pivotal modulator of metabolic health and appetite regulation. Recent clinical trials indicate that GLP-1 receptor agonists can alter microbial composition, promoting taxa associated with improved insulin sensitivity and reduced inflammation. Conversely, baseline microbiome diversity may predict therapeutic responsiveness.
Interventions such as prebiotic supplementation or targeted probiotics hold promise for enhancing medication outcomes by fostering a gut environment conducive to optimal hormone signaling and nutrient absorption, as detailed in a comprehensive review in Frontiers in Endocrinology.
Refining Adherence: Overcoming Barriers Through Behavioral Economics and Digital Health Integration
Adherence to appetite medications can be undermined by factors such as side effects, psychological resistance, or lifestyle incongruities. Behavioral economics principles applied to medication regimens—like leveraging commitment devices and immediate rewards—have shown promise in enhancing persistence.
Furthermore, digital health platforms offering real-time feedback, telemedicine consultations, and AI-driven personalized coaching are revolutionizing patient engagement. These technologies enable dynamic adjustments to treatment protocols in response to evolving patient data, optimizing therapeutic trajectories.
For clinicians and patients alike, embracing these integrative solutions transforms appetite management from a static prescription into a responsive, patient-centered journey.
Invitation to Dialogue: Share Your Experiences and Expand the Collective Wisdom
As we continue to unravel the intricate interplay between medication, neurobiology, and lifestyle, your insights become invaluable. Have you noticed shifts in cravings or mood that align with your medication schedule? How have personalized nutrition or digital tools influenced your appetite control? Engage with our expert community by sharing your narrative and questions below, and explore our in-depth resources for advanced appetite management strategies.
When the Brain Rewires: Exploring Neuroplasticity’s Role in Sustained Appetite Control
While the immediate appetite-suppressing effects of GLP-1 receptor agonists like semaglutide and tirzepatide are well-documented, a burgeoning body of research suggests these medications may catalyze longer-term neural adaptations. This neuroplasticity—essentially the brain’s ability to reorganize synaptic connections—could underlie sustained improvements in appetite regulation beyond pharmacological action alone. A 2024 study published in Neuroscience Letters revealed that prolonged GLP-1 therapy enhances synaptic strength in hypothalamic circuits, potentially recalibrating hunger and satiety signaling pathways.
Such findings open exciting avenues for integrating cognitive behavioral therapies that capitalize on this neural flexibility, reinforcing healthier eating patterns during critical periods of brain remodeling. For individuals navigating complex cravings and habitual overeating, understanding this neurobiological interplay can empower more nuanced treatment expectations and strategies.
Precision Medicine in Appetite Management: Pharmacogenomics and Personalized Nutrition
Appetite control is not a uniform experience; genetic variability profoundly influences response to appetite-suppressing medications. Pharmacogenomic profiling—analyzing gene variants affecting GLP-1 receptor sensitivity, dopamine transport, and serotonin pathways—enables clinicians to tailor both drug selection and dosing with unprecedented accuracy. This molecular-level customization is complemented by personalized nutrition plans informed by nutrigenomics, which assess how individual genetic makeup modulates macronutrient metabolism and glycemic responses.
For example, patients harboring specific polymorphisms associated with diminished GLP-1 receptor responsiveness may benefit from adjunctive therapies or modified dosing regimens. Meanwhile, nutritionists can optimize meal composition and timing to synergize with pharmacotherapy, enhancing overall efficacy. This integrated approach maximizes therapeutic outcomes while minimizing side effects, advancing the frontier of individualized appetite management.
How Can Digital Health Technologies Amplify the Integration of Medication, Behavioral Interventions, and Personalized Nutrition?
Digital health innovations are revolutionizing appetite management by seamlessly synchronizing pharmacotherapy, behavioral support, and nutritional guidance. AI-driven platforms provide real-time monitoring of medication adherence, symptom tracking, dietary intake, and physical activity, enabling dynamic treatment adjustments tailored to evolving patient needs.
Moreover, telemedicine consultations foster continuous clinician-patient collaboration, while gamification and behavioral economics principles embedded in mobile apps incentivize adherence and lifestyle modification. These technologies create a responsive ecosystem that transforms static prescriptions into adaptive, patient-centered journeys.
For practical insights on harmonizing medication with lifestyle changes, explore expert guidance on mastering prescription injection weight loss with medical guidance. Your experience and questions are vital—share your journey in the comments to enrich our collective understanding and support.

Behavioral Economics Meets Appetite Control: Nudging Toward Better Adherence and Outcomes
Adherence challenges remain a persistent barrier to the success of appetite medications. Integrating behavioral economics strategies—such as commitment devices, immediate positive reinforcement, and loss aversion incentives—can significantly improve persistence. For instance, setting up personalized reward systems or leveraging social accountability mechanisms helps patients stay motivated through common hurdles like side effects or lifestyle incongruities.
Healthcare providers increasingly incorporate these principles alongside digital tools to foster sustainable behavioral change, underscoring that appetite management is as much a psychological endeavor as a pharmacological one.
Expert Insights & Advanced Considerations
Neuroplasticity as a Therapeutic Ally in Sustained Appetite Control
Recent research reveals that GLP-1 receptor agonists like semaglutide and tirzepatide may induce neuroplastic changes within hypothalamic circuits, enhancing synaptic strength and recalibrating hunger and satiety pathways. This suggests that beyond their immediate pharmacological effects, these medications facilitate a biological substrate for lasting behavioral adaptation when paired with cognitive interventions.
Pharmacogenomic Profiling Enhances Personalization of Appetite Medication Regimens
Genetic variability in GLP-1 receptor sensitivity and neurotransmitter pathways significantly impacts individual responses to appetite-suppressing therapies. Integrating pharmacogenomic data allows clinicians to optimize dosing and select adjunctive treatments, thereby maximizing efficacy while minimizing adverse effects and tailoring nutrition plans to genetic metabolic profiles.
Behavioral Economics and Digital Health Synergize to Improve Medication Adherence
Incorporating behavioral economics strategies such as commitment devices and immediate reinforcement through digital health platforms increases persistence with appetite medications. AI-driven monitoring combined with telemedicine and gamification fosters dynamic, patient-centered treatment adjustments, transforming appetite management into an interactive, responsive process.
Synchronizing Meal Timing with Injection Schedules Optimizes Metabolic Outcomes
Strategic alignment of meals and snacks with the pharmacodynamics of GLP-1 receptor agonists prevents glycemic dips that provoke hunger spikes and reduces side effects like nausea. This precision timing supports better appetite regulation and enhances medication tolerability, emphasizing the importance of coordinated lifestyle and pharmacological approaches.
Gut Microbiome Modulation as an Emerging Factor in Medication Responsiveness
Appetite medications influence gut microbial composition, promoting taxa linked to improved insulin sensitivity and reduced inflammation. Baseline microbiome diversity may predict therapeutic responsiveness, and adjunctive interventions such as prebiotics or probiotics hold promise for amplifying treatment benefits by optimizing the gut-brain axis.
Curated Expert Resources
- Obesity Reviews (2023): Comprehensive analyses of combined pharmacotherapy and behavioral interventions for appetite control, providing evidence-based guidance on integrated treatment plans.
- Neuroscience Letters (2024): Cutting-edge studies on neuroplasticity induced by GLP-1 therapies, illuminating mechanisms underlying sustained appetite regulation.
- Frontiers in Endocrinology: Authoritative reviews on the gut microbiome’s role in metabolic health and its interaction with appetite-suppressing medications.
- eWeightLossTips.com Expert Guides: Practical advice on meal timing, injection technique, and behavioral strategies such as balancing energy and appetite with tirzepatide and mastering prescription injection weight loss with medical guidance.
- Pharmacogenomics Research Journals: For those seeking molecular-level insights into personalized medicine approaches in appetite control.
Final Expert Perspective
Appetite management medications represent a sophisticated intersection of neurobiology, genetics, and behavioral science. Understanding their role beyond simple appetite suppression—recognizing neuroplasticity’s potential, leveraging pharmacogenomic insights, and integrating behavioral economics through digital health—empowers both clinicians and patients to optimize outcomes. Coordinated meal timing and attention to the gut microbiome further refine therapeutic impact, underscoring that medication is one component of a multifaceted strategy.
For professionals and informed individuals seeking to deepen their expertise, embracing these advanced perspectives on appetite management will facilitate more effective, personalized interventions. Engage with our community to share experiences or explore nuanced guidance in areas such as personalized treatment plans and combining diet with injections. Your insights contribute to evolving the art and science of appetite control.

This article provides a thoughtful perspective on how appetite-managing medications like semaglutide and tirzepatide are valuable tools rather than quick fixes. I appreciate the emphasis on medication as partners in a comprehensive lifestyle strategy. From my experience, it’s not only about the medication but also developing mindful eating habits and managing stress, which really influence hunger signals. What stood out to me was the point about synchronizing meals with medication timing—this seems like a practical yet often overlooked factor that can smooth out blood sugar dips and reduce hunger spikes. I’ve struggled with unpredictable cravings in the afternoons, and aligning my snack times more closely with my medication schedule has helped me feel less overwhelmed by hunger. I’m curious if others have found meal timing to make a significant difference, and how they balance this with daily routines or social eating occasions? Also, how do you incorporate physical activity and stress management into your regimen alongside medication? Sharing these real-life strategies seems crucial because, as the post notes, managing appetite is deeply personal and multifaceted, extending far beyond just taking a pill.