Unlocking the Dual-Action Power of Tirzepatide in Fat Loss
In the evolving landscape of weight management, GLP-1 medications have carved out a transformative role, with tirzepatide emerging as a particularly potent agent. Unlike traditional weight loss strategies, tirzepatide operates through a unique dual mechanism targeting both glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors. This innovative approach not only enhances fat loss but also optimizes metabolic health, making it a game-changer in the fight against obesity.
Beyond Appetite Suppression: How Tirzepatide Enhances Metabolic Fat Burning
While many GLP-1 receptor agonists primarily curb appetite, tirzepatide’s synergy with GIP receptors amplifies fat oxidation and energy expenditure. This dual receptor activation facilitates improved insulin sensitivity, reducing fat storage and promoting the breakdown of existing adipose tissue. Clinical trials have shown that patients on tirzepatide experience significant reductions in body fat percentage, surpassing the results seen with semaglutide alone. These effects underscore tirzepatide’s capacity to recalibrate metabolic pathways towards sustained fat loss.
What Makes Tirzepatide More Effective Than Other GLP-1 Medications?
The distinctive efficacy of tirzepatide lies in its molecular design that mimics both GIP and GLP-1 incretins. This dual incretin mimetic effect leads to enhanced insulin secretion, better glycemic control, and a pronounced decrease in appetite and caloric intake. Moreover, tirzepatide’s influence on GIP receptors is believed to reduce fat accumulation in adipocytes, a mechanism not fully leveraged by other GLP-1 agonists. This multifaceted action results in more comprehensive weight loss outcomes, particularly in visceral fat reduction, which is critical for improving cardiovascular and metabolic health.
Integrating Tirzepatide into a Holistic Fat Loss Regimen
Maximizing tirzepatide’s benefits involves pairing the medication with lifestyle modifications such as tailored nutrition and physical activity. Studies emphasize that while tirzepatide provides a physiological advantage, sustained fat loss and metabolic improvements are optimized when combined with physician-guided dietary plans and exercise routines. For individuals seeking expert advice on combining tirzepatide with lifestyle strategies, resources like effective use of tirzepatide for fat loss offer practical guidance.
Expert Insights: Navigating Side Effects and Ensuring Safe Use
As with any pharmacological intervention, tirzepatide requires careful management to minimize side effects such as nausea or gastrointestinal discomfort. Health professionals recommend gradual dose escalation and close monitoring to enhance tolerability. Detailed strategies and expert tips on managing side effects effectively can be found in specialized guides like how to adjust your tirzepatide dose to minimize side effects. This ensures a safer and more sustainable weight loss journey.
Scientific Foundations: What Research Reveals About Tirzepatide’s Impact
Groundbreaking studies published in journals such as The New England Journal of Medicine highlight tirzepatide’s superior outcomes in glycemic control and weight reduction compared to other GLP-1 receptor agonists. These findings are pivotal for clinicians and patients alike, providing evidence-based confidence in tirzepatide’s role as a cornerstone in modern metabolic therapy.
Are you curious about how to incorporate tirzepatide into your weight loss journey effectively? Explore expert tips and strategies here to maximize your results while maintaining safety and long-term health.
Adapting to Tirzepatide: My Journey Through Side Effects and Solutions
Starting tirzepatide was a turning point in my weight loss journey, but it wasn’t without its challenges. The initial weeks brought some nausea and mild digestive discomfort, which honestly caught me off guard. I learned quickly that these side effects are common, especially when starting or increasing the dose. Gradual dose adjustments, as recommended by my healthcare provider, really helped me adapt. I also found that timing injections in the evening reduced the impact of nausea during my active hours.
Another tip that worked for me was staying well-hydrated and having small, frequent meals rich in fiber. This combo seemed to ease my stomach and kept energy levels stable. For anyone navigating similar issues, I highly recommend checking out detailed advice on how to adjust your tirzepatide dose to minimize side effects. It’s packed with practical strategies that can make a big difference in tolerability and overall comfort.
Why Consistency and Tracking Are Game Changers
One of the biggest lessons I learned was the importance of consistency—not just in taking the medication but also in tracking progress. Recording my weight, appetite changes, and energy levels weekly helped me and my doctor fine-tune the treatment plan. It also kept me motivated seeing tangible progress, even when the scale didn’t move dramatically at times.
Tools like journals or apps designed for weekly injection weight loss progress tracking can be invaluable. They offer an easy way to spot trends, identify triggers for side effects, and celebrate small victories that keep you moving forward.
How Can You Maintain Motivation When Fat Loss Feels Slow?
That question resonates deeply with me, as there were moments when the pace seemed frustratingly slow. I found that focusing on non-scale victories—like improved stamina, better sleep, or clothes fitting differently—helped shift my mindset. Surrounding myself with supportive communities and sharing experiences also made a huge difference. If you’re struggling, remember it’s a marathon, not a sprint. Patience combined with medical guidance and lifestyle tweaks creates the best environment for long-term success.
Learning from Science and Real-Life Stories
What truly convinced me to commit to tirzepatide was the robust science behind it. For example, a comprehensive review published by the National Center for Biotechnology Information (NCBI) details how tirzepatide’s dual-action mechanism leads to significant fat loss and metabolic improvements. Knowing that experts back these findings gave me confidence to persevere despite the initial hurdles.
Integrating this medication with a balanced diet and regular activity, as I’ve discussed earlier, creates a synergy that’s hard to beat. If you want to dive deeper into combining tirzepatide with lifestyle changes, check out our guide on doctor-approved weight loss advice combining injections with fitness. It’s a great resource for making your journey as smooth and effective as possible.
I’d love to hear about your experiences or questions regarding tirzepatide. Feel free to share in the comments below or connect with our community to exchange tips and support. Your journey matters, and together we can navigate the ups and downs of injectable fat loss treatments with confidence.
Decoding the Complex Interplay Between GIP and GLP-1 Receptors for Enhanced Fat Metabolism
Tirzepatide’s groundbreaking success in fat loss is largely attributed to its simultaneous activation of GIP and GLP-1 receptors, a synergy that redefines metabolic regulation. The GIP receptor’s role extends beyond insulin secretion; it influences adipocyte function by modulating lipid storage and mobilization. When paired with GLP-1 receptor activation, this dual agonism orchestrates a sophisticated metabolic shift favoring lipolysis over lipogenesis. This nuanced crosstalk between incretin pathways fine-tunes energy homeostasis, promoting a higher basal metabolic rate and improved fat oxidation efficiency.
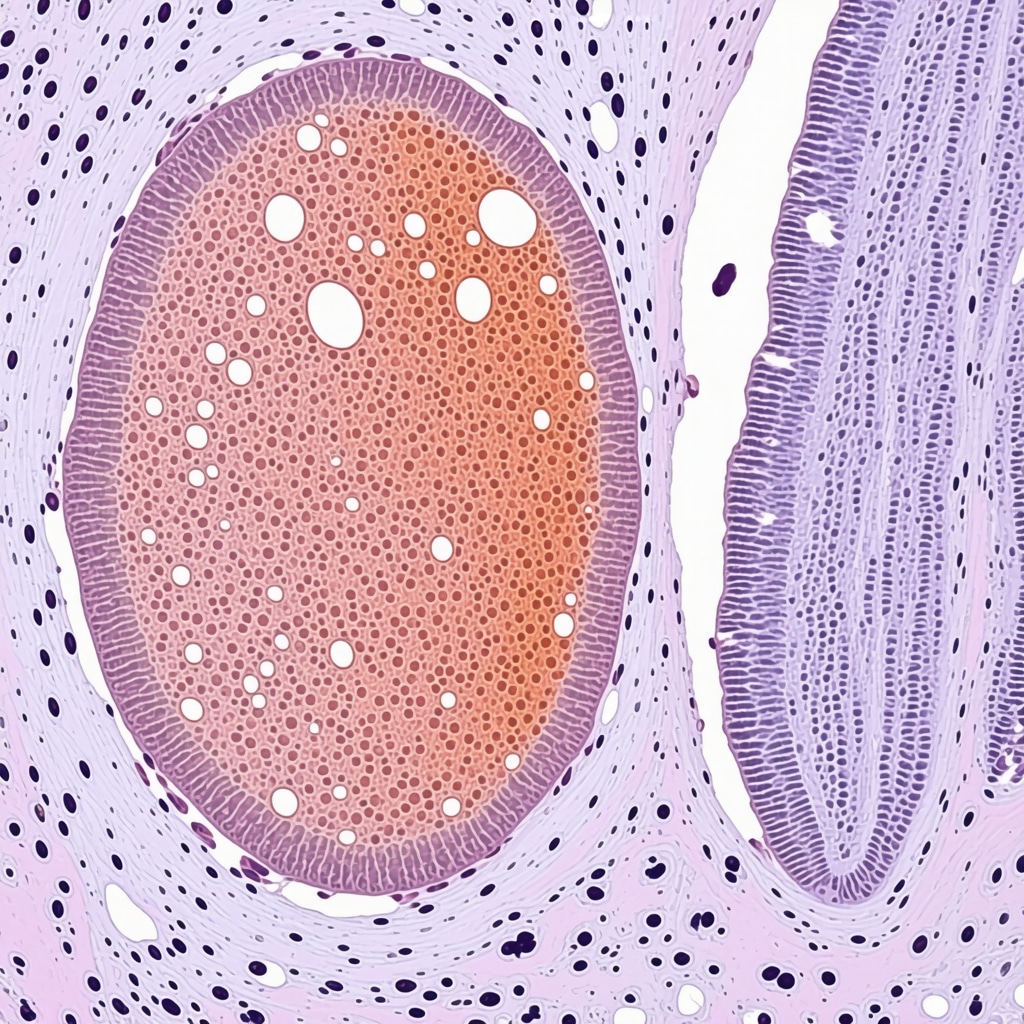
Recent molecular studies demonstrate that tirzepatide enhances mitochondrial biogenesis in adipose tissue, increasing the capacity for fatty acid oxidation. This effect is pivotal since mitochondrial dysfunction in adipocytes is a key contributor to obesity-associated insulin resistance. By restoring mitochondrial health, tirzepatide not only accelerates fat loss but also ameliorates metabolic dysfunction at a cellular level, a mechanism rarely targeted by conventional weight loss drugs.
Can Tirzepatide’s Dual Incretin Action Influence Brown Adipose Tissue Activation?
Emerging research suggests that tirzepatide may stimulate brown adipose tissue (BAT) thermogenesis through its dual incretin mechanism. BAT is specialized in energy expenditure via heat production, a process known as non-shivering thermogenesis. Activation of BAT increases total daily energy expenditure and facilitates fat loss beyond caloric restriction alone. While GLP-1 receptor agonists have shown some capacity to stimulate BAT activity, the addition of GIP receptor engagement in tirzepatide potentially amplifies this effect, offering a novel avenue for obesity treatment.
Understanding this interaction is critical for clinicians aiming to personalize therapy. Factors like genetic predisposition, baseline BAT activity, and patient metabolic profile may influence responsiveness to tirzepatide’s thermogenic effects, underscoring the importance of comprehensive metabolic assessments before and during treatment.
Optimizing Tirzepatide Therapy Through Precision Nutrition and Chronotherapy
To harness tirzepatide’s full therapeutic potential, integration with precision nutrition and chronotherapy principles is paramount. Nutritional strategies that complement incretin receptor activation—such as low glycemic index diets rich in polyphenols—may synergistically enhance insulin sensitivity and fat oxidation. Timing meals to align with circadian rhythms can also optimize metabolic responses, as incretin secretion is inherently tied to the body’s biological clock.
For example, administering tirzepatide in alignment with peak incretin receptor sensitivity and consuming nutrient-dense meals at strategic times can potentiate pharmacodynamic effects. This approach not only maximizes fat loss but also mitigates common side effects like nausea by smoothing gastrointestinal hormone fluctuations.
Leveraging Digital Health Tools for Personalized Tirzepatide Management
Incorporating digital health platforms into tirzepatide therapy presents a cutting-edge frontier for personalized medicine. Advanced apps capable of integrating continuous glucose monitoring, dietary intake, physical activity, and symptom tracking enable dynamic dose adjustments and early detection of adverse effects. These tools empower patients and clinicians to maintain adherence, optimize dosing schedules, and refine lifestyle interventions in real time.
Such precision management is supported by clinical evidence indicating improved treatment outcomes when pharmacotherapy is combined with digital behavioral coaching and feedback. This integrative strategy addresses the multifactorial nature of obesity and metabolic syndrome, positioning tirzepatide as a central component within a broader, patient-centered care paradigm.
For healthcare professionals seeking to deepen their understanding of tirzepatide’s mechanistic nuances and innovative integration strategies, the NCBI comprehensive review on dual incretin receptor agonists offers an authoritative resource.
Are you ready to explore tailored strategies that amplify tirzepatide’s efficacy in your weight management plan? Engage with our expert insights and join the conversation to unlock personalized solutions for sustainable fat loss and metabolic health.
Unlocking Molecular Synergies: The Frontier of Tirzepatide’s Dual Incretin Mechanism
Delving deeper into tirzepatide’s molecular orchestration reveals an intricate interplay between its dual incretin receptor agonism and adipose tissue remodeling. Beyond conventional glucose regulation, this agent modulates adipocyte differentiation and mitochondrial efficiency, fostering a metabolic milieu conducive to sustained lipolysis. Cutting-edge research elucidates how tirzepatide influences key transcription factors such as PPARγ and AMPK, pivotal in cellular energy homeostasis, thereby transcending mere appetite suppression to recalibrate systemic metabolism.
Chronopharmacology Meets Weight Loss: Timing Tirzepatide for Optimal Metabolic Impact
Emerging evidence highlights the significance of chronotherapy in enhancing tirzepatide’s efficacy. Aligning administration with circadian rhythms of incretin receptor expression can potentiate receptor responsiveness and downstream metabolic cascades. Patients might experience amplified fat oxidation and diminished gastrointestinal side effects when dosing coincides with endogenous hormone peaks. This temporal precision represents a promising paradigm, integrating pharmacokinetics with chronobiology to tailor individualized treatment regimens.
How Does Circadian Timing Influence Tirzepatide’s Pharmacodynamics and Patient Outcomes?
Exploring the temporal dynamics of tirzepatide reveals that receptor sensitivity and insulinotropic responses fluctuate diurnally, impacting therapeutic outcomes. Administering tirzepatide during periods of heightened GLP-1 and GIP receptor activity may enhance efficacy by synchronizing drug action with physiological hormone surges. Conversely, misaligned dosing could attenuate benefits and exacerbate side effects. Clinical trials investigating time-of-day dosing protocols are underway, promising refined guidelines for optimal chronotherapeutic application.
Harnessing Artificial Intelligence and Machine Learning for Personalized Tirzepatide Therapy
Integrating AI-driven analytics into patient management systems offers unprecedented precision in optimizing tirzepatide dosing. Machine learning algorithms can analyze multifactorial data streams—including genetics, metabolic biomarkers, lifestyle patterns, and drug response metrics—to predict individual treatment trajectories. This data-informed approach facilitates proactive dose adjustments, anticipates adverse events, and customizes supportive interventions, thereby enhancing safety and maximizing therapeutic gains.
Such innovations are transforming metabolic medicine, shifting from one-size-fits-all to dynamic, patient-centric models. Collaborations between endocrinologists, data scientists, and pharmacologists are essential to develop robust AI frameworks validated by clinical outcomes.
Evidence-Based Resources for Clinicians: Navigating Complexity with Authoritative Guidance
For healthcare professionals seeking to deepen their understanding of tirzepatide’s nuanced mechanisms and advanced management strategies, the NCBI comprehensive review on dual incretin receptor agonists is an indispensable resource. This peer-reviewed article synthesizes molecular insights, clinical trial data, and emerging therapeutic paradigms crucial for informed decision-making in complex metabolic disorder management.
Engage with these expert insights and elevate your clinical practice by incorporating precision chronotherapy and AI-assisted personalization into tirzepatide protocols. Explore tailored strategies now to unlock unparalleled fat loss and metabolic health outcomes.

Frequently Asked Questions (FAQ)
What is tirzepatide and how does it differ from other weight loss medications?
Tirzepatide is a novel dual incretin receptor agonist that activates both glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors. Unlike traditional GLP-1 receptor agonists, tirzepatide’s dual action not only reduces appetite but also enhances fat metabolism and insulin sensitivity, leading to more effective and sustained fat loss.
How does tirzepatide promote fat loss beyond appetite suppression?
Beyond reducing caloric intake, tirzepatide improves metabolic fat burning by enhancing lipolysis, mitochondrial biogenesis in adipose tissue, and increasing energy expenditure. Its activation of GIP receptors modulates adipocyte function to reduce fat storage and stimulate fat oxidation, contributing to significant reductions in body fat percentage, particularly visceral fat.
Can tirzepatide activate brown adipose tissue (BAT) to increase energy expenditure?
Emerging evidence suggests tirzepatide’s dual incretin mechanism may stimulate BAT thermogenesis, increasing non-shivering heat production and daily energy expenditure. This effect potentially amplifies fat loss beyond diet and exercise alone, although individual response may vary based on genetic and metabolic factors.
What are common side effects of tirzepatide and how can they be managed?
Common side effects include nausea, gastrointestinal discomfort, and occasional vomiting, especially during dose escalation. Gradual titration, timing injections to reduce daytime symptoms, hydration, and small frequent fiber-rich meals can improve tolerability. Close medical monitoring is essential to safely navigate these effects.
How important is timing and chronotherapy when administering tirzepatide?
Chronotherapy aligns tirzepatide dosing with circadian rhythms of incretin receptor activity, potentially enhancing drug efficacy and reducing side effects. Administering the medication during periods of peak receptor sensitivity may optimize fat oxidation and insulinotropic responses, although clinical guidelines are still evolving.
Can tirzepatide be combined with lifestyle changes for better outcomes?
Yes. Tirzepatide’s effectiveness is maximized when combined with precision nutrition, physical activity, and behavioral modifications tailored to the individual. Nutrient timing, low glycemic diets, and exercise synergize with tirzepatide’s metabolic effects to promote sustainable fat loss and metabolic health.
Is digital health technology beneficial in managing tirzepatide therapy?
Absolutely. Digital tools integrating glucose monitoring, symptom tracking, and lifestyle data allow for personalized dose adjustments and early side effect detection. This supports adherence and optimizes treatment outcomes through real-time feedback and tailored coaching.
Who should consider tirzepatide therapy for weight management?
Tirzepatide is primarily indicated for adults with obesity or overweight accompanied by metabolic conditions such as type 2 diabetes. However, therapy should be individualized, supervised by healthcare professionals, and considered alongside comprehensive lifestyle interventions.
Does tirzepatide affect long-term metabolic health beyond weight loss?
Yes. By improving insulin sensitivity, enhancing mitochondrial function, and reducing visceral adiposity, tirzepatide positively influences cardiovascular risk factors and metabolic syndrome components, supporting overall long-term metabolic health.
How is artificial intelligence shaping personalized tirzepatide therapy?
AI and machine learning analyze complex patient data—genetics, biomarkers, lifestyle—to predict responses and tailor dosing. This precision approach enables proactive management of side effects and optimizes therapeutic efficacy, heralding a new era in metabolic medicine.
Trusted External Sources
- The New England Journal of Medicine (NEJM): Provides high-impact clinical trial data on tirzepatide’s efficacy and safety, foundational for evidence-based practice.
- National Center for Biotechnology Information (NCBI): Offers comprehensive peer-reviewed reviews on dual incretin receptor agonists, including molecular mechanisms and emerging therapies.
- Endocrine Society Clinical Practice Guidelines: Authoritative guidelines on obesity pharmacotherapy and metabolic disorder management, informing safe and effective tirzepatide use.
- American Diabetes Association (ADA): Delivers consensus reports and research on diabetes treatments, including incretin-based therapies and their metabolic impacts.
- Obesity Society Publications: Specialized in obesity research, these publications provide insights into adipose tissue biology, pharmacological interventions, and integrative treatment strategies.
Conclusion
Tirzepatide represents an innovative advance in fat loss therapy through its unique dual agonism of GIP and GLP-1 receptors, delivering a multifaceted approach to weight management that transcends mere appetite suppression. Its capacity to enhance metabolic fat oxidation, improve insulin sensitivity, and promote adipose tissue remodeling positions it as a powerful tool against obesity and its associated metabolic disorders. Integrating tirzepatide with precision nutrition, chronotherapy, and digital health technologies amplifies its efficacy, enabling personalized, sustainable fat loss strategies. While managing side effects and ensuring safety remain paramount, ongoing research and clinical experience continue to refine its role within holistic treatment paradigms. Embracing these insights empowers both clinicians and patients to unlock tirzepatide’s full potential for transformative metabolic health. Share your experiences, explore further expert resources, and take an active role in advancing your fat loss journey with tirzepatide today.

The dual-action mechanism of tirzepatide offers an intriguing advancement in weight management by targeting both GIP and GLP-1 receptors, which seems to go beyond just appetite suppression and into enhancing fat metabolism directly. What I find particularly compelling is how this medication not only improves insulin sensitivity but also appears to promote mitochondrial biogenesis and even potentially activate brown adipose tissue thermogenesis. From a metabolic standpoint, this could mean more sustainable fat loss and improvements in metabolic health compared to traditional interventions.
In my experience with weight loss medications, side effects like nausea often discourage long-term adherence. The article’s emphasis on gradual dose escalation and lifestyle integration seems crucial for managing this. I also appreciate the nod to combining precision nutrition and chronotherapy, which signals a more personalized and holistic approach rather than a one-size-fits-all prescription.
I’m curious if others have tried to incorporate meal timing or specific dietary strategies alongside tirzepatide to maximize its effectiveness. Has anyone found a particular time or type of meal that helps balance the medication’s action and side effects better? It would be fascinating to discuss how individual variations in circadian rhythms or metabolism might intersect with tirzepatide therapy for customized fat loss outcomes.
Building on Maya Thompson’s insightful comment about the dual-action mechanism of tirzepatide, I want to highlight the importance of understanding how this medication’s unique targeting of both GIP and GLP-1 receptors reshapes fat metabolism. From my research, the synergy between these receptors does more than just reduce appetite; it actively increases the rate of fat oxidation and improves insulin sensitivity, which is crucial in reversing metabolic dysfunction common in obesity.
Regarding the question on meal timing, aligning food intake with the body’s circadian rhythm seems promising. I’ve read that consuming nutrient-dense, lower glycemic index meals during peak incretin receptor sensitivity—often in the morning to early afternoon—can optimize metabolic responses and minimize side effects like nausea. Evening administration of tirzepatide, as some users report, may also improve tolerability.
Has anyone experimented with specific dietary patterns such as intermittent fasting or time-restricted feeding alongside tirzepatide? It would be valuable to understand how these strategies affect both efficacy and side effect profiles. Furthermore, I wonder how closely monitoring energy expenditure and fat loss through digital tools could personalize treatment even more effectively. The interplay of medication timing, diet, and technology could be the frontier in achieving sustained fat loss while maintaining metabolic health.
I really appreciate the detailed insights on tirzepatide’s dual mechanism targeting both GIP and GLP-1 receptors. What stands out to me is how this approach not only tackles appetite suppression but also strategically enhances metabolic fat burning through improved insulin sensitivity and mitochondrial function. From what I’ve read and seen in some patient discussions, this receptor synergy could explain why tirzepatide outperforms older GLP-1 drugs, especially in visceral fat reduction—a critical factor for cardiovascular health.
Combining tirzepatide with lifestyle changes seems essential, and I find the emphasis on precision nutrition and chronotherapy intriguing. Personally, I’ve noticed that aligning my meal timing to earlier in the day, focusing on low glycemic index foods, has helped reduce the nausea side effects during treatment initiation. Additionally, staying consistent with tracking progress created a feedback loop that kept me motivated during plateaus.
Given the emerging research on brown adipose tissue activation by tirzepatide, I wonder how much individual variability in BAT activity influences treatment outcomes. Has anyone here had their BAT levels assessed or experimented with cold exposure or other methods to potentially boost brown fat activity alongside tirzepatide therapy? Exploring this could offer another lever to amplify fat loss effectiveness while supporting metabolic health.