Is Your Fat Loss Journey Missing a Piece of the Puzzle?
Picture this: you’re diligently counting calories, hitting the gym, and yet the scale refuses to budge. Frustrating, isn’t it? Now, imagine adding a secret weapon—prescription medications like GLP-1 receptor agonists—into your arsenal. The synergy between diet and medication can turbocharge your fat loss results, but only when managed wisely. Let’s dive into how to incorporate these tools seamlessly into your weight loss saga.
The Dynamic Duo: Diet & Medication—A Match Made in Fat Loss Heaven
When it comes to shedding stubborn fat, relying solely on diet can sometimes feel like fighting an uphill battle. Enter medications such as semaglutide or tirzepatide, which have revolutionized weight management. These drugs help suppress appetite and regulate blood sugar, making your dietary efforts more effective. But here’s the catch: combining them without guidance can be risky. That’s where expert advice and tailored plans come into play.
Why Not Just Eat Less and Hope for the Best?
Good question! While calorie restriction is fundamental, the body’s adaptive mechanisms—like increased hunger and metabolic slowdown—can sabotage your efforts. Medications help counteract these responses by modulating hunger signals, effectively resetting your body’s weight loss thermostat. This balanced approach ensures you’re not fighting your biology alone.
For instance, studies show that integrating GLP-1 medications with a controlled diet leads to more significant and sustainable weight loss (source: Science Magazine). It’s akin to upgrading from a bicycle to a motorcycle—speedier progress with better control.
Getting the Mix Right: Practical Tips for Combining Diet & Medication
- Consult Your Healthcare Provider: Never start or stop medication without professional oversight. They can tailor the regimen to your needs and monitor for side effects.
- Focus on Nutrient-Dense Foods: Fuel your body with quality nutrients to support medication efficacy and overall health.
- Stay Consistent: Adherence to both diet and medication schedules maximizes results and minimizes risks.
- Monitor and Adjust: Regular check-ins with your doctor allow adjustments for optimal outcomes.
Are You Ready to Take Control of Your Fat Loss?
If you’re contemplating combining diet and medication, remember that success hinges on expert guidance and personalized plans. Share your experiences or ask questions in the comments below—your journey might inspire others!
Can you truly optimize your fat loss results by integrating diet and medication?
Many individuals embarking on weight loss journeys wonder if there’s a way to accelerate their progress beyond traditional dieting. The answer is a resounding yes—when guided by medical expertise and a nuanced understanding of how these tools work together. Combining a carefully crafted diet plan with prescription medications such as GLP-1 receptor agonists can create a synergistic effect that amplifies fat loss and sustains your results.
The Science Behind Synergy: Why Combining Diet & Medication Works
Research indicates that pairing dietary changes with medications like semaglutide or tirzepatide significantly enhances weight loss outcomes. These medications act on appetite centers in the brain, reducing hunger and cravings, which makes sticking to calorie-controlled diets easier. Meanwhile, a nutrient-rich, balanced diet ensures your body gets essential nutrients, supports metabolic health, and minimizes potential side effects from medications.
As highlighted by science, such combined approaches leverage both behavioral and biological mechanisms, making weight management more effective and sustainable (Science Magazine).
What if your body fights back against your efforts—how can medications help reset your weight loss set point?
This question touches on a critical aspect of weight management—homeostasis. Our bodies tend to defend against weight loss by increasing hunger and decreasing energy expenditure, a phenomenon often called the body’s “set point.” Medications like GLP-1 agonists can help recalibrate this set point by suppressing appetite signals, making it easier to maintain a calorie deficit without constant willpower battles. Combining this with lifestyle modifications creates a more resilient weight loss strategy, one that addresses both the biological and behavioral hurdles.
Practical Strategies for a Harmonized Approach
- Partner with Healthcare Professionals: Personalized guidance ensures your medication and diet plan are safe and effective. Regular check-ins help tailor your approach as you progress.
- Prioritize Nutrient-Dense Foods: Whole foods rich in fiber, healthy fats, and lean proteins support medication efficacy and overall health.
- Adhere Rigorously: Consistency in medication schedules and dietary routines maximizes results and reduces risks.
- Monitor Progress and Side Effects: Regular assessments allow for timely adjustments, ensuring safety and success.
Incorporating these strategies requires a dedicated partnership with your healthcare team. For more detailed guidance, explore mastering prescription injection weight loss with medical guidance.
Are you ready to embrace a smarter, science-backed path to lasting fat loss?
If you’re considering this integrated approach, sharing your questions or experiences can be incredibly valuable. Comment below or reach out through our contact page. Remember, combining the right dietary strategies with medical support isn’t just about losing weight; it’s about transforming your relationship with health and wellness for the long term.
Leveraging Neuromodulation and Hormonal Pathways: Cutting-Edge Approaches to Fat Loss Synergy
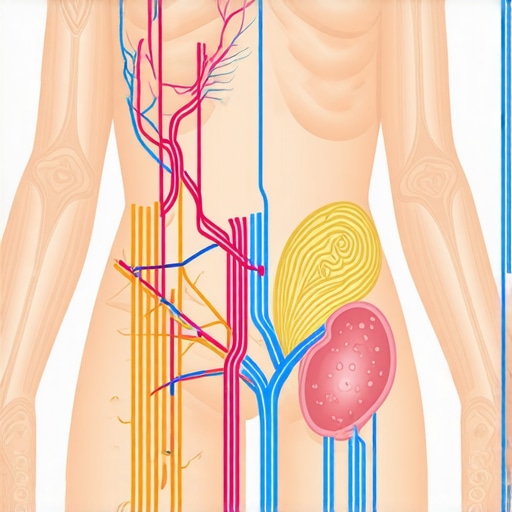
As we delve deeper into optimizing fat loss, understanding the neuroendocrine mechanisms becomes paramount. Recent research highlights the role of neuromodulation—such as vagus nerve stimulation—and its influence on appetite regulation and metabolic rate. Combining these innovative interventions with pharmacological agents like GLP-1 receptor agonists can potentially create a more robust and sustainable weight management strategy. For instance, targeted neuromodulatory techniques may enhance the efficacy of medications by further dampening hunger signals and promoting energy expenditure.
Can neuromodulation amplify the effects of pharmacotherapy in weight loss?
Emerging evidence from clinical studies suggests that neuromodulation can synergistically enhance drug effects, leading to greater fat loss and improved metabolic health. A notable example is the application of transcutaneous vagus nerve stimulation, which has shown promise in reducing appetite and improving insulin sensitivity (source: SAGE Journals). Integrating these modalities requires precision and a personalized approach, emphasizing the importance of interdisciplinary collaboration in weight management.
Tailoring Hormonal Modulation for Long-Term Weight Stability
Beyond appetite suppression, hormonal modulation—such as manipulating leptin, ghrelin, and adiponectin—offers avenues to recalibrate the body’s weight set point. Advanced therapeutic strategies include leveraging peptide-based therapies and gene editing techniques to optimize hormonal balances. For example, recombinant leptin therapy, although limited in general obesity, shows potential in specific syndromic cases and could inspire future personalized treatments. The goal is to shift the body’s homeostatic weight point, making sustainable fat loss more achievable.
How can personalized hormonal therapies redefine long-term weight management?
By tailoring hormonal interventions based on individual metabolic profiles, clinicians can address specific dysregulations that impede weight loss efforts. Precision medicine approaches—using biomarkers and genetic testing—are revolutionizing this field, enabling targeted therapies that align with each person’s unique physiology (source: Nature Medicine). This paradigm shift moves us beyond one-size-fits-all solutions towards highly individualized strategies that promote durable results.
If you’re interested in exploring cutting-edge, personalized fat loss strategies, consider consulting with a specialist who can integrate these innovative modalities into your health plan. Deepening your understanding of neuroendocrine dynamics and hormonal modulation could be the game-changer in your journey toward lasting weight management.
Harnessing Neuroendocrine Insights: Can Neuromodulation Supercharge Your Fat Loss?
Emerging research suggests that neuromodulation techniques—such as vagus nerve stimulation—may significantly influence appetite regulation and metabolic enhancement, opening new frontiers in weight management. When integrated with pharmacological agents like GLP-1 receptor agonists, these interventions can produce a synergistic effect, potentially leading to more profound and sustained fat loss. Experts believe that targeting neural pathways involved in hunger and satiety could amplify the biological impact of medications, making the journey toward your ideal weight more efficient.
How does neuromodulation interact with hormonal pathways to optimize fat burning?
Neuromodulatory interventions stimulate specific neural circuits that govern hormonal signals like leptin, ghrelin, and insulin, thereby recalibrating the body’s energy balance set point. For example, transcutaneous vagus nerve stimulation has shown promise in reducing hunger signals and improving insulin sensitivity (SAGE Journals). This dual approach—combining neural modulation and hormonal regulation—can help overcome biological resistance to weight loss, making long-term results more attainable and resilient.
Personalizing Hormonal Therapies for Lasting Weight Stability
Beyond appetite suppression, manipulating hormonal balances—such as leptin, ghrelin, and adiponectin—can recalibrate the body’s intrinsic weight set point. Cutting-edge therapies involve peptide-based treatments and gene editing techniques tailored to individual genetic and metabolic profiles. For instance, recombinant leptin therapy, although currently limited to specific syndromes, exemplifies the potential for hormonal customization in weight management (Nature Medicine). These personalized interventions aim to shift the homeostatic weight point, fostering sustainable fat loss and metabolic health.
What role does precision medicine play in hormonal modulation for weight management?
Precision medicine utilizes biomarkers and genetic profiling to customize hormonal therapies, addressing unique dysregulations that hinder weight loss. This approach enables clinicians to develop targeted strategies—such as tailored peptide therapies or gene editing—that optimize hormonal harmony and promote durable results. As research advances, the integration of these personalized modalities promises a paradigm shift from generic plans to individualized, effective solutions for long-term weight stability.
If you’re eager to explore these innovative, personalized fat loss approaches, consulting with specialists experienced in neuroendocrine therapies can provide tailored guidance. Deepening your understanding of neuroendocrine dynamics and hormonal modulation may be the key to unlocking sustainable success in your weight management journey.
Expert Insights & Advanced Considerations
1. Neuroendocrine Modulation as a Catalyst for Long-Term Success
Emerging evidence underscores the potential of neuromodulation techniques like vagus nerve stimulation to recalibrate appetite regulation and metabolic pathways. Integrating these with pharmacotherapies such as GLP-1 receptor agonists can amplify fat loss outcomes, offering a multi-faceted approach that addresses both neural and hormonal signals.
2. Personalized Hormonal Therapies for Sustainable Results
Advances in biomarker and genetic profiling facilitate tailored hormonal interventions, such as peptide therapies or gene editing, aimed at recalibrating the body’s weight set point. This personalized approach enhances the durability of weight loss, moving beyond one-size-fits-all solutions.
3. The Synergistic Power of Combining Lifestyle, Medication, and Neuroendocrine Strategies
Integrating evidence-based lifestyle modifications with targeted medications and neuromodulation techniques creates a comprehensive, resilient framework for fat loss. This synergy leverages behavioral, biological, and technological advances to overcome resistance mechanisms and sustain results.
4. The Role of Precision Medicine in Future Fat Loss Paradigms
Utilizing biomarkers and genetic insights, precision medicine enables bespoke therapies that target specific dysregulations, optimizing efficacy and safety. This paradigm shift promises more predictable, long-lasting outcomes in weight management.
5. Ethical and Safety Considerations in Advanced Interventions
While cutting-edge therapies offer promising avenues, rigorous safety protocols and ethical oversight are paramount. Continued research and clinical validation are essential to ensure these innovations translate into safe, effective treatments for diverse populations.

