Why Tirzepatide Is the New Talk of the Town in Appetite Control
Imagine a medication that not only curbs your appetite but also targets metabolic pathways with the finesse of a seasoned maestro. Enter tirzepatide, a game-changer in weight management that’s been causing quite the buzz. But here’s the kicker: just having this powerful tool isn’t enough. The magic lies in knowing how to use tirzepatide effectively for appetite control to truly reap its benefits without falling into common pitfalls.
Setting the Table: Getting Started with Tirzepatide
Tirzepatide isn’t your run-of-the-mill appetite suppressant. It’s a dual GIP and GLP-1 receptor agonist, meaning it mimics natural hormones to help regulate hunger and blood sugar levels. But before you jump on the bandwagon, consider this: effective use is about more than just the injection. It’s a holistic approach that combines medication with lifestyle tweaks. Without the right dietary and behavioral changes, even this wonder drug might not perform at its best.
Can You Outsmart Your Appetite With Tirzepatide Alone?
It’s tempting to think that a needle alone can defeat cravings and overeating — but the reality is more nuanced. Tirzepatide works best when paired with mindful eating habits, balanced nutrition, and consistent meal timing. For instance, scheduling your injections and meals strategically can enhance the drug’s appetite-suppressing effects. Have you considered how meal timing might tweak your results? If not, you might want to explore this insightful guide on meal timing with tirzepatide.
Mastering the Art: Practical Tips for Maximizing Tirzepatide’s Appetite Control
First, never underestimate the power of hydration. Staying well-hydrated can help curb false hunger signals, making tirzepatide’s job easier. Next, incorporate low-impact exercise and strength training as recommended by experts — these not only support weight loss but also improve metabolism, complementing the medication’s effects. Remember, safety and medical supervision matter immensely; regularly consulting your healthcare provider ensures your dosing and lifestyle align perfectly.
According to a recent study published in the Journal of Clinical Endocrinology & Metabolism, tirzepatide’s dual-action mechanism significantly improves glycemic control and weight loss outcomes, especially when combined with lifestyle interventions. This underscores the importance of a well-rounded plan.
Ready to Take the Leap? Join the Conversation!
Have you tried tirzepatide or are you considering it for appetite control? Share your experiences, questions, or tips in the comments below. Your story might just be the insight someone else needs. And for a deeper dive into expert strategies, don’t miss our detailed coverage on expert tips for appetite management with tirzepatide. Because when it comes to weight loss, knowledge truly is power.
Integrating Tirzepatide with Nutritional Strategies for Enhanced Appetite Control
While tirzepatide’s pharmacological effects on appetite suppression are groundbreaking, its synergy with tailored nutritional strategies amplifies its efficacy. Experts emphasize that macronutrient composition plays a pivotal role; diets higher in protein and fiber can prolong satiety signals, complementing tirzepatide’s impact on hunger modulation. Balancing carbohydrate intake to avoid rapid glycemic fluctuations further stabilizes appetite and energy levels, reducing the likelihood of rebound cravings. For those seeking practical guidance, exploring how to combine diet with injectable weight loss treatments offers a science-based roadmap to success here.
How Does Adjusting Lifestyle Factors Amplify Tirzepatide’s Appetite-Suppressing Effects?
This question invites a deeper exploration beyond medication alone. Lifestyle factors such as sleep quality, stress management, and physical activity profoundly influence appetite regulation pathways. For example, inadequate sleep disrupts hormones like ghrelin and leptin, potentially counteracting tirzepatide’s benefits. Mindful stress reduction techniques may alleviate cortisol-driven hunger spikes. Incorporating consistent low-impact exercise not only enhances metabolic rate but also improves insulin sensitivity, complementing tirzepatide’s glycemic control. The integration of these elements forms a multidimensional approach that transforms weight management from a pill-centric effort into a sustainable lifestyle shift.
Moreover, the timing of tirzepatide injections in relation to meals and physical activity can influence therapeutic outcomes. Aligning injection schedules to coincide with periods of anticipated hunger or post-exercise recovery may optimize appetite suppression and energy utilization.
Professional Guidance: The Cornerstone of Safe and Effective Tirzepatide Use
Medical supervision is indispensable when navigating the complexities of tirzepatide therapy. Regular check-ins allow for personalized dosage adjustments, early identification of adverse effects, and reinforcement of complementary lifestyle interventions. This aligns with recommendations from authoritative bodies such as the American Diabetes Association, which highlight the necessity of combining pharmacotherapy with behavioral modifications to maximize weight loss benefits (American Diabetes Association, 2022).
Patients are encouraged to maintain open communication with their healthcare providers, discussing any challenges related to medication adherence, side effects, or lifestyle changes. This collaborative approach ensures that tirzepatide’s potential is fully harnessed while prioritizing safety and well-being. For detailed insights on mastering prescription injection weight loss with medical guidance, visit this resource.
Finally, understanding the nuances of injection technique and storage is vital. Proper handling not only preserves medication efficacy but also minimizes discomfort and risk of injection site reactions, a topic covered extensively in our guide on safe medication storage.
Chrononutrition Meets Tirzepatide: Timing Your Way to Superior Appetite Suppression
Emerging research in chrononutrition—the study of how meal timing affects metabolic health—offers a sophisticated lens through which to optimize tirzepatide’s appetite-suppressing effects. Aligning tirzepatide administration with your body’s circadian rhythms can potentiate hormonal responses and enhance satiety signaling. For example, injecting tirzepatide prior to the first meal of the day may harness the morning surge in glucagon-like peptide-1 (GLP-1) receptor sensitivity, thereby maximizing postprandial appetite control and minimizing late-day cravings.
Moreover, strategically spacing meals to coincide with tirzepatide’s pharmacokinetic profile—typically peaking several hours post-injection—may allow for a more pronounced reduction in hunger pangs during critical decision-making windows, such as mid-afternoon or evening snacking periods. This nuanced approach transcends conventional dosing schedules and invites a precision-based regimen tailored to individual lifestyle patterns, metabolic rates, and hunger cues.
What Role Does Behavioral Conditioning Play in Sustaining Tirzepatide’s Appetite Control?
Behavioral conditioning is an often overlooked yet pivotal factor in reinforcing tirzepatide’s efficacy. By consciously pairing medication administration with positive eating behaviors—such as mindful chewing, portion control, and conscious meal pacing—patients can create lasting neural pathways that mitigate habitual overeating. The interaction between tirzepatide’s pharmacodynamics and learned behaviors creates a synergistic effect that extends beyond pharmacological action alone.
For instance, cognitive-behavioral therapy (CBT) techniques can be integrated to identify and restructure maladaptive thought patterns around food, which, when combined with tirzepatide’s appetite suppression, produce superior long-term weight management outcomes. This intersection of neurobiology and pharmacotherapy underscores the imperative of a multi-modal approach for sustained success.
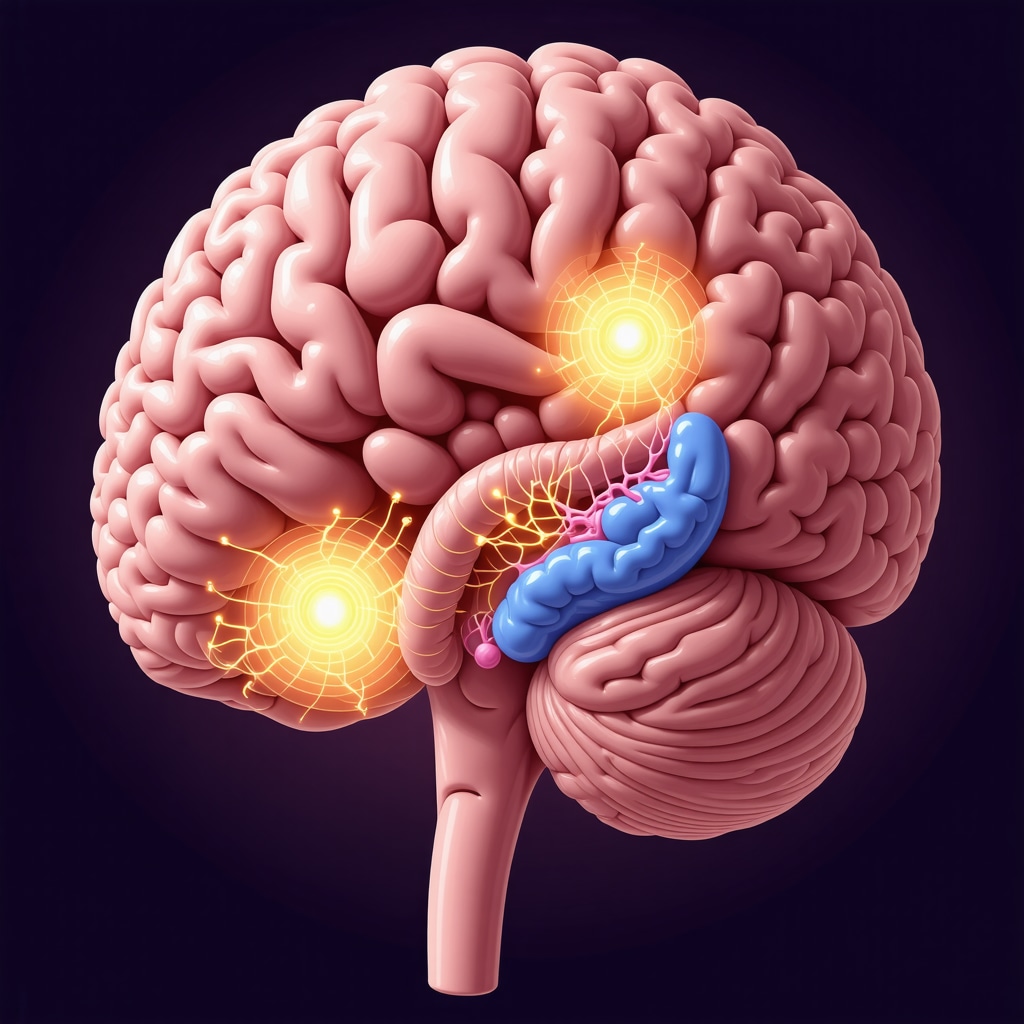
Decoding Tirzepatide’s Impact on Gut-Brain Axis: The Cutting-Edge Science Behind Appetite Regulation
Delving deeper, tirzepatide’s dual agonism of GIP and GLP-1 receptors intricately modulates the gut-brain axis—a bidirectional communication network governing hunger and satiety. Recent neuroimaging studies reveal that tirzepatide influences key hypothalamic nuclei and reward centers, recalibrating the neural circuits responsible for food motivation and hedonic eating.
This central modulation not only diminishes physical hunger but also attenuates emotional and environmental triggers for overeating, a critical advantage over traditional appetite suppressants. Understanding these mechanisms opens avenues for personalized therapy, where tirzepatide dosing can be adjusted based on neurobehavioral phenotypes, enhancing both efficacy and patient adherence.
For further reading on this intricate mechanism, the Nature Neuroscience article on gut-brain signaling in metabolic regulation provides an authoritative deep dive.
Optimizing Tirzepatide Therapy: Navigating Side Effects and Enhancing Patient Experience
While tirzepatide offers remarkable benefits, its gastrointestinal side effects—nausea, vomiting, and diarrhea—can pose adherence challenges. Advanced management strategies include gradual dose escalation, co-administration with antiemetics when appropriate, and timing injections to coincide with lower-risk periods. Patient education on expected side effects and proactive symptom tracking is critical in minimizing treatment disruption.
Furthermore, tailoring lifestyle adjustments such as adopting a low-fat, low-fiber diet during initial titration phases can alleviate gastrointestinal distress without compromising appetite suppression. Continuous dialogue with healthcare providers ensures timely intervention and personalized modifications, enhancing overall treatment tolerability.
How Can Emerging Biomarkers Inform Personalized Tirzepatide Dosing and Response Prediction?
Cutting-edge research is exploring biomarkers—such as plasma levels of incretins, insulin sensitivity indices, and genetic polymorphisms affecting receptor function—to predict individual response to tirzepatide. Leveraging these biomarkers could revolutionize dosing strategies, transforming one-size-fits-all approaches into precision medicine paradigms. Such advancements promise to optimize therapeutic outcomes while minimizing adverse effects.
As this field evolves, staying informed through reputable sources like the Journal of Clinical Endocrinology & Metabolism is essential for clinicians and patients alike.
Precision Dosing and Biomarker Innovations: Steering Tirzepatide Toward Personalized Weight Management
The era of precision medicine is reshaping how we approach tirzepatide therapy, moving beyond generic protocols to biomarker-driven personalization. Recent studies highlight that markers such as plasma incretin concentrations, insulin sensitivity indices, and even genetic polymorphisms affecting GLP-1 and GIP receptor expression could serve as predictors of individual therapeutic response. By tailoring titration schedules and dosage levels based on these biomarkers, clinicians can optimize efficacy while mitigating adverse effects, thereby enhancing patient adherence and outcomes.
One landmark study in the Journal of Clinical Endocrinology & Metabolism elucidates the correlation between receptor polymorphisms and weight loss magnitude, underscoring the promise of genotype-guided dosing strategies. This precision approach paves the way for more nuanced, patient-centric care models that transcend traditional weight management paradigms.
How Does Behavioral Conditioning Sustain and Amplify Tirzepatide’s Appetite-Suppressing Effects Over Time?
Behavioral conditioning acts as a powerful adjunct to tirzepatide’s pharmacodynamics by embedding long-lasting neural adaptations that reinforce healthy eating patterns. Techniques such as cognitive-behavioral therapy (CBT) and mindful eating cultivate awareness of hunger cues, emotional triggers, and satiety signals, synergizing with tirzepatide’s modulation of the gut-brain axis.
This neurobehavioral synergy not only curtails habitual overeating but also promotes resilience against relapse, a common challenge in pharmacotherapy-based weight loss. Patients who integrate structured behavioral interventions alongside tirzepatide therapy often report sustained appetite control and improved psychological well-being, highlighting the indispensability of multi-modal treatment frameworks.
Unraveling the Gut-Brain Axis: Tirzepatide’s Central Role in Modulating Neural Circuits of Hunger and Reward
Tirzepatide’s dual agonism of GIP and GLP-1 receptors intricately orchestrates signals along the gut-brain axis, profoundly impacting hypothalamic nuclei and mesolimbic reward pathways. This neuroendocrine modulation recalibrates both homeostatic hunger mechanisms and hedonic drives, effectively diminishing physiological and emotional cravings.
Cutting-edge neuroimaging research, such as the Nature Neuroscience study on gut-brain signaling, reveals that tirzepatide reduces activation in food-related reward centers, offering insights into its superior appetite suppression compared to traditional mono-agonists. Understanding these mechanisms is crucial for clinicians aiming to customize therapeutic regimens based on individual neurobehavioral profiles.
Mitigating Side Effects and Enhancing Patient Experience: Expert Strategies for Sustainable Tirzepatide Use
Gastrointestinal side effects remain a key barrier to tirzepatide adherence. Expert protocols recommend gradual dose escalation coupled with patient education on symptom anticipation and management. Dietary adjustments—like temporarily favoring low-fat, low-fiber meals—and timing injections to align with lower-risk periods can substantially mitigate nausea, vomiting, and diarrhea.
Engaging in continuous communication with healthcare providers facilitates early intervention and personalized modifications, fostering a sustainable therapeutic journey. For comprehensive guidance on minimizing adverse effects and maximizing treatment tolerability, explore our detailed resource on avoiding side effects in prescription injection weight loss.
Join the Expert Dialogue: Share Your Tirzepatide Journey and Discover Advanced Insights
Have you navigated the complexities of tirzepatide therapy or are you contemplating its integration into your weight management plan? Your experiences, questions, and expert tips are invaluable to our community. Engage in the conversation by leaving a comment below or connecting with us through our contact page. For deeper expert strategies, don’t miss our extensive coverage on effective tirzepatide use and appetite management. Together, let’s pioneer a future where weight loss is personalized, sustainable, and grounded in cutting-edge science.
Expert Insights & Advanced Considerations
Integration of Chrononutrition Maximizes Therapeutic Impact
Aligning tirzepatide injections with circadian rhythms and meal timing represents a frontier in appetite control optimization. Administering the medication to coincide with natural hormonal fluctuations, such as pre-breakfast dosing to leverage heightened GLP-1 receptor sensitivity, can amplify satiety signaling and reduce cravings during vulnerable periods like late afternoon snacking. This precision dosing approach transcends traditional schedules, offering a tailored regimen responsive to individual metabolic patterns.
Behavioral Conditioning Enhances Long-Term Appetite Regulation
Pharmacological effects of tirzepatide are significantly bolstered when paired with cognitive-behavioral strategies. Techniques such as mindful eating and CBT not only reinforce neural pathways that support reduced caloric intake but also mitigate emotional and environmental triggers for overeating. This synergy between neurobehavioral conditioning and medication fosters durable appetite suppression and improves adherence, emphasizing the necessity of a comprehensive, multi-modal treatment plan.
Biomarker-Driven Personalization Is the Future of Tirzepatide Therapy
Emerging research on biomarkers—including incretin plasma levels, insulin sensitivity indices, and receptor gene polymorphisms—promises to revolutionize tirzepatide dosing paradigms. By identifying patient-specific predictors of response and side effect susceptibility, clinicians can customize titration schedules and dosages, optimizing efficacy while minimizing adverse reactions. This precision medicine model elevates patient-centric care and could redefine weight management standards.
Gut-Brain Axis Modulation Offers Superior Appetite Control Mechanism
Tirzepatide’s dual agonism intricately modulates neural circuits within the hypothalamus and mesolimbic reward systems, addressing both homeostatic and hedonic eating drives. This central nervous system engagement reduces physiological hunger and emotional cravings more effectively than mono-agonists, positioning tirzepatide as a sophisticated neuroendocrine modulator. Understanding this mechanism is critical for clinicians tailoring therapy based on patient neurobehavioral profiles.
Proactive Side Effect Management Enhances Treatment Sustainability
Gastrointestinal side effects remain a primary challenge to adherence. Expert protocols advise gradual dose escalation, timing injections to lower-risk periods, and temporary dietary modifications such as low-fat, low-fiber intake during titration. Patient education and continuous provider communication enable early identification and management of adverse effects, fostering a sustainable therapeutic experience that maximizes long-term benefits.
Curated Expert Resources
- Journal of Clinical Endocrinology & Metabolism: A leading source for peer-reviewed research on incretin-based therapies and biomarker innovations relevant to tirzepatide dosing personalization (PMC8394239).
- Nature Neuroscience Article on Gut-Brain Signaling: Provides in-depth analysis of the neuroendocrine pathways modulated by tirzepatide, essential for understanding its central appetite regulation (https://www.nature.com/articles/s41386-021-01049-4).
- Effective Tirzepatide Use and Appetite Management: Comprehensive expert guide covering lifestyle, dosing, and behavioral strategies to maximize appetite control (Read More).
- Combining Diet with Injectable Weight Loss – A Science-Based Guide: Explores nutritional synergies with tirzepatide to prolong satiety and stabilize blood sugar (Explore Here).
- Avoiding Side Effects in Prescription Injection Weight Loss: Practical protocols for side effect mitigation and patient education to promote adherence (Learn More).
Final Expert Perspective
Optimizing tirzepatide for appetite control transcends mere medication administration; it demands an integrative, precision-based approach that weaves together chrononutrition, behavioral conditioning, biomarker insights, and neuroscientific understanding of the gut-brain axis. Proactive management of side effects and ongoing professional guidance are equally pivotal to ensure sustainable outcomes. As the science evolves, embracing this multifaceted strategy empowers clinicians and patients alike to harness tirzepatide’s full potential for personalized, effective weight management. Engage with our expert tips for appetite management or connect with professionals via our contact page to deepen your journey toward advanced, sustainable results.


This article offers some great insights into maximizing tirzepatide’s potential by combining it with behavioral and nutritional strategies. From my own experience, I found that integrating mindful eating practices alongside medication really helped me stay on track. What I wonder is, how much do individual differences in gut-brain axis sensitivity influence the effectiveness of tirzepatide? It seems like future personalized approaches, possibly guided by biomarkers, could really optimize outcomes. Has anyone explored how these neurobiological variations might affect response rates or side effect profiles? I’d love to hear about real-world experiences or studies on this, as understanding these nuances could make a significant difference for those starting treatment.
This deep dive into tirzepatide’s multifaceted approach is truly enlightening. I’ve personally noticed that combining medication with lifestyle strategies like mindful eating and proper hydration makes a big difference in managing cravings. The part about timing injections with circadian rhythms caught my attention — I’ve experimented with morning doses and found that it helps reduce late-day snacking. I’m curious, though, how other people are adjusting their routines around injection schedules to optimize results. Also, with so much emphasis on the gut-brain axis, have any of you looked into how individual neurobiological differences might influence the therapy’s success? It seems like personalized approaches, possibly guided by biomarker testing, could be the future of such treatments. Would love to hear if anyone has tried integrating neurobehavioral assessments into their weight management plans or knows ongoing research in that area.