Injectable Weight Loss: The New Frontier or a Medical Minefield?
Let’s face it: the world of weight loss has gone from fad diets to fancy pharmaceuticals faster than you can say “miracle cure.” Injectable medications like Ozempic and Wegovy have become the talk of the town—and for good reason. But with great power comes great responsibility, especially when it involves your health. Are these doctor-backed treatments a game-changer or a risky gamble? Buckle up, because we’re diving into the bright, sometimes murky waters of injectable weight loss.
Why Are Doctors So Excited About Injectable Weight Loss?
It’s simple: these injections harness the power of GLP-1 receptor agonists, which help regulate appetite and blood sugar. This isn’t just hype; scientific studies show significant weight loss results when used under medical supervision. According to a comprehensive review, patients experience not only fat loss but also improved metabolic health—a win-win for everyone tired of yo-yo dieting. But remember, it’s not just about losing pounds; it’s about doing it safely and sustainably.
Are These Treatments Safe? Or Just a Shortcut to Trouble?
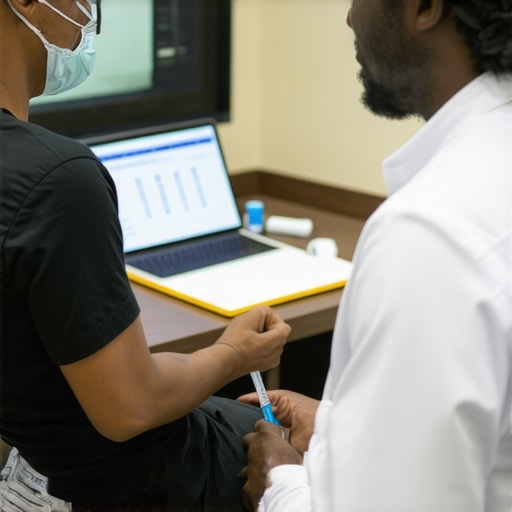
This is the million-dollar question. While many patients report positive outcomes, safety is paramount. Side effects such as nausea, injection site reactions, or even rare complications demand professional oversight. That’s where the doctor-backed approach shines. Physicians can tailor doses, monitor progress, and intervene if anything’s amiss. For example, proper injection techniques and timing—like following recommended weekly schedules—are crucial to minimize discomfort and side effects.
Can You Really Trust Your Doctor to Keep You Safe?
Absolutely! When it comes to prescription injections, self-medicating is like playing Russian roulette with your health. Always seek medical guidance—your doctor is your best ally in navigating this new landscape. They can assess your health, review your medications, and ensure you’re a good candidate. Plus, a doctor can help you integrate these treatments with lifestyle changes, making your weight loss journey more effective and safer. For more insights, check out this expert guide.
And don’t forget, long-term success isn’t just about the shot; it’s about building habits and maintaining those results. Curious how to maximize your outcomes? Dive into our comprehensive strategies at this detailed article.
So, fellow weight loss warriors, the bottom line is clear: injectable treatments backed by medical professionals can be powerful allies—if used wisely. Share your thoughts below or reach out via our contact page to start your safe, doctor-guided journey today!
How Can Medical Professionals Fine-Tune Injectable Treatments for Maximum Success?
As the landscape of injectable weight loss evolves, one question arises: how can physicians optimize these treatments to ensure safety and efficacy? The key lies in personalized medicine, where each patient’s unique health profile guides dosage and treatment plans. This tailored approach not only minimizes side effects but also enhances long-term results, making the journey sustainable. For instance, adjusting medication doses based on individual responses helps prevent issues like nausea or injection site reactions, which are common concerns among newcomers to these therapies. Moreover, integrating these medications with comprehensive lifestyle interventions—such as diet modifications and exercise—magnifies their benefits. For detailed insights, explore this expert guide.
Are We Overlooking the Long-Term Implications of Injectable Weight Loss?
The conversation often centers around immediate weight loss results, but what about the long-term safety and health outcomes? Experts emphasize that while these medications can be potent tools, their long-term use requires careful monitoring and ongoing research. There’s a growing body of evidence suggesting that with proper medical oversight, these treatments can be part of a sustainable weight management plan—yet, gaps in data remain. For example, understanding how these drugs impact metabolic health and hormonal balance over years is crucial. Physicians should consider periodic assessments and possibly tapering strategies to ensure that weight loss is maintained without compromising overall health. Staying informed through reputable sources like this scientific review can help guide responsible use.
What Innovative Approaches Are Emerging to Enhance Injectable Weight Loss?
As science advances, new methods are emerging to boost the effectiveness of injectable treatments. Combining medications with emerging technologies such as digital health monitoring or behavioral coaching can lead to more consistent outcomes. For example, apps that track injection schedules, side effects, and lifestyle changes empower patients to stay engaged and compliant. Additionally, research into novel drug formulations aims to extend the duration of action, reducing injection frequency and improving adherence. These innovations promise a future where injectable weight loss is not only more effective but also more patient-friendly. To explore cutting-edge strategies, visit this comprehensive resource.
If you’ve found this information valuable, please share your thoughts or questions below! For personalized guidance, don’t hesitate to contact us through our contact page. Staying informed and proactive is the best way to harness the power of medical science safely and effectively on your weight loss journey.
Harnessing Precision Medicine: Tailoring Injectable Weight Loss for Maximum Impact
As the landscape of obesity management evolves, one of the most promising frontiers is personalized medicine. Achieving optimal results with injectable weight loss treatments like GLP-1 receptor agonists hinges on customizing protocols to individual patient profiles. This approach involves a comprehensive assessment of factors such as metabolic rate, hormonal milieu, comorbidities, and even genetic predispositions. By leveraging advanced diagnostics—like pharmacogenomic testing—clinicians can fine-tune dosages and treatment durations, thereby enhancing efficacy and minimizing adverse effects.
For instance, patients with a predisposition to gastrointestinal sensitivity might benefit from gradual dose escalation, while those with insulin resistance may require specific adjustments to optimize glycemic control alongside weight loss objectives. Integrating continuous glucose monitoring data and behavioral analytics into treatment planning further refines this personalization. This holistic strategy not only accelerates weight reduction but also fosters sustainable habits, turning short-term interventions into long-lasting health transformations.
The Nuanced Role of Long-Term Monitoring and Adjustments
While the initial phase of injectable weight loss often garners attention, the true mastery lies in long-term management. Experts emphasize that ongoing monitoring is essential to identify subtle shifts in metabolic health, hormonal balance, and psychological well-being. Regular assessments—including blood panels, body composition analyses, and even gut microbiome evaluations—offer invaluable insights into how the body adapts over time.
Moreover, adaptive dosing strategies can be employed to maintain weight loss momentum and prevent plateaus. For example, clinicians might implement tapering protocols or incorporate intermittent breaks to assess the body’s response, thereby reducing dependency and fostering intrinsic motivation. This dynamic, patient-centric approach ensures that treatment remains safe, effective, and aligned with evolving health goals.
Emerging Technologies: The Next Leap in Injectable Weight Loss
Innovation is driving a new era of precision delivery and patient engagement. Digital health platforms—integrating wearable devices, mobile apps, and telehealth—empower both clinicians and patients to track progress in real-time. These tools can automate reminders for injections, monitor side effects, and provide behavioral coaching, creating a seamless support system that enhances adherence.
On the pharmaceutical front, research into longer-acting formulations aims to reduce injection frequency, thereby improving compliance and quality of life. Biodegradable microspheres and sustained-release implants are under investigation, promising to revolutionize treatment paradigms. Furthermore, combining injectable therapies with adjunct technologies such as virtual reality-based counseling or AI-driven predictive analytics could unlock new levels of personalization and effectiveness.
For those eager to explore cutting-edge developments, reputable sources like the National Institutes of Health offer in-depth scientific insights. Staying abreast of these innovations ensures that healthcare providers can offer evidence-based, forward-thinking solutions tailored to each patient’s unique journey.
If you’re serious about leveraging the latest in injectable weight loss science, consider consulting with a specialist who can craft a bespoke plan that adapts as your body responds. Remember, the future of weight management is not just about losing pounds—it’s about transforming health through precision, innovation, and expert guidance.
Harnessing Genetic and Hormonal Profiling to Optimize Injectable Weight Loss Outcomes
Emerging research underscores the importance of integrating genetic and hormonal data into treatment plans. Pharmacogenomics, for instance, allows clinicians to tailor GLP-1 receptor agonist dosages based on individual genetic markers, potentially reducing side effects and enhancing efficacy. Studies published in this comprehensive review highlight how genetic variability influences drug response, paving the way for truly personalized therapies. Incorporating hormonal assessments—such as thyroid function and sex hormone levels—further refines treatment, ensuring that metabolic and endocrine factors support sustained weight management.
How Can Advanced Diagnostics Revolutionize Long-Term Management of Injectable Weight Loss?
Integrating continuous monitoring tools, like real-time glucose sensors and wearable biofeedback devices, facilitates dynamic adjustments to treatment. This proactive approach minimizes risks of weight regain and hormonal imbalance. For example, real-time glucose data can inform dose modifications, preventing hypoglycemia or hyperglycemia episodes that might compromise safety. Additionally, periodic microbiome analyses can identify gut flora imbalances affecting appetite regulation, allowing for targeted interventions that complement pharmacotherapy. Experts advocate that such comprehensive diagnostics transform weight loss from a static process into an adaptive, precision medicine journey.
Exploring Novel Drug Delivery Systems for Enhanced Patient Adherence
Innovations in pharmaceutical technology aim to extend the duration of action for injectable medications, reducing injection frequency and improving adherence. Biodegradable microspheres, implantable devices, and nanotechnology-based systems are under active research. For instance, long-acting formulations could deliver therapeutic doses over several months, decreasing the burden of weekly injections. Such advancements not only improve patient compliance but also stabilize blood levels, reducing side effects associated with fluctuating drug concentrations. As outlined in latest scientific literature, these systems hold promise for transforming injectable weight loss into a more manageable, less invasive process.

Visualize innovative drug delivery systems like implantable microchips or sustained-release microspheres designed for long-term medication release, with labels highlighting their benefits for adherence and safety.
Integrating Behavioral and Lifestyle Data for Holistic Weight Management
Beyond pharmacology, the future of injectable weight loss involves merging behavioral analytics with medical data. Digital platforms that track sleep patterns, stress levels, and dietary habits can provide insights into psychological and environmental factors influencing weight. Machine learning algorithms analyze these datasets to recommend personalized lifestyle modifications, optimizing treatment outcomes. This holistic approach recognizes that sustainable weight management requires addressing behavioral drivers alongside medical intervention. Experts emphasize that combining data-driven behavioral coaching with targeted injections maximizes long-term success and resilience against weight regain.
What Role Will Artificial Intelligence Play in Personalizing Injectable Weight Loss Regimens?
AI-driven models are poised to revolutionize treatment customization by predicting individual responses to various medications based on vast datasets. These predictive analytics can recommend optimal dosing schedules, identify potential adverse reactions, and suggest lifestyle adjustments tailored to each patient’s unique profile. For example, AI algorithms analyzing genetic, hormonal, and behavioral data might forecast which patients will benefit most from specific formulations or dosing frequencies. This technological leap transforms weight loss from a standardized protocol into a bespoke, adaptive process, substantially increasing the likelihood of sustained success.
Expert Insights & Advanced Considerations
Personalized Medicine is Transforming Outcomes
Top clinicians emphasize tailoring injectable weight loss therapies based on genetic, hormonal, and metabolic profiles. Incorporating pharmacogenomic testing enables precise dosage adjustments, reducing side effects and enhancing efficacy, thereby turning weight management into a highly individualized process.
Long-Term Monitoring is Critical for Success
Continuous assessment of metabolic health, hormonal balance, and psychological well-being ensures sustained results. Regular blood panels, body composition analyses, and microbiome evaluations help clinicians adapt treatment plans, preventing plateaus and relapse.
Emerging Technologies Drive Innovation
The integration of digital health tools such as wearable biosensors, mobile health apps, and telemedicine platforms enables real-time monitoring and personalized coaching. These advancements improve adherence, optimize dosing, and support holistic health management.
Genetic and Hormonal Profiling Optimizes Treatment
Analyzing genetic markers and hormone levels refines therapy. For example, individuals with specific SNPs may respond better to certain GLP-1 receptor agonists, allowing for more effective and safer interventions.
Next-Generation Drug Delivery Systems Enhance Adherence
Innovations like long-acting injectables, biodegradable microspheres, and implantable devices reduce injection frequency, improving patient compliance and stability of drug levels, thus elevating treatment success.
Curated Expert Resources
- National Institutes of Health (NIH): Provides comprehensive scientific research on pharmacogenomics and long-term safety of GLP-1 therapies, essential for advanced understanding.
- PubMed Central: Hosts peer-reviewed articles and reviews on emerging injectable formulations and personalized medicine approaches in weight management.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Offers guidelines and expert consensus on integrating surgical and medical weight loss strategies with emerging injectable therapies.
- ClinicalTrials.gov: Tracks ongoing studies on novel drug delivery systems and combined digital health interventions, keeping practitioners informed of cutting-edge developments.
Final Expert Perspective
Harnessing the full potential of injectable weight loss demands a sophisticated blend of personalized medicine, innovative delivery systems, and technology-driven monitoring. As we advance, the integration of genetic, hormonal, and behavioral data will redefine success, making weight management safer, more effective, and truly tailored. For healthcare providers and patients alike, staying informed and engaged with these frontier strategies is essential. If you’re ready to elevate your approach, consider consulting with specialists who can craft a bespoke plan—because in this field, the future belongs to those who innovate and adapt. For more in-depth insights, explore this resource or this guide. Your journey to optimal health begins with knowledge and expert guidance.”},