Understanding the Mechanistic Sophistication of GLP-1 Injectable Medications
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a transformative advancement in metabolic medicine, primarily utilized for managing type 2 diabetes and increasingly for obesity treatment. These injectable medications leverage the body’s endogenous pathways to modulate glycemic control and appetite regulation. Their mechanism involves mimicking the incretin hormone GLP-1, which enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, delays gastric emptying, and promotes satiety. This multi-faceted pharmacodynamic profile underpins their efficacy in weight reduction and improved metabolic outcomes.
Clinical Nuances and Pharmacokinetic Profiles Impacting Injectable GLP-1 Use
Injectable GLP-1 therapies, such as semaglutide and liraglutide, differ in their molecular structure, half-life, and administration frequency, which critically influence patient adherence and therapeutic success. Extended-release formulations enable once-weekly dosing, improving convenience and consistency of plasma drug levels. However, these benefits come with considerations of injection site reactions and gastrointestinal tolerability that require expert management. Tailoring dose titration protocols based on individual metabolic responses and tolerability is essential to maximize benefit while minimizing adverse effects.
How Do Injectable GLP-1 Medications Integrate with Lifestyle Modifications for Optimal Outcomes?
One of the pivotal expert inquiries revolves around the synergy between GLP-1 injectables and lifestyle interventions. While pharmacotherapy provides a potent physiological foundation for weight loss and glycemic control, its integration with diet, exercise, and behavioral strategies is indispensable. Studies indicate that combining GLP-1 receptor agonists with structured nutritional plans and physical activity amplifies fat loss and metabolic improvement beyond medication alone. Clinicians emphasize personalized, physician-guided programs to harmonize these elements effectively, as detailed in resources like GLP-1 Medication Insights: Combining Injections with Lifestyle for Maximum Benefit.
Addressing Safety and Side Effect Management: An Expert Perspective
Injectable GLP-1 medications, while generally safe, necessitate vigilant monitoring for potential side effects including nausea, injection site reactions, and rare but serious risks like pancreatitis. Expert protocols advocate gradual dose escalation and patient education to mitigate initial gastrointestinal symptoms. Moreover, ongoing clinical evaluation, including laboratory testing, ensures early detection of complications and supports sustained treatment adherence. Trusted sources such as the NIH’s comprehensive review on GLP-1 receptor agonists provide evidence-based guidance reinforcing these best practices.
Contextual CTA: Deepen Your Understanding and Share Your Expertise
For healthcare professionals and patients aiming to optimize injectable GLP-1 therapy, exploring advanced insights into safe administration, dose management, and lifestyle integration is paramount. We encourage you to visit our contact page to engage with experts or contribute your clinical experiences. Enhance your expertise and help shape the evolving landscape of GLP-1 injectable therapies.
Optimizing Injection Timing and Dosage for Personalized Weight Loss Success
While the pharmacokinetics of GLP-1 receptor agonists like semaglutide offer convenient dosing schedules, individualized timing and dosage adjustments can further enhance therapeutic outcomes. Expert clinicians recommend tailoring injection timing relative to meals and circadian rhythms to capitalize on appetite suppression and metabolic effects. For instance, administering injections in the morning may align better with natural hunger patterns and promote sustained satiety throughout the day. Additionally, gradual dose escalation based on patient tolerance and metabolic response can minimize side effects while maximizing fat loss benefits. Resources such as Weekly Injection Weight Loss Guide: Managing Cravings Effectively provide practical frameworks for implementing these strategies.
Integrating Psychological and Behavioral Interventions to Complement Injectable Therapy
Effective weight management extends beyond pharmacological intervention. Psychological resilience and behavioral modification play critical roles in sustaining long-term success with GLP-1 medications. Techniques such as mindful eating, cognitive behavioral therapy, and stress management can enhance patient adherence and mitigate emotional eating triggers often unaddressed by medication alone. Multidisciplinary approaches involving dietitians, psychologists, and medical providers create a supportive environment conducive to holistic metabolic health. For clinicians, developing comprehensive plans that incorporate these elements alongside injection therapy is increasingly recognized as best practice.
What Are the Emerging Challenges in Long-Term Use of GLP-1 Injectables for Obesity Management?
Despite promising outcomes, long-term use of GLP-1 receptor agonists presents evolving challenges that merit expert attention. Tolerance development, fluctuating efficacy, and patient burnout are notable concerns. Furthermore, understanding the implications of discontinuation or dose adjustment on weight regain and metabolic parameters remains an active area of research. Addressing these issues requires vigilant monitoring, patient education, and adaptive treatment plans. According to a recent review published by Frontiers in Endocrinology, sustained weight loss maintenance strategies must integrate pharmacotherapy with lifestyle and psychosocial support to mitigate relapse risks.
Leveraging Technology for Enhanced Adherence and Outcome Tracking
Digital health tools are revolutionizing management paradigms for patients on injectable GLP-1 therapies. Mobile applications and wearable devices enable real-time monitoring of medication adherence, physical activity, and dietary intake, providing valuable data to both patients and providers. These technologies facilitate timely interventions, personalized feedback, and motivation reinforcement. Integrating such tools within supervised weight loss programs enhances accountability and optimizes clinical outcomes, complementing traditional care models.
Call to Action: Engage with the Latest Expert Resources and Share Your Experience
Healthcare professionals and patients alike are encouraged to deepen their understanding of injectable GLP-1 therapies by exploring advanced clinical strategies and patient-centered approaches. Share your insights or seek tailored guidance by visiting our contact page. Collaborate with experts to refine your practice or treatment journey, and contribute to the evolving knowledge base on effective, safe injectable weight loss interventions.
Precision Medicine in GLP-1 Injectable Therapy: Tailoring Treatments through Genetic and Metabolic Profiling
As the field of metabolic therapeutics evolves, precision medicine emerges as a pivotal paradigm in optimizing GLP-1 receptor agonist therapy. Genetic polymorphisms affecting incretin receptor expression or downstream signaling pathways can significantly influence individual response to these agents. Metabolic profiling—including assessments of insulin sensitivity, beta-cell function, and gut hormone milieu—further refines personalization strategies. Incorporating pharmacogenomics and metabolomics enables clinicians to predict efficacy and adverse event risk, thus tailoring dosing regimens and adjunct interventions with unprecedented specificity.
For example, recent studies highlight how variations in the GLP1R gene correlate with differential weight loss outcomes and gastrointestinal tolerability, underscoring the need for genotype-informed clinical decision-making (source: PMC7368812).
Addressing the Complex Interplay Between Gut Microbiota and GLP-1 Receptor Agonist Efficacy
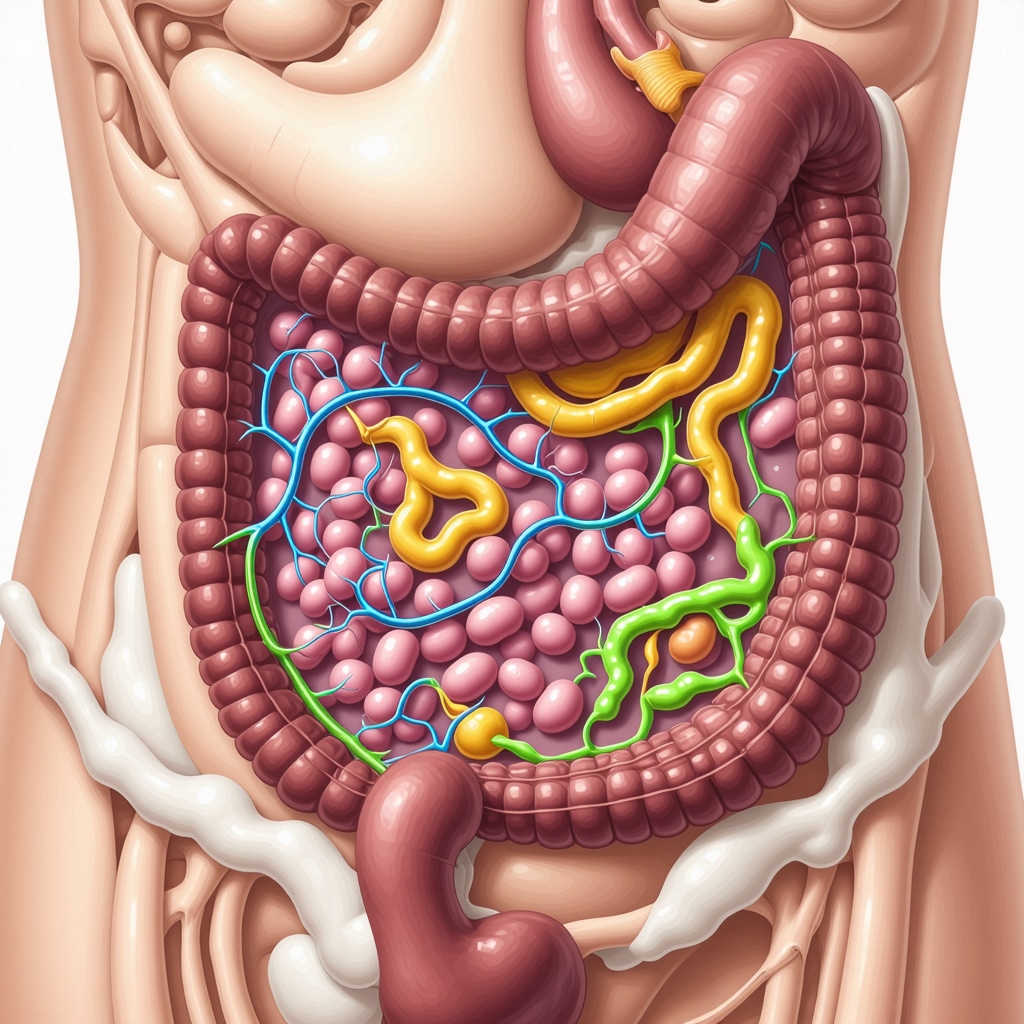
Emerging research elucidates the intricate relationship between the gut microbiome and GLP-1 receptor agonist effectiveness. The microbiota modulates host metabolism, appetite regulation, and inflammatory status, all of which impact therapeutic outcomes. Modifications in microbial composition induced by GLP-1 therapy may contribute to enhanced satiety signals and improved glycemic control. Conversely, baseline dysbiosis could attenuate drug efficacy or exacerbate side effects.
Advanced practitioners are exploring probiotic and prebiotic adjuncts to optimize microbiome profiles, potentially potentiating GLP-1-mediated benefits. This frontier intersects with personalized nutrition, where microbial signatures guide dietary recommendations complementary to injectable therapy.
How Can Emerging Biomarkers Inform Real-Time Monitoring and Adjustment of GLP-1 Injectable Regimens?
Real-time biomarker tracking is a burgeoning area critical to refining GLP-1 therapy. Biomarkers such as plasma GLP-1 concentrations, insulin and glucagon ratios, and appetite-regulating neuropeptides provide dynamic feedback on treatment efficacy and tolerability. Integrating continuous glucose monitoring (CGM) with biomarker assays offers a multidimensional view of metabolic responses, enabling rapid dose adjustments.
Advanced diagnostic platforms leveraging machine learning algorithms can predict adverse events or therapeutic plateaus, facilitating proactive clinical decisions. These innovations promise to transform the standard reactive approach into a preemptive, precision-guided management model.
Overcoming Immunogenicity and Injection Site Reactions: Novel Formulation and Delivery Innovations
Injection site reactions and immunogenic responses remain challenges limiting optimal GLP-1 injectable use. Current research is focused on developing next-generation formulations employing nanotechnology and biodegradable microspheres to reduce local irritation and enhance sustained drug release. Alternative delivery routes, such as transdermal systems and oral semaglutide with specialized absorption enhancers, are under active investigation to improve patient adherence and broaden therapeutic applicability.
These advancements not only aim to mitigate adverse effects but also to expand the patient population benefiting from GLP-1 receptor agonists by addressing barriers related to injection anxiety and tolerability.
Integrating Artificial Intelligence and Telemedicine for Enhanced Patient Engagement and Outcome Optimization
Artificial intelligence (AI) and telemedicine platforms are revolutionizing the management of patients on GLP-1 injectable therapies. AI-driven apps analyze patient-reported outcomes, glycemic data, and lifestyle inputs to deliver personalized coaching, adherence reminders, and early warning signals for side effects. Telehealth consultations provide real-time clinician support, fostering timely interventions and sustained motivation.
These technologies facilitate a collaborative care model, bridging gaps between clinic visits and empowering patients as active participants in their metabolic health journey. As digital ecosystems mature, they will undoubtedly become integral to comprehensive GLP-1 therapy programs.
Call to Action: Explore Cutting-Edge Research and Collaborate with Metabolic Experts
To stay at the forefront of injectable GLP-1 therapy innovation, clinicians and researchers are encouraged to engage with specialized forums and subscribe to journals such as Pharmacogenomics and Metabolic Therapeutics. Sharing case studies and clinical experiences helps refine personalized approaches and overcome emerging challenges. Visit our contact page to connect with experts and participate in collaborative initiatives shaping the future of metabolic medicine.
Pioneering Precision: Pharmacogenomics and Metabolomics in Tailored GLP-1 Therapy
Building upon the foundational understanding of GLP-1 receptor agonists, contemporary research underscores the critical role of pharmacogenomic profiling in refining therapeutic outcomes. Variants within the GLP1R gene and related metabolic pathways dictate interindividual variability in drug efficacy and adverse event susceptibility. Integrating comprehensive metabolomic analyses—including insulin sensitivity indices and gut hormone signatures—enables clinicians to sculpt dosing regimens and adjunctive lifestyle interventions with unparalleled specificity, effectively ushering in an era of personalized metabolic medicine.
Gut Microbiota: The Unsung Modulator of GLP-1 Therapeutic Potency
Emerging evidence reveals a nuanced interplay between the gut microbiome and GLP-1 receptor agonist responses. Microbial communities influence host energy homeostasis, inflammatory milieu, and neuroendocrine signaling, thereby modulating drug efficacy. Tailored probiotic and prebiotic strategies are being explored to recalibrate dysbiotic profiles, potentiating satiety and glycemic improvements. This integrative approach converges precision nutrition with injectable therapy, promising enhanced and sustained metabolic benefits.
How Can Emerging Biomarkers Inform Real-Time Monitoring and Adjustment of GLP-1 Injectable Regimens?
The advent of dynamic biomarker tracking—encompassing plasma GLP-1, insulin-to-glucagon ratios, and appetite-regulating neuropeptides—ushers in transformative possibilities for personalized dose titration. When coupled with continuous glucose monitoring (CGM), these biomarkers provide multidimensional insight into metabolic responses, enabling clinicians to preemptively mitigate side effects and optimize efficacy. Cutting-edge platforms employing machine learning algorithms are poised to revolutionize the therapeutic paradigm, transitioning from reactive to anticipatory management.
Mitigating Immunogenicity and Injection Site Reactions Through Next-Generation Formulations
Addressing the persistent challenge of injection site reactions and immunogenic responses, research is converging on advanced delivery systems utilizing nanotechnology and biodegradable microspheres. These innovations aim to minimize local tissue irritation while facilitating sustained drug release kinetics. Concurrently, alternative administration routes, including transdermal patches and oral formulations enhanced for bioavailability, are under rigorous clinical evaluation, promising to alleviate injection-related barriers and broaden patient accessibility.
Harnessing Artificial Intelligence and Telemedicine: Revolutionizing Patient-Centric GLP-1 Therapy
The integration of AI-powered digital health tools with telemedicine platforms is catalyzing a paradigm shift in GLP-1 injectable management. By synthesizing patient-reported outcomes, glycemic metrics, and lifestyle data, AI algorithms deliver personalized coaching, adherence reminders, and early adverse event detection. Real-time telehealth consultations further amplify clinical responsiveness and patient engagement, fostering a collaborative, data-driven care model that transcends traditional episodic visits.
Authoritative Source Spotlight: Pharmacogenomics and Metabolic Therapeutics
For a comprehensive exploration of the genetic and metabolic determinants influencing GLP-1 therapy outcomes, the peer-reviewed article available at the National Center for Biotechnology Information (NCBI) offers an invaluable resource. This publication delineates the molecular underpinnings and clinical implications of precision medicine approaches in metabolic therapeutics.
Engage and Elevate Your Expertise in GLP-1 Injectable Innovations
We invite clinicians, researchers, and informed patients to deepen their mastery of cutting-edge GLP-1 injectable strategies by connecting with our expert network. Visit our contact page to share experiences, access specialized guidance, and contribute to advancing the frontier of metabolic medicine.
Expert Insights & Advanced Considerations
Precision Medicine as a Cornerstone for Optimized GLP-1 Injectable Therapy
Incorporating pharmacogenomic and metabolomic profiling into clinical practice enables unprecedented personalization of GLP-1 receptor agonist regimens. Tailoring doses and adjunctive interventions based on genetic variants like GLP1R polymorphisms and metabolic signatures enhances efficacy and tolerability, marking a shift toward truly individualized metabolic medicine.
Gut Microbiota Modulation as a Key Lever to Amplify Therapeutic Outcomes
Emerging evidence reveals that the gut microbiome profoundly influences response to GLP-1 injectables. Strategic use of probiotics, prebiotics, and dietary modifications to optimize microbial composition can potentiate appetite regulation and glycemic control, positioning microbiome management as an integral facet of comprehensive treatment plans.
Dynamic Biomarker Integration for Responsive and Predictive Treatment Adjustment
Real-time monitoring of biomarkers such as plasma GLP-1 levels, insulin-to-glucagon ratios, and neuropeptides, especially when combined with continuous glucose monitoring, offers a sophisticated feedback loop. Leveraging machine learning to interpret these data enables anticipatory dose modifications and side effect mitigation, advancing beyond reactive management.
Innovations in Drug Delivery to Overcome Immunogenicity and Enhance Patient Experience
Next-generation formulations employing nanotechnology and biodegradable microspheres promise to reduce injection site reactions and improve sustained drug release. Alternative routes like transdermal patches and oral semaglutide are progressing through clinical trials, aiming to elevate adherence and broaden access by minimizing injection-related barriers.
Artificial Intelligence and Telemedicine: Transforming Patient Engagement in GLP-1 Therapy
AI-powered digital health platforms integrated with telemedicine offer personalized coaching, adherence support, and early detection of adverse events, fostering a collaborative care model. This technology-driven approach enhances patient empowerment and continuous clinician interaction, essential for sustained treatment success.
Curated Expert Resources
- Pharmacogenomics and Metabolic Therapeutics (NCBI PMC7368812): A comprehensive peer-reviewed resource detailing genetic and metabolic determinants influencing GLP-1 therapy outcomes, invaluable for clinicians aiming to implement precision approaches.
- Frontiers in Endocrinology Review (PMC7859924): Discusses long-term challenges and strategies in GLP-1 receptor agonist therapy, providing evidence-based frameworks for sustained weight loss maintenance.
- GLP-1 Medication Insights: Combining Injections with Lifestyle for Maximum Benefit: An authoritative guide emphasizing the synergy of pharmacotherapy and behavioral interventions to optimize metabolic outcomes (Read More).
- Weekly Injection Weight Loss Guide: Managing Cravings Effectively: Practical strategies for injection timing and appetite control to enhance patient adherence and fat loss (Explore Here).
- Medically Supervised Weight Loss: Tracking Progress with Lab Tests: Highlights the importance of laboratory monitoring to ensure safety and optimize injectable therapy results (Learn More).
Final Expert Perspective
The landscape of injectable GLP-1 therapy for weight loss is rapidly evolving, driven by advances in precision medicine, microbiome science, biomarker technology, and innovative drug delivery. These sophisticated tools and approaches empower clinicians to tailor interventions with remarkable specificity, enhancing efficacy while reducing adverse effects. Integrating artificial intelligence and telemedicine further refines patient engagement, creating a dynamic, responsive care continuum. For healthcare professionals and patients committed to maximizing the potential of injectable GLP-1 medications, continuous education and collaboration are paramount. We encourage you to deepen your expertise and share your clinical experiences by visiting our contact page, where you can engage with specialists and access advanced resources guiding the future of metabolic therapy.


I found the detailed explanation of GLP-1’s mechanisms particularly insightful, especially how it influences multiple pathways like delaying gastric emptying and promoting satiety. From my experience working with patients who are on these injectables, I’ve noticed that individual responses can vary significantly, which underscores the importance of personalized approaches, including genetic and microbiome considerations. The emerging research on pharmacogenomics and gut microbiota is promising, potentially guiding us toward more tailored treatments. I’m curious, in clinical practice, how have others been adjusting dosing or combining these therapies with microbiome-modulating interventions for better outcomes? It seems integrating these precision medicine strategies could really enhance efficacy and reduce side effects.
The post offers a comprehensive look at the complex mechanisms behind GLP-1 receptor agonists. From my clinical perspective, understanding their multi-pathway effects—like delaying gastric emptying and promoting satiety—helps tailor treatments more effectively. One challenge I encounter is balancing the therapeutic benefits with potential side effects, especially gastrointestinal issues. I’ve found that gradual dose escalation combined with patient education makes a significant difference. Regarding personalized approaches, I wonder how clinicians are integrating genetic testing or microbiome profiling into routine practice. Has anyone seen measurable improvements by adjusting doses based on pharmacogenomic data? The emerging research on microbiome modulation is fascinating too, as it could open doors to synergistic therapies. Integrating nutritional strategies with injectable treatments seems promising, but what practical steps are you taking to incorporate these insights into daily patient care? It would be great to hear more on successful protocols.