Understanding Injection Fatigue in Tirzepatide Therapy: A Clinical Perspective
Tirzepatide, a novel dual GIP and GLP-1 receptor agonist, has revolutionized metabolic disorder management with its potent effects on glycemic control and weight reduction. However, long-term adherence to its injectable regimen can be compromised by injection fatigue, a multifactorial phenomenon characterized by psychological and physiological resistance to frequent subcutaneous administration. Appreciating the nuanced etiology of injection fatigue is essential for clinicians aiming to optimize therapeutic outcomes and patient quality of life.
Advanced Techniques to Mitigate Injection Site Discomfort and Enhance Patient Compliance
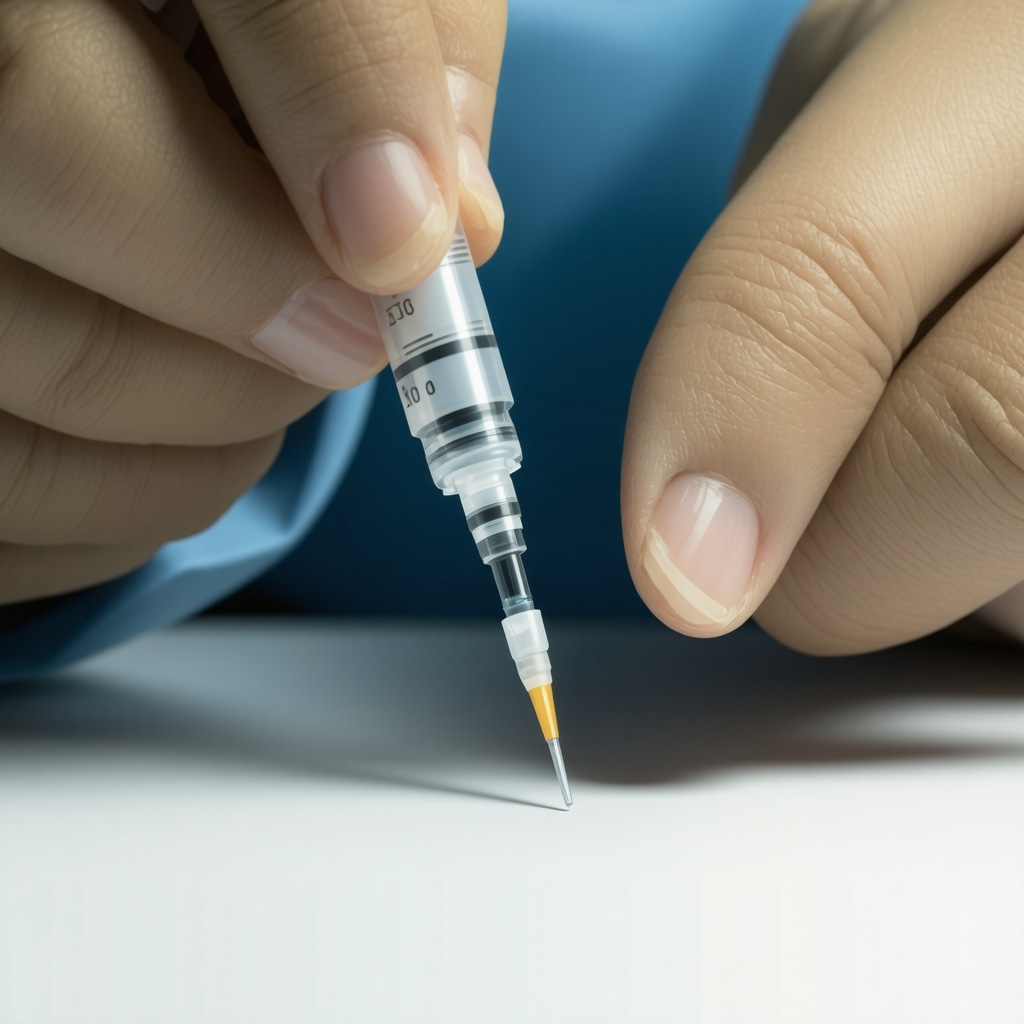
Injection site reactions, including pain, erythema, and lipodystrophy, significantly contribute to injection fatigue. Employing rotation protocols that systematically alternate injection sites between the abdomen, thigh, and upper arm mitigates localized tissue stress and promotes consistent absorption kinetics. Additionally, adopting fine-gauge needles and proper injection angles—typically 90 degrees for subcutaneous delivery—reduces tissue trauma. Patient education emphasizing aseptic technique and needle hygiene further prevents complications such as infections or bruising, corroborated by studies such as those published in the Journal of Diabetes Science and Technology.
Optimizing Injection Scheduling and Dosage to Balance Efficacy with Patient Tolerability
Strategically timing doses can alleviate psychological burden and physical side effects. Evidence suggests administering tirzepatide during times of day aligned with patients’ daily routines enhances adherence. Moreover, gradual dose escalation protocols reduce gastrointestinal adverse events, often precursors to injection discontinuation. Integrating tirzepatide use with tailored meal plans amplifies metabolic benefits while minimizing hunger-related discomfort, as explored in expert dietary strategies.
How Can Patients and Providers Collaborate to Overcome Psychological Barriers Associated with Injectable Therapies?
Injection fatigue is not solely physical; psychological barriers such as needle phobia, anxiety, and motivation lapses play critical roles. Collaborative patient-provider dialogue employing motivational interviewing techniques can identify individualized barriers and foster empowerment. Incorporating behavioral interventions, including cognitive-behavioral therapy or support groups, facilitates resilience and sustained engagement with tirzepatide therapy. Digital health tools offering injection reminders and progress tracking also bolster adherence, reflecting an integrative approach to managing injectable treatments.
Integrating Tirzepatide into Comprehensive Weight Loss Plans: Beyond the Injection
Maximizing the efficacy of tirzepatide extends beyond pharmacology. Combining injections with supervised exercise regimens and mindful eating practices addresses metabolic health holistically. Resources such as integrative therapy guides provide clinicians and patients with actionable frameworks to sustain weight loss and mitigate injection fatigue simultaneously.
For further expert insights on navigating injection fatigue safely and effectively, explore comprehensive strategies endorsed by medical professionals.
Leveraging Technology for Enhanced Tirzepatide Injection Adherence
Incorporating digital health innovations can significantly mitigate injection fatigue by providing real-time support and monitoring. Mobile applications equipped with injection reminders, symptom trackers, and motivational prompts empower patients to maintain consistent dosing schedules. Furthermore, telemedicine consultations allow healthcare providers to closely supervise treatment progress, promptly address adverse effects, and adapt regimens based on patient feedback. Such digital interventions complement traditional clinical strategies, fostering sustained engagement with tirzepatide therapy.
Personalizing Tirzepatide Dosing: Pharmacogenomics and Patient-Centered Approaches
Emerging evidence underscores the potential of pharmacogenomics to tailor tirzepatide dosing, optimizing efficacy while minimizing side effects that contribute to injection fatigue. Genetic polymorphisms affecting GLP-1 and GIP receptor sensitivity may influence individual responses, necessitating precise dose adjustments. Integrating patient-specific factors such as comorbidities, lifestyle, and psychological readiness further refines treatment plans. This personalized paradigm encourages adherence and enhances therapeutic outcomes, aligning with precision medicine principles highlighted in recent literature (Pharmacogenomics in Diabetes Management).
Addressing Nutritional Factors to Support Injection Tolerability and Weight Loss
Optimizing nutritional intake plays a pivotal role in reducing gastrointestinal side effects and improving patient comfort during tirzepatide therapy. Emphasizing balanced macronutrient distribution, adequate hydration, and small frequent meals can mitigate nausea and enhance energy levels. Careful meal planning also synergizes with tirzepatide’s appetite-suppressing effects, facilitating sustainable fat loss while preserving lean mass. For detailed dietary strategies, explore our guide on effective tirzepatide meal plans.
What Are the Cutting-Edge Behavioral Interventions to Combat Injection Fatigue in Long-Term Tirzepatide Users?
Beyond physiological considerations, behavioral science offers advanced frameworks to enhance adherence. Techniques such as habit stacking, where injections are paired with existing daily routines, reduce cognitive load and normalize therapy. Mindfulness-based stress reduction and biofeedback can alleviate anxiety associated with injections, while motivational incentives and peer support groups foster communal accountability. Clinicians integrating these evidence-based behavioral interventions can significantly improve patient persistence, ultimately translating into superior clinical outcomes.
Incorporating Physical Activity to Complement Tirzepatide Therapy and Reduce Injection Fatigue
Regular exercise not only amplifies weight loss effects but also improves metabolic flexibility and psychological well-being, which may attenuate injection fatigue. Structured programs combining aerobic and resistance training enhance insulin sensitivity and support lean muscle preservation. Moreover, physical activity serves as a positive behavioral reinforcement, countering treatment-related stress. Combining tirzepatide injections with tailored exercise regimens is therefore a holistic approach advocated in contemporary weight management practice (strength training integration with injectable therapies).
To explore more expert insights on overcoming injection fatigue and maximizing tirzepatide benefits, please visit our comprehensive strategies page or share your experiences in the comments below. Your contributions help foster a supportive community dedicated to effective and sustainable weight loss.
Neuropsychological Mechanisms Underpinning Injection Fatigue: Insights for Tailored Interventions
Injection fatigue in chronic tirzepatide users is increasingly recognized as a complex interplay of neuropsychological factors. The cumulative stress from repeated subcutaneous administration engages neural circuits implicated in pain perception, anxiety, and habituation. Functional imaging studies reveal altered activity in the anterior cingulate cortex and insular cortex during injection anticipation, contributing to heightened discomfort and avoidance behaviors. Understanding these pathways enables clinicians to deploy targeted interventions such as neurofeedback and desensitization protocols, which have demonstrated efficacy in reducing injection-related distress in analogous therapies (Neurobiological Bases of Injection-Related Anxiety).
Harnessing Artificial Intelligence to Personalize Injection Schedules and Predict Patient Adherence
The integration of machine learning algorithms into tirzepatide treatment regimens heralds a new era of personalized medicine. By analyzing patient-reported outcomes, biometric data, and behavioral patterns, AI models can forecast injection fatigue onset and recommend individualized dosing schedules that optimize tolerability and metabolic efficacy. Early pilot programs utilizing wearable sensors and app-based feedback loops have shown promise in dynamically adjusting injection timing and dosage to minimize adverse effects and enhance quality of life. This approach underscores the potential for technology-driven customization beyond static clinical guidelines.
What Are the Latest Pharmacological Adjuncts for Mitigating Injection Site Pain and Enhancing Tirzepatide Tolerability?
Recent pharmaceutical advancements focus on adjunct therapies to alleviate injection site discomfort associated with tirzepatide. Topical anesthetics such as liposomal lidocaine formulations provide localized analgesia with minimal systemic absorption, improving patient comfort during administration. Additionally, co-administration of anti-inflammatory agents targeting local cytokine release—currently under clinical investigation—may reduce erythema and swelling. These adjuncts, combined with optimized injection techniques, represent a multifaceted strategy to reduce physiological barriers to adherence, as detailed in Pharmacological Innovations in Injection Site Pain Management.
Exploring Epigenetic Influences on Tirzepatide Responsiveness and Injection Fatigue Propensity
Beyond genetic polymorphisms, epigenetic modifications such as DNA methylation and histone acetylation may modulate receptor expression and sensitivity, influencing both therapeutic response and side effect profiles. Preliminary studies suggest that environmental factors and lifestyle can induce epigenetic changes affecting GLP-1 and GIP receptor pathways, potentially altering patient susceptibility to injection fatigue. Epigenetic biomarkers could, therefore, serve as predictive tools for tailoring tirzepatide therapy and preemptively addressing adherence challenges. This frontier invites further research into integrating epigenomics into clinical decision-making.
Implementing Multidisciplinary Care Models to Sustain Long-Term Tirzepatide Therapy Engagement
Given the multifactorial nature of injection fatigue, a multidisciplinary approach involving endocrinologists, behavioral psychologists, dietitians, and physical therapists is paramount. Coordinated care plans that encompass psychological counseling, nutritional optimization, and physical rehabilitation can mitigate the diverse factors undermining adherence. Regular interdisciplinary case reviews and patient-centered goal setting foster a supportive environment conducive to sustained therapy engagement. This collaborative framework exemplifies best practices in chronic metabolic disease management.
For clinicians and patients eager to deepen their understanding of advanced strategies to combat injection fatigue, we invite you to explore our comprehensive resource library and participate in ongoing forums where expert insights and patient experiences converge.
Decoding Neuroimmune Interactions in Injection Fatigue: A Frontier for Innovative Therapeutics
Recent advances in neuroimmunology have illuminated the bidirectional communication between peripheral immune responses at injection sites and central nervous system processing, shaping the subjective experience of injection fatigue. Pro-inflammatory cytokines released locally can sensitize nociceptors, while systemic neuroimmune signaling modulates mood and motivation circuits, potentially exacerbating treatment aversion. Targeting these pathways with immunomodulatory agents or neuromodulation techniques could represent a novel adjunct to traditional symptomatic management, advancing the therapeutic index of tirzepatide.
Utilizing Real-World Data Analytics to Inform Personalized Tirzepatide Injection Protocols
The aggregation and analysis of real-world evidence (RWE) from diverse patient populations provide unprecedented insights into patterns of injection fatigue and treatment adherence. Leveraging big data and advanced analytics enables identification of demographic, behavioral, and clinical predictors of injection discontinuation. This data-driven approach informs the development of adaptive, patient-centric injection protocols and supports proactive intervention strategies, thus enhancing long-term outcomes in metabolic disease management.
How Can Precision Digital Therapeutics Be Integrated to Enhance Tirzepatide Injection Adherence and Patient Autonomy?
Precision digital therapeutics (PDTs) harness artificial intelligence and behavioral science to deliver tailored interventions that dynamically adjust to patient needs. Integrating PDTs with tirzepatide regimens offers real-time behavioral nudges, personalized educational content, and adaptive support modules that mitigate injection fatigue. These platforms empower patients through enhanced self-efficacy and continuous engagement, fostering sustained adherence. Clinical trials investigating PDT integration have demonstrated improvements in glycemic control and quality of life metrics, underscoring their transformative potential.
Synergizing Psychoneuroendocrinology Insights with Tirzepatide Management for Enhanced Patient Experience
Understanding the psychoneuroendocrine axes implicated in stress and reward processing provides a sophisticated framework to address injection fatigue. Chronic treatment stress can dysregulate hypothalamic-pituitary-adrenal (HPA) axis activity and alter dopaminergic reward pathways, diminishing treatment motivation. Interventions incorporating stress-reduction techniques, such as biofeedback and targeted pharmacotherapy, can recalibrate these systems, improving psychological resilience and treatment adherence in tirzepatide users.
Harnessing Cutting-Edge Biomaterials for Next-Generation Tirzepatide Delivery Systems
Innovations in biomaterial science have catalyzed the development of novel drug delivery platforms aimed at minimizing injection frequency and discomfort. Biodegradable microneedle arrays, implantable depots, and sustained-release hydrogels are under exploration to facilitate painless, controlled tirzepatide administration. These technologies promise to circumvent traditional injection challenges, substantially reducing injection fatigue and enhancing patient-centric care paradigms.
For a comprehensive review of these emerging modalities, refer to the authoritative analysis published in Nature Reviews Materials: Advanced Drug Delivery Systems.
Integrative Multimodal Approaches: Bridging Pharmacology, Psychology, and Technology
Optimizing tirzepatide therapy mandates a convergent strategy that synthesizes pharmacological optimization, behavioral health interventions, and technological augmentation. Multimodal programs incorporating dose personalization, cognitive-behavioral support, digital adherence tools, and physical activity regimens have demonstrated synergistic benefits. This holistic model addresses the multifactorial etiology of injection fatigue, promoting durable engagement and superior metabolic outcomes.
Ethical Considerations in AI-Driven Personalization of Tirzepatide Treatment
While artificial intelligence offers remarkable capabilities for individualizing injection schedules, ethical implications regarding data privacy, algorithmic bias, and patient autonomy warrant careful scrutiny. Transparent AI frameworks, patient-informed consent, and interdisciplinary oversight are essential to ensure equitable and ethical deployment of these technologies within clinical practice.
To explore these advanced insights and contribute to evolving best practices, engage with our expert-led forums and subscribe to our latest research updates for cutting-edge developments in tirzepatide therapy.
Expert Insights & Advanced Considerations
Integrating Neuropsychological Interventions for Sustainable Adherence
Injection fatigue is deeply intertwined with neuropsychological mechanisms that influence pain perception, anxiety, and motivation. Advanced interventions such as cognitive-behavioral therapy, neurofeedback, and mindfulness-based stress reduction can recalibrate neural pathways implicated in injection-related distress, fostering long-term adherence and enhancing patient experience during tirzepatide therapy.
Leveraging Artificial Intelligence for Personalized Injection Management
The application of AI-driven predictive models enables clinicians to anticipate injection fatigue onset and customize dosing schedules dynamically. By analyzing biometric and behavioral data, these tailored regimens minimize adverse effects and optimize metabolic outcomes, representing a transformative step beyond traditional, one-size-fits-all protocols.
Multidisciplinary Care as a Cornerstone for Addressing Injection Fatigue
A collaborative model engaging endocrinologists, behavioral psychologists, dietitians, and physical therapists offers a holistic framework to tackle the multifactorial nature of injection fatigue. This integrated approach ensures comprehensive support encompassing psychological resilience, nutritional optimization, and physical wellness, thereby sustaining long-term tirzepatide therapy engagement.
Emerging Biomaterial Technologies for Next-Generation Delivery Systems
Innovations such as biodegradable microneedle arrays and sustained-release hydrogels promise to revolutionize tirzepatide administration by reducing injection frequency and discomfort. These biomaterial advances have the potential to significantly diminish physiological barriers, thus mitigating injection fatigue and increasing patient-centered treatment adherence.
Epigenetics: A New Frontier in Predicting and Managing Injection Fatigue
Epigenetic modifications affecting GLP-1 and GIP receptor pathways may influence individual responsiveness and side effect profiles. Understanding these mechanisms could lead to predictive biomarkers that personalize tirzepatide therapy further, allowing preemptive strategies to prevent injection fatigue and optimize therapeutic benefits.
Curated Expert Resources
1. “Pharmacogenomics in Diabetes Management”: A comprehensive review detailing genetic influences on GLP-1 receptor agonist responsiveness, essential for understanding patient-specific dosing considerations (PMC9256197).
2. “Neurobiological Bases of Injection-Related Anxiety”: An authoritative article exploring neural circuits involved in injection anticipation and pain, fundamental for designing neuropsychological interventions (PMC7326765).
3. “Nature Reviews Materials: Advanced Drug Delivery Systems”: Insightful analysis on cutting-edge biomaterials for sustained and painless drug delivery, pivotal for future tirzepatide administration strategies (Nature Reviews Materials).
4. Expert Tirzepatide Meal Plans and Injection Fatigue Strategies: Practical and evidence-based guidance combining nutritional planning with tirzepatide therapy to mitigate injection fatigue and enhance metabolic outcomes (effective tirzepatide meal plans).
5. Doctor-Approved Weight Loss Advice on Overcoming Injection Fatigue Safely: A professional resource offering comprehensive strategies for managing injection fatigue and maintaining adherence in injectable therapies (doctor-approved advice).
Final Expert Perspective
In addressing injection fatigue within tirzepatide therapy, an integrative, precision-focused approach is paramount. Understanding the intricate neuropsychological, genetic, and immunological underpinnings enables clinicians to deploy multifaceted strategies that transcend mere injection technique adjustments. Coupled with technological innovations such as AI personalization and biomaterial advancements, these insights pave the way for enhanced patient adherence and optimized metabolic health outcomes. As the field evolves, continuous engagement with emerging research and multidisciplinary collaboration will remain essential.
For clinicians and patients aiming to deepen their expertise and optimize tirzepatide therapy, exploring comprehensive resources like effective tirzepatide meal plans and doctor-approved weight loss advice is highly recommended. Engage with professional communities and remain informed to sustain therapeutic success and elevate patient care standards.