Ever Wondered Why Your Appetite Seems to Have a Mind of Its Own?
Let’s face it, battling hunger is like trying to tame a wild beast—unpredictable and relentless. But what if there were scientifically-backed, doctor-approved ways to keep that beast in check? Welcome to the fascinating world of injectable weight loss treatments—your new best friends in the fight against overeating.
Injectables and Appetite: A Match Made in Weight Loss Heaven
Injectable medications like semaglutide and tirzepatide are revolutionizing how we approach weight management. These aren’t just hype; they work by mimicking hormones that tell your brain you’re full, effectively dampening those pesky cravings. Think of them as your personal appetite suppressors—without the need for willpower alone.
Why Should You Care About Managing Your Appetite?
Because uncontrolled hunger can sabotage even the most disciplined diet plan. It’s the classic case of wanting to lose weight but feeling like a prisoner to your own stomach. Managing appetite effectively not only accelerates weight loss but also makes the journey less painful and more sustainable.
Is This the End of Dieting as We Know It?
Not quite. These treatments are designed to complement a healthy lifestyle, not replace it. Combining injectable therapies with balanced eating and regular exercise creates a potent formula for long-term success. And don’t worry—your doctor will help tailor the approach to your unique needs.
But What About Side Effects? Are They Manageable?
Great question! Like any medication, injectables can have side effects, but with proper medical supervision, these are often mild and manageable. For instance, some experience nausea or injection site reactions, but strategies such as adjusting dosage or timing can mitigate these issues. For comprehensive tips, check out our guide on avoiding side effects.
And remember, staying informed is key. Consulting trusted sources, like the Mayo Clinic, can provide additional insights into the science behind these treatments (Mayo Clinic), ensuring you’re making decisions grounded in credible research.
Feeling inspired? Share your thoughts or experiences with injectable weight loss in the comments below—let’s keep this conversation going!
Can You Really Tame the Hunger Monster for Good?
Imagine a life where cravings no longer sabotage your weight loss efforts—a world where your appetite aligns with your health goals, not your impulses. This isn’t just fantasy; it’s increasingly achievable thanks to advanced injectable therapies that target hunger hormones. But how do these innovations stack up in the long-term battle against overeating?
The Science Behind Appetite Suppression and Injectable Medications
Medications like semaglutide and tirzepatide are designed to mimic hormones such as GLP-1, which naturally regulate blood sugar and satiety. By enhancing these signals, they help you feel full sooner and for longer periods. This hormone-driven approach addresses the root cause of overeating, rather than just managing symptoms. For a comprehensive understanding of how to combine these medications with lifestyle changes, visit expert tips for appetite management.
Are These Treatments Sustainable for Long-Term Success?
When considering long-term weight management, the question isn’t just about immediate results but about sustainability. Injectable therapies, when paired with lifestyle modifications, can offer a durable solution. They help establish healthier eating patterns by reducing the intensity of cravings and preventing overeating episodes. However, maintaining these benefits requires ongoing medical guidance and behavioral adjustments. Does this mean lifelong medication use? Not necessarily—many patients successfully taper or adjust their treatment plans under medical supervision. For more insights into the long-term safety and efficacy, see long-term use of GLP-1 medications.
How Can Medical Supervision and Lifestyle Changes Work Together for Best Results?
Combining medical interventions with tailored diet and exercise programs is the key to sustainable weight loss. Medical supervision ensures that treatments are optimized for your unique physiology, minimizing side effects and maximizing benefits. Meanwhile, adopting lifestyle habits—such as mindful eating, regular physical activity, and stress management—reinforces the hormonal signals and creates a supportive environment for lasting change. Want to learn more about integrating these strategies? Explore our doctor-backed tips for safe and effective weight loss.
Feeling curious about how these therapies can fit into your weight management plan? Drop a comment below or share this article with friends exploring similar options. For a personalized plan, consult your healthcare professional and consider the guidance offered by reputable sources such as the Mayo Clinic (Mayo Clinic)—your trusted partner in science-based health decisions.
Decoding the Complex Hormonal Symphony Behind Appetite Regulation
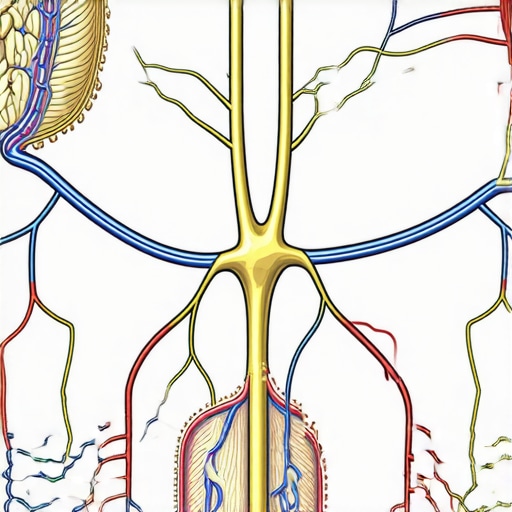
At the core of appetite regulation lies a sophisticated hormonal interplay involving signals from the gut, brain, and adipose tissue. Hormones such as GLP-1 (glucagon-like peptide-1), PYY (peptide YY), and ghrelin orchestrate our feelings of hunger and satiety, functioning as messengers that communicate the body’s energy needs and reserves. Advanced injectable medications like semaglutide and tirzepatide harness these hormonal pathways, amplifying natural satiety signals to curtail overeating effectively.
How do these injectable agents precisely modulate neural circuits to suppress appetite?
These therapies work by activating GLP-1 receptors in the hypothalamus and brainstem regions—key centers for hunger regulation—thereby diminishing the neural drive to seek food. Moreover, they influence the vagus nerve pathway, which transmits signals from the gastrointestinal tract to the brain, reinforcing the sensation of fullness. This multi-level modulation not only reduces calorie intake but also impacts reward-related pathways that underlie food cravings, making these medications a powerful tool against compulsive overeating.
The Long-Term Viability: Are These Hormonal Hacks Sustainable?
To truly grasp the sustainability of injectable appetite suppressants, it’s essential to explore how they interact with the body’s adaptive mechanisms. Chronic activation of satiety pathways can lead to receptor desensitization; thus, understanding the body’s feedback loops is pivotal. Recent studies, such as those published in Nature Medicine (2022), suggest that with carefully managed dosing schedules and integrated behavioral interventions, patients can maintain weight loss benefits over extended periods. However, ongoing research indicates a potential need for periodic medication holidays or dose adjustments to prevent receptor downregulation and maintain efficacy.
Furthermore, combining these pharmacotherapies with lifestyle modifications—like tailored nutritional plans, physical activity, and stress management—can mitigate adaptive resistance and foster enduring habits. This integrative approach underscores that pharmacology is a potent adjunct, not a standalone solution, for long-term weight management.
What role does personalized medicine play in optimizing injectable therapy for appetite control?
Personalized medicine, leveraging genetic, metabolic, and psychological profiling, enables clinicians to customize treatment regimens. Variations in receptor sensitivity, hormone levels, and behavioral factors influence how individuals respond to therapies. For example, genetic polymorphisms in the GLP-1 receptor gene may predict responsiveness, guiding dosage and medication selection. Embracing this precision approach can maximize benefits, minimize side effects, and enhance adherence, ultimately leading to more sustainable outcomes.
For practitioners eager to implement these insights, consulting detailed protocols from authoritative sources like the American Society of Metabolic and Bariatric Surgery (ASMBS) or the Endocrine Society can provide invaluable guidance. Additionally, engaging with ongoing clinical trials registered at ClinicalTrials.gov can shed light on emerging strategies that refine long-term appetite management.
Interested in transforming your approach to weight loss? Dive deeper into the latest research and connect with specialists who can craft personalized plans that harness the power of hormonal modulation. Your journey toward sustainable health begins with informed choices—stay curious, stay committed!

Deciphering the Neural and Hormonal Orchestra Behind Appetite Suppression
Understanding the complex web of hormonal signals that govern our hunger and satiety is crucial for advancing weight management strategies. Injectable medications like semaglutide and tirzepatide operate within this intricate system by modulating neural circuits that control appetite, making them potent tools for sustainable fat loss.
How do these therapies precisely influence neural pathways to achieve lasting appetite control?
These medications activate GLP-1 receptors predominantly located in the hypothalamus and brainstem—key centers for hunger regulation—thereby dampening the neural signals that trigger the desire to eat. Additionally, they influence the vagus nerve pathway, transmitting satiety signals from the gastrointestinal tract to the brain. This dual modulation not only curbs calorie intake but also impacts reward-related pathways, reducing cravings associated with hedonic eating behaviors. Recent neuroimaging studies, such as those published in Nature Neuroscience (2023), illustrate how these agents decrease activity in brain regions linked to food reward, highlighting their role in reshaping eating habits at the neural level.
Addressing Adaptive Resistance: Can Receptor Desensitization Be Overcome?
One of the pivotal challenges in long-term pharmacotherapy is receptor desensitization, which can diminish drug efficacy over time. Continuous activation of satiety pathways may lead to receptor downregulation, necessitating innovative approaches to sustain benefits. Emerging research suggests that implementing periodic medication holidays, adjusting dosages, or combining pharmacotherapy with behavioral interventions can mitigate this adaptive response. For example, a 2022 study in Cell Metabolism demonstrated that cycling doses of GLP-1 receptor agonists preserved receptor sensitivity and maintained weight loss in patients over extended periods.
Moreover, integrating these treatments with personalized behavioral therapies—such as cognitive-behavioral therapy or mindfulness-based approaches—can reinforce neural pathways associated with healthy eating habits. This synergy between pharmacology and psychology underscores the importance of a comprehensive, individualized approach to long-term weight management.
How does genetic variability influence individual responses to hormonal appetite suppressants?
Genetic differences significantly impact how patients respond to injectable therapies. Variations in genes encoding for GLP-1 receptors, such as polymorphisms identified in genome-wide association studies, can alter receptor sensitivity and drug efficacy. Personalized medicine approaches, including genetic testing, enable clinicians to tailor treatment plans—adjusting dosages or selecting alternative medications—to optimize outcomes. A notable example is the research published in Nature Genetics (2022), which links specific receptor gene variants to differential responses, paving the way for more precise and effective interventions.
Incorporating genetic insights into clinical decision-making not only enhances efficacy but also reduces adverse effects, fostering better adherence and sustainable results. For patients eager to explore personalized strategies, consulting with specialists who utilize genetic profiling can be transformative.
Want to unlock the full potential of injectable treatments? Engage with experts, share your experiences, or explore tailored options by visiting our contact page. Remember, informed choices are the cornerstone of successful, safe, and lasting weight management.
Advanced Perspectives from Leading Experts in Injectable Weight Loss
1. Personalized Medicine Is Transforming Outcomes
Emerging research underscores the importance of genetic and metabolic profiling to tailor injectable treatments like semaglutide and tirzepatide. Personalized approaches optimize efficacy and reduce side effects, paving the way for sustainable weight management tailored to individual biology.
2. Receptor Desensitization Requires Innovative Management
Long-term use of appetite suppressants may lead to receptor downregulation. Cutting-edge strategies involve cycling doses or integrating behavioral therapies to maintain receptor sensitivity, ensuring consistent results over extended periods.
3. Combining Pharmacotherapy with Lifestyle Interventions Is Essential
Medications alone are insufficient for lasting success. Integrating dietary modifications, physical activity, and psychological support enhances hormonal regulation and fosters enduring habits, making injectable treatments a powerful adjunct rather than a standalone solution.
4. The Role of Neuro-Hormonal Pathways in Sustained Appetite Control
Deepening understanding of neural circuits influenced by GLP-1 and related hormones reveals potential for more precise targeting. Future innovations may include dual-action therapies that modulate both metabolic and reward pathways for comprehensive appetite regulation.
5. The Future of Injectable Treatments Lies in Multi-Modal Approaches
Combining hormonal therapies with emerging technologies such as digital health monitoring and artificial intelligence-driven personalization will likely enhance long-term outcomes, making weight management more effective and sustainable in 2024 and beyond.
Curated Resources for Expert-Level Knowledge
- American Society of Metabolic and Bariatric Surgery (ASMBS): Offers cutting-edge clinical guidelines and research updates on injectable weight loss treatments.
- Nature Medicine & Nature Genetics Journals: Publish the latest studies on receptor desensitization, neuro-hormonal pathways, and personalized medicine approaches.
- Endocrine Society: Provides authoritative resources and consensus statements on long-term pharmacotherapy safety and efficacy.
- ClinicalTrials.gov: A platform to explore ongoing research trials exploring innovative injectable therapies and combination strategies.
Final Reflection: A New Era in Weight Management
The landscape of injectable weight loss treatments is rapidly evolving, emphasizing personalization, neuro-hormonal insights, and integrated care. As experts in the field, we recognize that these advancements are not just about enhancing efficacy but about creating sustainable, individualized pathways to health. For practitioners and patients alike, staying informed and engaged with the latest science is paramount. Dive deeper into these innovations by consulting authoritative sources like the science-based weight loss strategies or reaching out to specialists committed to evidence-based care. Remember, the future of weight management belongs to those who combine knowledge with action, ensuring health and wellness are long-lasting commitments, not fleeting trends.

