Unlocking the Synergy Between Diet and Injectable Weight Loss Treatments
Embarking on a weight loss journey often involves navigating a maze of options. Among these, injectable weight loss treatments such as GLP-1 receptor agonists have surged in popularity due to their ability to suppress appetite and improve metabolic outcomes. Yet, the true potential of these treatments is realized when combined thoughtfully with a tailored diet plan. This article delves into the expert strategies behind effectively integrating diet with injectable therapies to optimize fat loss, preserve lean muscle, and sustain long-term health benefits.
Precision Nutrition: Crafting a Diet That Amplifies Injectable Therapy
Injectable weight loss medications like semaglutide or tirzepatide modulate appetite hormones and glucose metabolism, but their efficacy can be significantly enhanced through dietary alignment. A diet rich in whole, nutrient-dense foods—emphasizing lean proteins, healthy fats, and fiber—supports satiety and blood sugar stability. For instance, incorporating complex carbohydrates such as quinoa and legumes can prevent energy crashes that might otherwise sabotage adherence to treatment protocols.
Moreover, timing meals around the pharmacodynamics of injectables can mitigate side effects. Taking cues from GLP-1 medication insights, patients are advised to consume smaller, more frequent meals to accommodate reduced gastric motility and nausea sometimes induced by these drugs.
Integrative Approach: Balancing Caloric Intake and Appetite Suppression
While injectable treatments suppress appetite, they do not replace the need for mindful caloric intake. An imbalanced diet—either excessively restrictive or unstructured—can lead to nutrient deficiencies or plateauing weight loss. Experienced clinicians recommend an integrative approach where dietitians and prescribing physicians collaborate to tailor calorie goals that complement injection therapy, ensuring sustainable fat loss without compromising metabolic health.
For practical guidance on balancing injection dosage and diet, see this expert advice.
How Can Patients Optimize Their Weight Loss by Synchronizing Injection Timing with Eating Patterns?
Optimal injection timing plays a pivotal role in maximizing treatment benefits. Research indicates that administering injectables such as semaglutide prior to meals can enhance appetite suppression and reduce caloric intake. Patients should be coached on timing injections to align with their primary eating windows, thereby minimizing hunger and improving meal control. Adhering to a regular schedule also helps stabilize blood glucose levels, a critical factor in long-term weight management.
To deepen your understanding of injection timing and diet coordination, explore these specialized tips.
Real-World Success: Case Study Illuminating Effective Integration
Consider the case of a 45-year-old patient with obesity and insulin resistance who combined a Mediterranean-style diet with weekly semaglutide injections. Within six months, the patient achieved a 15% reduction in body weight, improved glycemic control, and reported sustained appetite regulation. Key to this success was consistent meal planning, hydration, and close follow-up with healthcare providers to adjust injections and dietary intake responsively.
Expert Tips to Navigate Challenges and Enhance Safety
Common challenges include injection site discomfort, gastrointestinal side effects, and managing cravings. Employing physician-approved strategies like rotating injection sites and using pain-reduction techniques can improve adherence. Additionally, incorporating high-fiber foods and probiotics may alleviate digestive symptoms associated with GLP-1 therapies (NIH study on GLP-1 and GI effects).
For comprehensive guidance on combining diet and injectable weight loss treatments safely, visit this expert resource.
Ready to elevate your weight loss journey with a personalized, medically supervised plan? Contact us to connect with specialists who can tailor your injectable and nutrition strategy for optimal results.
Personal Reflections on Sustaining Motivation During Weight Loss
When I first started my journey with injectable weight loss treatments, I noticed that motivation ebbed and flowed in surprising ways. It’s not just about the medication or the diet plan; it’s about how you emotionally connect with the process. Some days, the appetite suppression made it easier to stick to my meal plan; other days, cravings still found a way to sneak in, reminding me that this journey is deeply human.
One strategy that helped me was journaling my food intake and feelings around meals and injections. This not only offered insight into patterns but also helped me celebrate small victories that might otherwise go unnoticed. For instance, recognizing that I handled a social dinner without overeating was a win worth noting.
Adapting Diet Plans With Changing Injection Dosages
Throughout my experience, my healthcare provider adjusted my injection dosages to better suit my progress and tolerance. Each adjustment required me to fine-tune my diet to maintain balance and avoid side effects. Early on, higher doses made me feel a bit nauseous, so I leaned into more frequent, lighter meals with gentle, easy-to-digest foods.
As my body adapted, I gradually reintroduced more variety and volume into my meals, always mindful of how my appetite and digestion responded. This dynamic relationship between dosage and diet underscored the importance of personalized medical supervision, something I highly recommend for anyone using injectable weight loss treatments.
How Do You Find the Right Balance Between Medical Guidance and Your Own Body’s Signals?
Listening to your body while following medical advice can sometimes feel like walking a tightrope. For me, open communication with my healthcare team was key. I made it a point to report not just side effects but also shifts in hunger, energy, and mood. This dialogue allowed for timely tweaks to both injections and nutrition plans.
Research from the National Institutes of Health highlights that patient feedback is crucial in managing gastrointestinal and appetite-related symptoms during GLP-1 therapy, reinforcing that your experience matters just as much as clinical data.
Incorporating Mindful Eating Practices to Complement Injectable Therapy
One unexpected insight for me was how mindful eating became a powerful ally. Paying close attention to hunger cues, savoring each bite, and avoiding distractions during meals helped me better appreciate food and recognize fullness signals sooner. This mindfulness reduced the temptation to overeat, which sometimes creeps in even with medication.
Mindful eating also improved my emotional relationship with food, turning meals into moments of self-care rather than stress or guilt triggers. If you’re curious about integrating mindful habits with your weight loss routine, exploring resources that blend nutrition with behavioral strategies can be incredibly beneficial.
For those interested, you might find practical tips on combining nutrition with injections quite helpful.
Sharing Your Journey: Why Community Support Matters
Weight loss, especially when involving injectable treatments, isn’t just a physical journey but an emotional one. Connecting with others who understand the challenges and triumphs can provide encouragement and accountability. Whether through online forums, support groups, or trusted friends, sharing experiences can ease feelings of isolation.
If you’ve tried combining diet and injectable therapies or are considering it, I’d love to hear about your experiences, challenges, or questions. Feel free to comment below or share this article with anyone who might benefit from these insights. Remember, your journey is unique, and you’re not alone in it.
Precision Timing and Macronutrient Manipulation: Elevating Injectable Treatment Outcomes
Beyond simply aligning injection schedules with meal timing, advanced practitioners emphasize the nuanced manipulation of macronutrient ratios throughout the day to potentiate the pharmacological effects of GLP-1 receptor agonists. For example, increasing protein intake during the injection’s peak activity window can augment satiety signaling and support lean muscle preservation, which is critical for sustaining basal metabolic rate during weight loss.
Experts suggest a strategic distribution of carbohydrates, favoring low-glycemic index sources in the morning to stabilize insulin response, while incorporating moderate healthy fats later in the day to enhance prolonged fullness without compromising lipid profiles. This dynamic macronutrient cycling, tailored to individual metabolic responses, can mitigate common barriers such as gastrointestinal discomfort and energy dips.
What Are the Biochemical Interactions Between Macronutrients and GLP-1 Agonists That Influence Appetite and Metabolism?
GLP-1 receptor agonists engage in complex biochemical pathways that modulate insulin secretion, glucagon suppression, and gastric emptying rates. When combined with specific macronutrient compositions, these effects are either amplified or tempered. For instance, dietary fats tend to slow gastric emptying independently, synergizing with GLP-1 induced motility reduction to extend satiety but may also exacerbate nausea if not carefully balanced.
Conversely, high-protein meals stimulate glucagon release, which may counterbalance some GLP-1 effects on glucose metabolism, necessitating precise dietary calibration to optimize metabolic outcomes (Journal of Clinical Endocrinology & Metabolism).
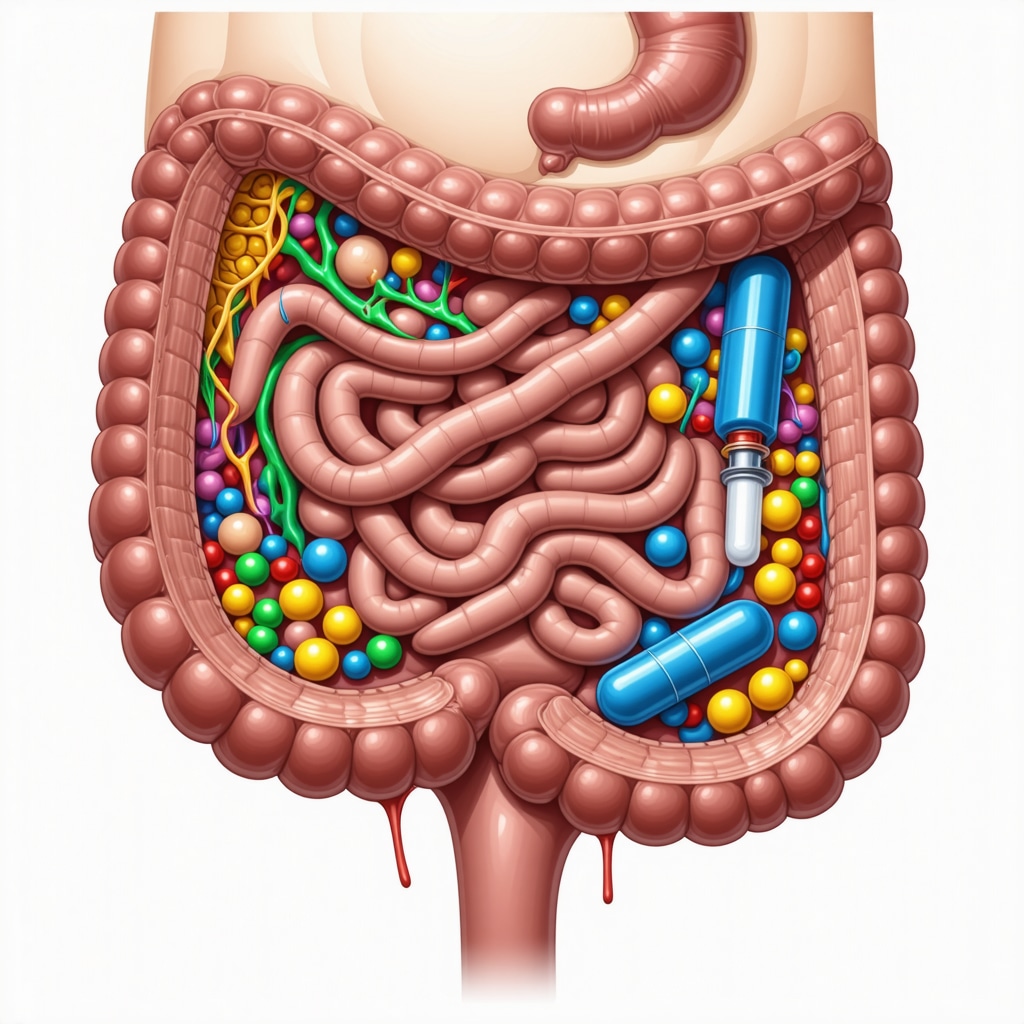
Leveraging Gut Microbiota Modulation to Complement Injectable Weight Loss Therapies
Emerging research highlights the pivotal role of the gut microbiome in mediating the efficacy of weight loss interventions, including GLP-1 analogs. Dietary components such as prebiotics, probiotics, and fermentable fibers can favorably alter microbial diversity and metabolite production, which in turn influence systemic inflammation, insulin sensitivity, and appetite regulation.
In practical terms, integrating fermented foods like kefir or kimchi alongside soluble fiber sources (e.g., oats, apples) can enhance GLP-1 receptor agonist responsiveness by supporting enteroendocrine cell function and gut barrier integrity. This gut-centric approach represents a frontier in personalizing injectable weight loss regimens for superior, sustainable results.
Personalizing Injectable Weight Loss: The Role of Pharmacogenomics and Nutrigenomics
Cutting-edge advancements in pharmacogenomics reveal that genetic variations can influence individual responses to GLP-1 receptor agonists, including variability in appetite suppression and side effect profiles. Concurrently, nutrigenomics sheds light on how specific dietary patterns interact with genetic predispositions to affect metabolism and weight loss trajectories.
Incorporating genetic testing into clinical practice allows for a precision medicine approach—customizing both injectable dosages and diet plans to harmonize with a patient’s unique genetic makeup. This integration has the potential to reduce trial-and-error periods and enhance the efficacy and tolerability of combined therapies.
As a transformative tool, genetic insights empower clinicians and patients to co-create adaptive, evidence-based strategies that maximize fat loss while safeguarding metabolic health.
Interested in exploring how personalized genomics can refine your injectable weight loss journey? Connect with our expert team to discover tailored solutions grounded in the latest scientific advancements.
Decoding the Interplay of Circadian Rhythms and Injectable Weight Loss Efficacy
Recent investigations into chrononutrition underscore the importance of aligning meal timing and injection schedules with the body’s internal clock. Chronobiological synchronization enhances metabolic flexibility and hormonal responses, optimizing the pharmacodynamics of GLP-1 receptor agonists. For example, administering injections during morning hours when endogenous GLP-1 secretion peaks may potentiate appetite suppression and glucose regulation more effectively than evening dosing.
This temporal precision also aligns with nutrient absorption cycles, suggesting that tailoring carbohydrate intake to earlier in the day can prevent postprandial hyperglycemia and reduce insulin resistance risks.
Harnessing Adaptive Exercise Protocols to Complement Injectable and Dietary Interventions
While injectable therapies and diet form the cornerstone of many weight loss plans, incorporating adaptive exercise regimens can synergistically amplify results. High-intensity interval training (HIIT) timed to coincide with peak medication efficacy windows can improve insulin sensitivity and support lean muscle retention, mitigating common metabolic slowing during caloric deficit phases.
Additionally, resistance training focused on muscle hypertrophy helps counteract sarcopenia, a frequent concern with rapid weight loss, enhancing basal metabolic rate and long-term weight maintenance.
How Can Advanced Biomarker Monitoring Refine Injectable Weight Loss and Nutritional Strategies?
Utilizing cutting-edge biomarker panels, including continuous glucose monitors (CGM), appetite hormone assays (like ghrelin and leptin), and inflammatory markers, enables clinicians to dynamically adjust both injectable dosages and dietary macronutrient distributions. By interpreting these biological signals, practitioners can personalize interventions to mitigate side effects, prevent metabolic plateaus, and optimize fat loss kinetics.
According to a comprehensive review in The Journal of Clinical Endocrinology & Metabolism, integrating biomarker feedback loops into treatment protocols represents the frontier of precision obesity medicine.
Embracing Technological Innovations: Digital Health Tools in Injectable Weight Management
Digital platforms incorporating AI-driven dietary tracking, injection reminders, and symptom logging elevate patient engagement and adherence. These tools facilitate real-time communication with healthcare providers, allowing for prompt adjustments and personalized coaching that address individual variability in response to therapy.
Moreover, leveraging machine learning algorithms can predict side effect onset and recommend preemptive dietary modifications, thus enhancing tolerability and outcomes.
What Are the Ethical Considerations Surrounding Genomic Data Utilization in Personalized Weight Loss?
As pharmacogenomics and nutrigenomics become integral to injectable weight loss personalization, the ethical stewardship of genetic data demands rigorous privacy safeguards and informed consent processes. Patients must be apprised of potential risks, including data breaches and genetic discrimination, while benefiting from transparent data usage policies.
Healthcare providers are called to balance innovation with patient autonomy and confidentiality, fostering trust in genomic-guided therapeutic paradigms.
Inspired to explore these advanced, integrative strategies for your weight loss journey? Reach out to our expert team and unlock personalized solutions tailored to your unique biology and lifestyle.
Frequently Asked Questions (FAQ)
What are GLP-1 receptor agonists and how do they aid weight loss?
GLP-1 receptor agonists are injectable medications that mimic the glucagon-like peptide-1 hormone, enhancing insulin secretion, suppressing appetite, and slowing gastric emptying. These combined effects lead to reduced caloric intake and improved metabolic control, thereby promoting weight loss.
How should diet be adjusted when using injectable weight loss treatments?
Diets should emphasize nutrient-dense whole foods with balanced macronutrients—lean proteins, complex carbohydrates, healthy fats, and fiber—to support satiety and metabolic health. Meal timing and portion size adjustments help mitigate side effects like nausea and optimize drug efficacy.
Can meal timing enhance the effectiveness of injectable therapies?
Yes. Administering injections prior to main meals aligns peak drug activity with eating, reducing hunger and caloric intake. Pairing this with smaller, frequent meals can improve tolerance and maintain steady energy levels.
What role does gut microbiota play in injectable weight loss treatment outcomes?
The gut microbiome influences inflammation, insulin sensitivity, and appetite regulation. Dietary components such as probiotics, prebiotics, and fermentable fibers can modulate gut flora to enhance responsiveness to GLP-1 receptor agonists.
How can exercise complement injectable and dietary weight loss strategies?
Adaptive exercise protocols like HIIT and resistance training improve insulin sensitivity, preserve lean muscle mass, and boost basal metabolic rate. Timing exercise to coincide with medication peaks can further potentiate metabolic benefits.
What is the significance of pharmacogenomics and nutrigenomics in personalizing weight loss?
These fields study genetic influences on drug response and nutrient metabolism, enabling tailored injectable dosages and diet plans that maximize efficacy and minimize side effects, thus enhancing individualized treatment outcomes.
Are there ethical concerns related to using genomic data in weight loss personalization?
Yes. Protecting patient privacy, preventing genetic discrimination, and ensuring informed consent are essential ethical considerations when utilizing genomic information in clinical decision-making.
How do circadian rhythms affect injectable weight loss treatment efficacy?
Synchronizing injection and meal timing with the body’s internal clock optimizes hormone levels and metabolic responses, enhancing appetite suppression and glucose regulation.
What advanced monitoring tools assist in refining injectable weight loss and nutrition plans?
Biomarker monitoring such as continuous glucose monitoring and hormone assays enables dynamic adjustments of injections and macronutrient intake, preventing plateaus and improving safety and outcomes.
How can digital health tools improve adherence to injectable weight loss therapies?
AI-driven platforms offer injection reminders, dietary tracking, and symptom logging, fostering patient engagement and timely communication with healthcare providers for personalized support and intervention.
Trusted External Sources
- National Institutes of Health (NIH) – PubMed Central: Provides peer-reviewed research on GLP-1 receptor agonists, gut microbiota interactions, and pharmacogenomics, underpinning evidence-based therapeutic strategies.
- Journal of Clinical Endocrinology & Metabolism: Offers authoritative reviews on biochemical pathways of GLP-1 agonists, biomarker monitoring, and metabolic adaptations relevant to injectable weight loss treatments.
- American Diabetes Association (ADA): Publishes clinical guidelines on managing obesity and diabetes with pharmacotherapy and lifestyle integration, essential for safe and effective treatment planning.
- International Society of Nutrigenetics/Nutrigenomics (ISNN): Provides insights into genetic influences on nutrition and personalized medicine, informing precision diet and drug regimens.
- Chronobiology International: Features research on chrononutrition and circadian biology, critical for optimizing timing of injections and meals to align with endogenous rhythms.
Conclusion
Integrating injectable weight loss treatments with precision nutrition, adaptive exercise, and personalized timing strategies represents a transformative approach to obesity management. Understanding the complex interplay between pharmacology, diet, genetics, and circadian biology enables tailored interventions that maximize fat loss, preserve metabolic health, and enhance patient adherence. As digital tools and biomarker monitoring advance, individualized plans become increasingly feasible, reducing side effects and improving outcomes. Embracing these expert-informed strategies empowers patients and clinicians to co-create sustainable, effective weight loss journeys. Share your experiences, comment with questions, and explore related expert content to deepen your understanding and application of these cutting-edge approaches.


I found the discussion on aligning injection timing with meal patterns particularly insightful. From my experience, the practical challenge lies in establishing a consistent meal-injection routine that fits into a busy lifestyle. The idea of smaller, frequent meals to counteract nausea is something I’ve personally had to adapt to, and it truly makes a difference in tolerability. One aspect that resonated strongly is the emphasis on preserving lean muscle through increased protein intake during the injection’s peak activity. I hadn’t realized how critical this is for maintaining metabolic rate during weight loss phases, which often get overshadowed by the focus on just fat loss.
Also, the article’s mention of integrating gut microbiota modulation through probiotics and fiber-rich foods opened my eyes to the emerging role our gut health plays in boosting injectable treatment effectiveness. This holistic approach feels more sustainable rather than just relying solely on medication.
I’m curious, how do other readers balance the sometimes conflicting advice about meal frequency and macronutrient allocation while managing side effects? Has anyone experimented with timing or specific foods that significantly improved their comfort and weight loss outcomes? Sharing real-life strategies could be invaluable for those navigating this nuanced journey.
Elena, I really appreciate your insights on the challenges of finding the right meal-injection balance and the focus on lean muscle preservation with protein timing. In my experience, maintaining consistent mealtimes aligned with injection schedules was a game-changer. Early on, I struggled with nausea and fatigue, especially when meals were too large or heavy in fats during peak medication times. What helped me was shifting to smaller, nutrient-dense meals with an emphasis on lean proteins and complex carbs like quinoa or lentils, which also helped avoid those midday energy slumps.
Regarding macronutrient allocation, I found that increasing fiber intake through oats and fermented foods like yogurt strongly improved my digestion and overall gut comfort. This, coupled with probiotic supplementation, seemed to ease GI side effects and possibly enhanced medication efficacy as hinted in the article.
Overall, I think personalization is key—listening carefully to your body’s responses and tweaking both food types and timing accordingly. Has anyone else found particular foods or meal patterns that notably reduced side effects or improved energy during their injectable weight loss journey? It would be great to swap strategies that make this nuanced process feel more manageable and sustainable.
Elena and Marcus, your insights resonate with my recent experience combining injectables and a tailored diet. One challenge I’ve noticed is balancing the timing of injections with my natural hunger rhythms, which don’t always align neatly with strict meal schedules. I found that incorporating more plant-based proteins, like lentils and chickpeas, during the injection’s peak appetite suppression helped maintain energy without triggering nausea. Also, experimenting with fermented foods like sauerkraut and kefir has made a notable difference in managing digestive discomfort, likely due to improved gut microbiota as the article highlights.
On the matter of macronutrient allocation, I’ve struggled with the conflicting advice around fats—knowing they prolong satiety but can exacerbate nausea during peak medication times. What’s worked for me is consuming moderate healthy fats in the evening rather than near injection timing, which aligns with the circadian rhythm strategies discussed.
I’m curious, has anyone tried adjusting injection timing slightly to better suit their individual metabolic responses, perhaps experimenting with morning versus midday doses? How did that affect your appetite control and side effect profile? It seems that a personalized approach, including biomarker feedback as the post suggests, might be key here but I’d love to hear more firsthand experiences.