When Science Meets Appetite: Why Tirzepatide Is the Talk of the Town
Picture this: a medication that doesn’t just nudge your appetite but orchestrates a symphony of metabolic benefits, all while helping you shed stubborn pounds. Enter tirzepatide, the rising star in the GLP-1 medication realm that’s rewriting the script on weight management and diabetes care. If you’re wondering why everyone from endocrinologists to wellness enthusiasts is buzzing about this injectable wonder, you’re not alone.
Not Your Average Injection: Tirzepatide’s Dual Action Magic
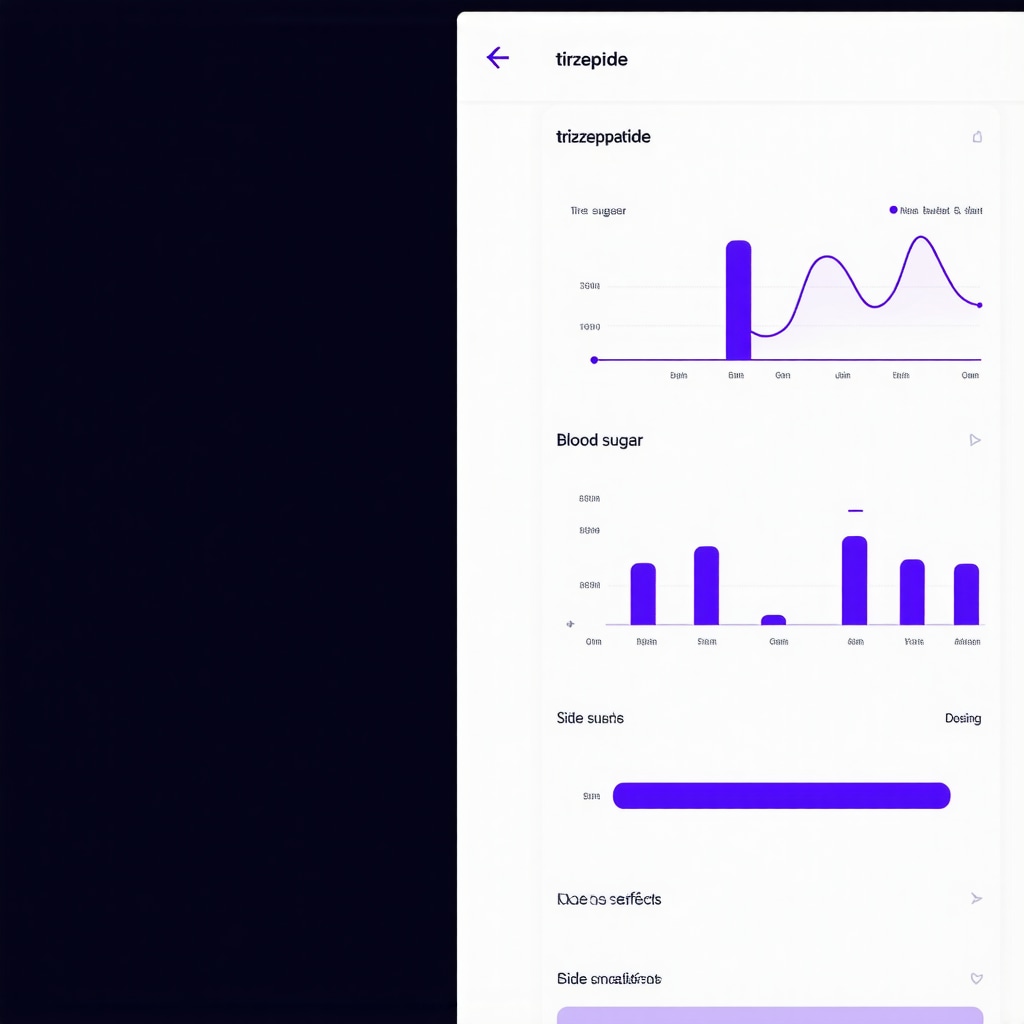
Unlike traditional GLP-1 receptor agonists that primarily stimulate insulin secretion and slow gastric emptying, tirzepatide doubles down by acting on both GLP-1 and GIP receptors. This dual-action approach is like having a tag team working tirelessly to improve blood sugar control and curb appetite, making it a game-changer for those battling obesity and type 2 diabetes.
Is Tirzepatide the Future of Appetite Control or Just Another Fad?
It’s a fair question. With so many weight-loss drugs promising the moon, can tirzepatide deliver? Clinical trials suggest yes. Participants not only experienced significant weight loss but also improvements in metabolic markers. But here’s the kicker – it’s not magic alone. Success hinges on integrating this medication with lifestyle tweaks. Curious? The detailed lifestyle guides at how to use tirzepatide effectively offer a treasure trove of expert advice.
Why Your Gut Will Thank You: The Science Behind the Benefits
Beyond weight loss, tirzepatide’s impact on the gut-brain axis is fascinating. By modulating hormones that signal fullness and energy balance, it subtly reprograms cravings and hunger cues. This isn’t just about eating less; it’s about eating smarter and feeling satisfied. For those keen on mastering appetite control, the insights shared in GLP-1 medication tips for appetite control can be a valuable companion.
When Does Expertise Make the Difference? Navigating Tirzepatide Safely
Injectables can be intimidating – but with proper medical guidance, they become powerful allies. Tirzepatide’s benefits are best realized under physician supervision, ensuring dosage customization and side effect management. For real-world wisdom and practical tips on balancing safety and efficacy, head over to effective tirzepatide use expert tips. Remember, your health journey deserves that blend of science and personalized care.
Still wondering about the latest research? A recent New England Journal of Medicine study provides compelling evidence of tirzepatide’s superiority in glycemic control and weight reduction compared to other therapies, cementing its position in modern treatment paradigms.
Feeling inspired or skeptical? Share your thoughts, experiences, or burning questions in the comments below. After all, understanding the nuances of GLP-1 medications like tirzepatide is a journey best traveled together.
Expanding Horizons: Tirzepatide’s Role Beyond Weight Loss
While tirzepatide’s headline-grabbing weight reduction effects are impressive, its influence extends into broader metabolic health realms. Emerging research highlights its potential in improving cardiovascular markers and insulin sensitivity, which are crucial for long-term health outcomes in patients with obesity and type 2 diabetes. The medication’s ability to modulate the gut-brain axis also suggests promising neuroendocrine benefits that warrant further exploration.
The Art of Personalization: Tailoring Tirzepatide Therapy for Maximum Benefit
No two bodies respond identically. This reality underscores the importance of personalized dosing strategies. Through careful monitoring and adjustment, physicians can optimize tirzepatide’s efficacy while minimizing side effects. For those interested in the nuances of dose customization, physician-guided fat loss injections provide an expert roadmap to tailoring injectable treatments effectively.
How Can Integrating Tirzepatide with Lifestyle Changes Enhance Long-Term Success?
The synergy between pharmacotherapy and lifestyle modifications cannot be overstated. Tirzepatide’s appetite-suppressing and metabolic effects create a physiological environment conducive to sustainable behavioral change. However, without conscious efforts in diet, exercise, and stress management, the full spectrum of benefits may not materialize. Practical strategies, such as mindful eating and strength training, can amplify results and improve quality of life. Resources like mindful eating tips for injectable users offer actionable guidance to integrate these elements seamlessly.
Addressing Safety and Side Effects: A Proactive Approach
Understanding and managing potential adverse effects is vital for maintaining adherence and optimizing outcomes. Common side effects, including nausea, injection site reactions, and occasional fatigue, are generally transient but require attentive management. Proactive communication with healthcare providers enables timely interventions, dose adjustments, and supportive measures. Comprehensive advice on managing injection side effects is essential for empowering patients through this journey.
Furthermore, the New England Journal of Medicine offers authoritative insights into tirzepatide’s safety profile and comparative efficacy, reinforcing its position within evidence-based clinical practice.
For those navigating the complexities of injectable therapies, exploring supervised injectable weight loss can provide a structured and safe framework that balances efficacy with patient safety.
What has been your experience integrating tirzepatide with lifestyle changes or managing its side effects? Share your insights or questions in the comments below – your perspective enriches the community’s understanding and supports collective success.
Precision Medicine in Action: Customizing Tirzepatide Protocols for Complex Metabolic Profiles
While tirzepatide’s dual agonist mechanism offers broad-spectrum metabolic benefits, the heterogeneity of patient responses demands a nuanced approach to therapy customization. Factors such as baseline insulin resistance, beta-cell function, and even genetic polymorphisms influencing incretin receptor sensitivity can modulate efficacy and tolerability. Emerging research advocates for integrating biomarkers like HOMA-IR and continuous glucose monitoring data to fine-tune dosing increments, enhancing both safety and therapeutic outcomes. This precision medicine paradigm not only optimizes weight loss trajectories but also mitigates risks of hypoglycemia and gastrointestinal side effects.
What Are the Cutting-Edge Biomarkers Guiding Tirzepatide Dose Adjustments in Refractory Obesity?
Advanced clinical strategies now incorporate inflammatory markers (e.g., high-sensitivity C-reactive protein), adipokine profiles, and incretin hormone assays to better phenotype patients. For instance, elevated baseline GIP levels might predict enhanced responsiveness to tirzepatide’s dual receptor action, whereas individuals with diminished GLP-1 receptor expression could require alternative or adjunctive therapies. A landmark study from Diabetes Care highlights how integrating these biomarkers into clinical algorithms can personalize treatment and optimize efficacy in complex cases.
Synergizing Pharmacotherapy with Metabolic Flexibility: Beyond Caloric Restriction
Traditional approaches to weight loss often emphasize caloric restriction, yet tirzepatide’s modulation of energy homeostasis invites a more sophisticated strategy centered on enhancing metabolic flexibility—the body’s capacity to switch between lipid and carbohydrate utilization efficiently. Incorporating intermittent fasting protocols or time-restricted feeding can potentiate tirzepatide’s effects on mitochondrial function and insulin sensitivity. Moreover, tailored exercise regimens focusing on high-intensity interval training (HIIT) have shown promise in augmenting incretin sensitivity and amplifying fat oxidation, creating a virtuous cycle of metabolic improvement.
Delving deeper, the neuroendocrine adaptations driven by tirzepatide may recalibrate hypothalamic pathways governing appetite and energy expenditure. This complex feedback loop underscores the importance of integrating behavioral therapy and nutritional counseling to sustain long-term metabolic health.
Innovative Solutions to Overcome Common Therapeutic Challenges with Tirzepatide
Despite its impressive profile, tirzepatide treatment is not without hurdles. Gastrointestinal side effects remain the primary cause of discontinuation. Cutting-edge approaches include gradual dose escalation protocols, adjunctive use of prokinetic agents, and personalized timing of injections to mitigate nausea and improve adherence.
Furthermore, emerging digital health tools equipped with AI-driven symptom tracking enable real-time monitoring of side effects and metabolic responses, facilitating timely interventions. Such integration of technology with clinical care exemplifies the future of personalized medicine in metabolic disorders.
For practitioners and patients alike, staying abreast of these innovations is critical. Resources that delve into these advanced management strategies, such as those offered by expert endocrinology networks, can be invaluable in navigating these complexities.
Are you interested in exploring how personalized tirzepatide regimens can transform metabolic health in challenging cases? Engage with our expert community or schedule a consultation to tailor your approach.
Beyond Basics: How Precision Medicine is Revolutionizing Tirzepatide Therapy
As tirzepatide continues to disrupt traditional weight management and diabetes treatment, a growing body of evidence highlights the importance of precision medicine in maximizing its benefits. Tailoring dosing protocols based on individual metabolic profiles—taking into account factors like insulin resistance, beta-cell functionality, and even genetic markers—ushers in a new era of personalized care. This bespoke approach not only enhances efficacy but also mitigates common side effects, allowing patients to optimize their therapeutic journey.
For a deep dive into physician-guided customization of injectable treatments, explore physician-guided fat loss injections, which provide an expert roadmap to individualizing dosage for maximum benefit.
What Cutting-Edge Biomarkers Are Shaping Tirzepatide Dose Adjustments in Complex Cases?
Recent advancements in metabolic research spotlight biomarkers such as high-sensitivity C-reactive protein (hs-CRP), adipokine profiles, and incretin hormone levels as pivotal in predicting patient responsiveness to tirzepatide. A notable study published in Diabetes Care discusses how integrating these markers into clinical algorithms can refine dosing strategies, particularly for patients with refractory obesity or atypical metabolic phenotypes. Utilizing continuous glucose monitoring (CGM) data alongside these biomarkers enables clinicians to anticipate hypoglycemia risk and adjust titration schedules proactively.
Metabolic Flexibility Meets Pharmacotherapy: Rethinking Weight Loss Beyond Calorie Counting
Caloric restriction has long dominated weight loss paradigms, but tirzepatide’s unique modulation of energy homeostasis invites a more nuanced strategy emphasizing metabolic flexibility—the body’s ability to switch efficiently between fuel sources. Integrating lifestyle interventions such as intermittent fasting or time-restricted feeding with tirzepatide can potentiate mitochondrial efficiency and insulin sensitivity. Complementary exercise regimens, especially high-intensity interval training (HIIT), further enhance incretin sensitivity and promote fat oxidation, creating a synergistic metabolic environment conducive to sustainable fat loss.
For those interested in combining pharmacotherapy with evidence-based lifestyle adjustments, the insights at effective use of tirzepatide adjusting lifestyle for better results offer practical guidance.
Leveraging AI and Digital Health: The New Frontier in Tirzepatide Side Effect Management
Gastrointestinal discomfort remains the leading cause of tirzepatide discontinuation, presenting a clinical challenge. Innovative dose escalation protocols and adjunctive therapies are traditional countermeasures, but the integration of AI-powered digital health tools is revolutionizing this space. Real-time symptom tracking apps powered by artificial intelligence can monitor side effect patterns, predict exacerbations, and suggest timely interventions, thereby improving adherence and patient quality of life.
Patients and providers can explore strategies to mitigate side effects proactively at avoiding side effects in prescription injection weight loss, a resource dedicated to empowering users through education and technology.
How Can AI-Driven Symptom Monitoring Transform Tirzepatide Treatment Outcomes?
By harnessing machine learning algorithms, AI platforms analyze individual patient data to customize side effect management plans, optimize dosing schedules, and enhance patient engagement. This technology fosters a dynamic feedback loop between patients and healthcare teams, enabling swift adjustments and personalized support. A recent review in Nature Digital Medicine underscores the transformative potential of AI in chronic disease management, including injectable therapies like tirzepatide.
Engage with our expert community and share your experiences or questions about managing tirzepatide’s challenges. Your insights help build a richer dialogue and foster collective success. For personalized advice, consider scheduling a consultation through our contact page—because your health journey deserves tailored support every step of the way.
Expert Insights & Advanced Considerations
Dual Agonism Unlocks a New Therapeutic Frontier
Tirzepatide’s simultaneous activation of GLP-1 and GIP receptors represents a paradigm shift in metabolic therapy. This dual mechanism not only enhances glycemic control but also synergistically modulates appetite and energy homeostasis, offering superior outcomes in weight management compared to traditional GLP-1 receptor agonists alone. Clinicians should consider this when tailoring treatment plans for patients with complex metabolic profiles.
Biomarker-Guided Personalization Enhances Safety and Efficacy
Emerging evidence supports the integration of biomarkers such as hs-CRP, adipokine levels, and incretin hormone assays to predict individual responsiveness and tailor tirzepatide dosing. Combining these with continuous glucose monitoring provides a precision medicine framework that minimizes side effects like hypoglycemia and gastrointestinal discomfort while maximizing therapeutic benefit.
Metabolic Flexibility Is the Key to Sustainable Fat Loss
Beyond pharmacotherapy, optimizing metabolic flexibility through intermittent fasting, time-restricted feeding, and targeted exercise protocols such as HIIT can potentiate tirzepatide’s effects. This approach enhances mitochondrial efficiency and insulin sensitivity, creating a metabolic environment conducive to long-term weight loss maintenance and improved cardiometabolic health.
AI-Driven Digital Tools Revolutionize Side Effect Management
The integration of AI-powered symptom tracking platforms enables real-time monitoring of gastrointestinal and other side effects, facilitating proactive dose adjustments and supportive interventions. This technology enhances patient adherence and quality of life, marking a new era in the management of injectable therapies like tirzepatide.
Comprehensive Lifestyle Integration Amplifies Medication Impact
Weight loss medications are most effective when combined with evidence-based lifestyle changes. Mindful eating, stress management, and strength training complement tirzepatide’s pharmacodynamics, leading to more sustainable appetite control and metabolic improvements. Resources like effective use of tirzepatide adjusting lifestyle for better results provide practical guidance for integrating these elements.
Curated Expert Resources
- New England Journal of Medicine (NEJM): Offers rigorous clinical trial data and authoritative reviews on tirzepatide’s efficacy and safety profiles, essential for evidence-based practice.
- Diabetes Care Journal: Features cutting-edge research on precision medicine approaches, including biomarker-driven dosing strategies relevant to tirzepatide therapy.
- eWeightLossTips.com: A comprehensive platform providing expert advice on injectable weight loss therapies, lifestyle modifications, and managing side effects, including expert tips for appetite management and strategies to avoid side effects.
- Nature Digital Medicine: Explores the transformative potential of AI in chronic disease management, including real-world applications for monitoring tirzepatide side effects.
- Physician-Guided Fat Loss Injections (customizing dosage): Offers practical frameworks for individualized injectable treatment plans that optimize outcomes and reduce adverse effects.
Final Expert Perspective
Tirzepatide stands at the forefront of a new era in metabolic care, where dual receptor agonism, personalized medicine, and lifestyle synergy converge to redefine weight management and diabetes treatment. Understanding its nuanced mechanisms, embracing biomarker-guided customization, and leveraging digital health innovations empower healthcare providers and patients alike to unlock its full potential safely and effectively. For those ready to elevate their approach, engaging with advanced resources and clinical expertise is indispensable. Your journey with tirzepatide is not just about medication—it’s about crafting a comprehensive, individualized strategy for lasting metabolic health.
We invite you to deepen this conversation by sharing your clinical experiences or questions, exploring expert-led content like mastering prescription injection weight loss with medical guidance, or connecting through our contact page to tailor your metabolic health plan with professional support.


The way tirzepatide combines action on both GLP-1 and GIP receptors truly stands out compared to earlier diabetes and weight management drugs. This dual approach seems to not only improve blood sugar control but also subtly recalibrates hunger signals, which I find fascinating since it aligns with the emerging understanding that metabolic health is deeply connected to gut-brain communication. I’ve noticed in some discussions that patients experience a better sense of fullness and reduced cravings, which, as the article points out, is more about eating smarter rather than just eating less. However, the emphasis on integrating this medication with lifestyle changes can’t be overstated. In my experience supporting family members on similar therapies, those who combine the drug with mindful eating and physical activity tend to see more sustainable results. I’m curious to hear from others: has anyone found particular lifestyle strategies that synergize best with tirzepatide’s effects? For example, do certain dietary patterns or types of exercise seem to amplify the medication’s benefits? Let’s share what’s worked because these nuances can really shape long-term success beyond just the pharmacology.
This post really highlights the multifaceted nature of tirzepatide and its potential beyond just weight loss. I’ve read that its effects on the gut-brain axis could be transformative, especially for people who struggle with persistent cravings and metabolic inflexibility. From my own experience supporting friends with similar treatments, integrating moderate exercise like walking or yoga seems to enhance its benefits, possibly because it helps improve insulin sensitivity further. What I find particularly interesting is how personalized medicine might play a critical role in optimizing outcomes with tirzepatide. Has anyone here experimented with specific lifestyle modifications tailored to their metabolic profile? For example, using continuous glucose monitoring data to adjust diet or activity levels? I think combining these strategies could unlock even greater benefits and make the treatment more sustainable in the long run. Would love to hear others’ insights or practical tips on what has worked to boost tirzepatide’s effects in daily life.