When Sweat Meets Science: The New Frontier of Weight Loss
Imagine this: you’re lacing up your sneakers, ready to hit the gym, when you remember your weekly injectable weight loss treatment waiting patiently in the fridge. It’s not just any treatment — it’s a doctor-approved, science-backed addition to your fitness journey. The marriage of exercise and injectables like GLP-1 receptor agonists has become the talk of the town, and for good reason. This dynamic duo is reshaping how we think about shedding pounds, blending the old-fashioned grind of physical activity with cutting-edge medical innovation.
Injectables and Exercise: Should They Be Best Friends?
Doctors increasingly recommend combining lifestyle changes with injectable medications for weight loss, acknowledging that neither approach alone is a silver bullet. Medications like semaglutide or tirzepatide can help regulate appetite and improve metabolic health, but without the complementary boost of exercise, the journey might feel incomplete. According to a recent study published in the National Center for Biotechnology Information, integrating physical activity with GLP-1 therapies amplifies fat loss, improves insulin sensitivity, and helps maintain muscle mass.
Can You Really Outsmart Your Body Without Moving a Muscle?
Let’s face it: the allure of a magic injection that melts fat while you binge-watch your favorite show is tempting. But even the most effective injectable treatments work best when paired with regular exercise. Not only does physical activity help burn calories, but it also enhances the body’s responsiveness to these medications. Think of injectables as the spark and exercise as the fuel that keeps the fire of fat loss blazing.
What’s fascinating is how exercise complements the appetite regulation side effects of these injectables. Many patients report reduced hunger pangs, which makes sticking to a balanced diet and workout routine far less daunting. It’s a harmonious interplay that many doctors now emphasize in their weight loss protocols.
Injectables Are Powerful—But They’re Not Standalone Superheroes
One of the key pieces of doctor-approved advice is to view injectables as tools rather than cures. They assist but don’t replace the foundational pillars of healthy living: exercise and mindful eating. Pairing your weekly injections with workouts tailored to your fitness level not only accelerates fat loss but supports cardiovascular health and mental well-being. The synergy here is undeniable — as highlighted in this insightful guide, customizing your approach can turn a challenging weight loss journey into an achievable lifestyle transformation.
So, whether you’re a gym rat or a casual walker, incorporating movement amplifies the benefits of your injectable regimen. The trick? Finding a balance that suits your body, schedule, and preferences.
Ready to Share Your Success Story or Ask the Experts?
Weight loss isn’t a solo mission — it’s a community effort. If you’ve experimented with combining exercise and injectable treatments or are curious about how to start, drop a comment below or explore more doctor-approved strategies by connecting with our expert team. Your journey could inspire someone else!
Enhancing Injectable Weight Loss: The Role of Tailored Exercise Programs
Understanding how exercise synergizes with injectable weight loss medications like semaglutide or tirzepatide is crucial for optimizing outcomes. Tailored physical activity programs, designed around individual fitness levels and health status, can significantly enhance the efficacy of these treatments. For example, moderate-intensity aerobic exercise combined with resistance training not only promotes fat loss but also preserves lean muscle mass, which is vital for metabolic health.
Additionally, exercise stimulates mitochondrial biogenesis and improves insulin sensitivity, mechanisms that complement the pharmacological actions of GLP-1 receptor agonists. By fostering a metabolic environment conducive to fat oxidation, physical activity works hand in hand with injectables to accelerate and sustain weight loss.
How Can Personalized Fitness Plans Unlock Greater Benefits from Injectable Therapies?
Personalization is the cornerstone of effective fat loss strategies involving injectables. Fitness plans that consider factors such as age, comorbidities, and lifestyle preferences enable patients to adhere consistently and safely. Moreover, integrating behavior change techniques like goal setting and self-monitoring can further enhance adherence and motivation.
Experts recommend collaborating with healthcare providers to develop comprehensive plans that incorporate exercise, diet, and medication management. This multidisciplinary approach ensures that therapy is holistic and adaptive, minimizing plateaus and maximizing fat loss results over time.
Addressing Common Challenges in Combining Exercise and Injectable Weight Loss Treatments
Despite the clear benefits, some patients encounter barriers such as fatigue, injection site discomfort, or motivational lapses. Managing these challenges proactively is essential. Strategies include scheduling workouts during periods of peak energy, rotating injection sites as advised in this guide on injection site care, and leveraging social support or professional coaching.
Furthermore, maintaining hydration and balanced nutrition supports both exercise performance and medication effectiveness. Regular follow-up with healthcare professionals ensures timely adjustments and addresses any side effects or concerns swiftly.
What Does the Latest Research Say About Combining Injectables with Exercise?
A 2023 publication in the Journal of the American Medical Association Internal Medicine highlights that patients using GLP-1 receptor agonists who engaged in structured exercise programs experienced significantly greater weight loss and improvements in glycemic control compared to those relying on medication alone. This underscores the indispensable role of physical activity in achieving optimal health outcomes alongside injectable therapies.
Join the Conversation: Share Your Experience or Learn More
Are you currently combining exercise with your injectable weight loss treatment? What challenges or successes have you encountered? Sharing your journey can provide valuable insights to others navigating similar paths. Feel free to comment below or explore further expert-backed advice on safe semaglutide use and combining diet with injectable treatments. Your engagement enriches the community and fosters informed, empowered weight loss journeys.
Unlocking the Metabolic Symphony: How Injectables and Exercise Orchestrate Fat Loss at a Cellular Level
Beyond the surface, the interaction between injectable weight loss medications such as GLP-1 receptor agonists and exercise triggers a complex metabolic symphony. At the cellular level, these agents modulate pathways that regulate appetite and glucose metabolism, while exercise induces mitochondrial biogenesis and enhances oxidative capacity. This biochemical duet amplifies energy expenditure and optimizes substrate utilization, fundamentally reshaping body composition.
Emerging research illustrates that exercise-induced increases in AMP-activated protein kinase (AMPK) activity synergize with GLP-1 agonists to enhance lipid oxidation and reduce adipocyte size. These molecular mechanisms not only promote fat loss but also improve insulin sensitivity and cardiovascular markers, contributing to comprehensive metabolic health.
What are the molecular mechanisms by which exercise enhances the efficacy of GLP-1 receptor agonists?
The synergy between exercise and GLP-1 receptor agonists pivots on several interrelated molecular processes. Exercise activates AMPK and peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), which stimulate mitochondrial biogenesis and fatty acid oxidation. Concurrently, GLP-1 agonists modulate pancreatic beta cell function and reduce glucagon secretion, improving glycemic control. Together, these effects optimize metabolic flexibility by shifting energy utilization towards fats rather than carbohydrates, facilitating sustained weight loss.
Moreover, exercise enhances the expression of GLP-1 receptors in peripheral tissues, potentially increasing drug responsiveness. This receptor upregulation creates a positive feedback loop that magnifies the therapeutic benefits of injectable treatments.
For a detailed exploration of these mechanisms, refer to the comprehensive review published in Frontiers in Endocrinology, which synthesizes current evidence on exercise-induced modulation of incretin-based therapies.
Designing Precision Exercise Protocols: Beyond Generic Recommendations to Tailored Interventions
While general advice encourages aerobic and resistance training, the frontier of weight loss optimization lies in personalization—crafting exercise programs that align intricately with an individual’s metabolic profile, medication schedule, and lifestyle constraints. High-intensity interval training (HIIT), for instance, has shown promise in augmenting the benefits of GLP-1 receptor agonists by rapidly improving insulin sensitivity and cardiovascular fitness within shorter durations.
Equally, resistance training combats the risk of muscle loss commonly associated with calorie deficits and pharmacological interventions, preserving lean mass which is crucial for maintaining basal metabolic rate. Integrating neuromuscular electrical stimulation (NMES) or functional movement exercises can further refine outcomes, particularly for patients with mobility limitations.
How can exercise timing and intensity be optimized to complement injectable weight loss treatments?
Timing exercise sessions to coincide with peak pharmacodynamic effects of injectables can enhance patient outcomes. For example, scheduling workouts during periods when GLP-1 receptor agonist plasma concentrations are highest may maximize appetite suppression and glucose control, permitting more effective energy expenditure and better glycemic responses.
Intensity modulation also matters: moderate-to-high intensity sessions stimulate greater metabolic adaptations without inducing excessive fatigue that could impair medication adherence. Incorporating periodization strategies, alternating between different exercise intensities and modalities, sustains engagement and mitigates plateau effects.
Overcoming Real-World Barriers: Integrative Solutions for Sustained Engagement and Adherence
Despite scientific understanding, practical challenges often impede the ideal integration of exercise with injectable therapies. Fatigue, injection site discomfort, and psychological barriers can diminish motivation and consistency. Addressing these requires an interdisciplinary approach involving behavioral psychology, physical therapy, and pharmacological management.
Utilizing digital health tools such as wearable fitness trackers and mobile apps can promote self-monitoring and provide real-time feedback, fostering accountability. Cognitive-behavioral techniques, including motivational interviewing and goal-setting frameworks, empower patients to navigate lapses and maintain long-term commitment.
Healthcare providers should encourage open communication channels, enabling timely adjustments to medication regimens or exercise prescriptions based on patient feedback and progress assessments.
Join the Expert Dialogue: Elevate Your Weight Loss Journey with Customized Insights
If you’re eager to refine your weight loss strategy by harmonizing injectable treatments with tailored exercise regimens, we invite you to engage with our expert content. Explore advanced protocols, share your experiences, and receive personalized guidance by connecting with our specialist team here. Empower your journey with science-backed precision and community support.
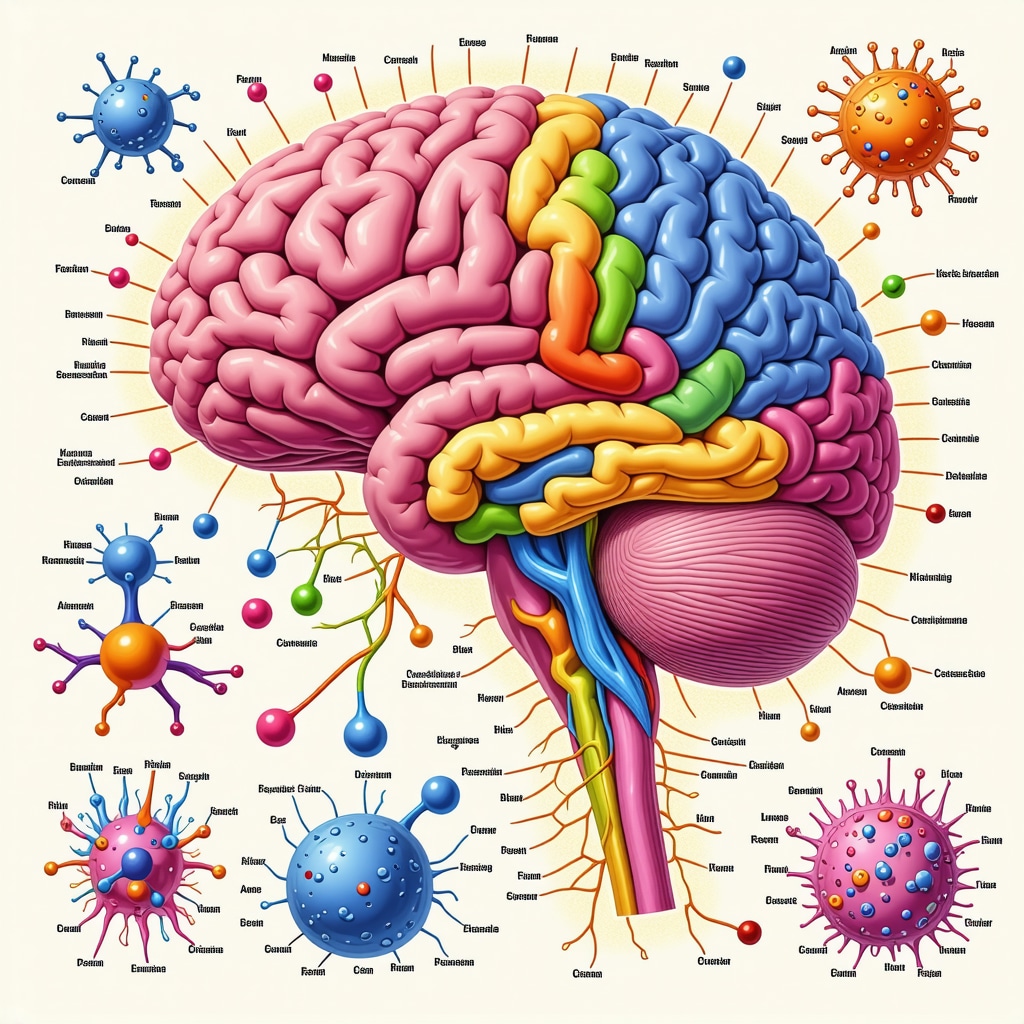
Neuroendocrine Nuances: How Exercise Modulates GLP-1 Pathways Beyond Appetite Suppression
While GLP-1 receptor agonists are celebrated for their appetite suppression and glycemic control, emerging evidence suggests that exercise exerts profound neuroendocrine influences that further prime these pathways. Physical activity stimulates the release of endogenous incretins and neuropeptides, such as peptide YY and brain-derived neurotrophic factor (BDNF), which synergistically amplify the pharmacodynamics of injectables. This neuroendocrine crosstalk enhances satiety signaling and mood regulation, potentially mitigating emotional eating—a common barrier during weight loss.
Moreover, exercise-induced improvements in hypothalamic sensitivity may recalibrate energy homeostasis, augmenting the efficacy of GLP-1 agonists. Understanding these subtleties enriches the rationale for integrating personalized fitness regimens with injectable therapies, transcending mere calorie burning.
How Does Exercise Influence Central Nervous System Mechanisms to Complement Injectable Weight Loss Medications?
Exercise activates multiple central nervous system (CNS) pathways that modulate appetite and reward mechanisms. Specifically, aerobic and resistance training elevate BDNF levels, which support neuroplasticity and improve hypothalamic function related to hunger and satiety. Concurrently, increased endogenous GLP-1 secretion during exercise may potentiate the effects of exogenous GLP-1 receptor agonists, fostering enhanced appetite regulation.
A recent study published in Scientific Reports demonstrates that exercise-induced neurochemical adaptations improve insulin sensitivity and modulate dopaminergic signaling, which can reduce food cravings and improve adherence to weight loss protocols. These CNS modulations, combined with pharmacotherapy, create a robust framework for sustainable fat loss and metabolic health.
Integrating Chronobiology: Timing Exercise to Synchronize with Injectable Pharmacokinetics for Maximum Impact
Chronobiology—the study of biological rhythms—offers intriguing insights into optimizing exercise schedules to complement injectable weight loss treatments. Circadian variations influence hormone secretion, metabolism, and drug pharmacokinetics, suggesting that timing workouts to align with peak medication plasma levels can enhance therapeutic outcomes.
For instance, scheduling moderate-to-high intensity exercise sessions during the period when semaglutide or tirzepatide concentrations are at their apex may potentiate appetite suppression and improve post-exercise glucose metabolism. This strategic timing leverages the synergistic effects of exercise and injectables, potentially accelerating fat oxidation and improving insulin action.
Can Aligning Exercise Timing with Injectable Dosing Enhance Metabolic Outcomes?
Preliminary clinical observations advocate for exercise sessions within 4–8 hours post-injection, coinciding with peak GLP-1 receptor agonist activity. This window appears optimal for maximizing appetite control and glucose homeostasis, reducing compensatory overeating, and fostering improved energy expenditure. Tailoring workout timing also mitigates fatigue and optimizes patient adherence.
Further research is ongoing, but integrating chronotherapeutic principles into personalized weight loss plans embodies a cutting-edge approach increasingly endorsed in physician-guided strategies, such as those detailed in this comprehensive guide.
Behavioral Economics and Motivation: Leveraging Cognitive Strategies to Sustain Exercise and Injectable Therapy Synergy
Weight loss success hinges not only on biological synergy but also on sustained behavioral adherence. Incorporating principles from behavioral economics—such as nudges, incentives, and framing—can bolster motivation to maintain consistent exercise alongside injectable regimens.
Techniques such as implementation intentions (pre-planned exercise scheduling), loss aversion framing (highlighting risks of non-adherence), and social accountability (peer support groups or coaching) have demonstrated efficacy in improving long-term engagement. Digital platforms integrating reminders and progress tracking further enhance adherence, bridging the gap between intention and action.
How Can Behavioral Interventions Be Tailored to Support Patients Combining Exercise with Injectable Weight Loss Therapies?
Customized behavioral strategies that acknowledge individual psychological profiles, barriers, and preferences maximize engagement. Healthcare providers play a pivotal role in crafting these interventions, often collaborating with psychologists and exercise specialists to deliver multidisciplinary care. Evidence-based frameworks, such as motivational interviewing, complement these efforts by enhancing intrinsic motivation and self-efficacy.
For practical, doctor-approved guidance on maintaining motivation and managing side effects during injectable therapy, explore this resource, which offers nuanced tips for integrating mind and body approaches.
Join the Dialogue: How Have You Personalized Your Exercise and Injectable Weight Loss Journey?
Your unique experience enriches the collective understanding and inspires others navigating similar paths. Share your insights, challenges, or questions in the comments below, or connect directly with our expert team for tailored advice through our consultation portal. Together, we can unlock the full potential of science and lifestyle synergy for transformative fat loss.
Expert Insights & Advanced Considerations
Synergistic Metabolic Adaptations Amplify Fat Loss
Injectable weight loss medications such as GLP-1 receptor agonists and tailored exercise regimens interact at the molecular level to enhance mitochondrial biogenesis and lipid oxidation. This synergy not only accelerates fat loss but also improves insulin sensitivity, creating a metabolic environment favorable for sustainable weight reduction. Recognizing this interplay aids clinicians and patients in crafting strategies that go beyond calorie counting to target cellular energy metabolism effectively.
Personalized Exercise Timing Optimizes Pharmacodynamics
Aligning physical activity schedules with peak plasma concentrations of injectables maximizes therapeutic impact. For instance, exercising within 4–8 hours post-injection harnesses optimal appetite suppression and glycemic control, reducing compensatory overeating. Incorporating chronobiological principles into weight loss plans allows for precision medicine approaches that improve adherence and metabolic outcomes.
Behavioral Economics Enhances Long-Term Adherence
Integrating cognitive-behavioral strategies such as implementation intentions, social accountability, and motivational interviewing supports patients in maintaining consistent exercise alongside injectable therapies. These approaches address psychological barriers and leverage intrinsic motivation, which is crucial for overcoming fatigue, injection site discomfort, and emotional eating, thereby fostering sustainable lifestyle transformation.
Customized Resistance Training Preserves Lean Mass During Caloric Deficits
Resistance training tailored to individual fitness levels counteracts muscle loss often observed during calorie restriction and pharmacotherapy. Preserving lean muscle mass maintains basal metabolic rate and supports cardiovascular health, ensuring that weight loss is primarily from fat stores. This nuanced approach enhances both physical function and metabolic resilience.
Neuroendocrine Modulation Extends Beyond Appetite Control
Exercise induces the release of endogenous incretins and neuropeptides such as BDNF, which enhance hypothalamic sensitivity and satiety signaling. This neuroendocrine crosstalk augments the pharmacodynamics of GLP-1 receptor agonists, mitigating emotional eating and improving mood regulation. Understanding these mechanisms encourages a holistic view of weight loss that integrates mind-body interactions.
Curated Expert Resources
- Frontiers in Endocrinology Review on Exercise and Incretin Therapies: A comprehensive synthesis of molecular mechanisms linking physical activity with GLP-1 receptor agonist efficacy, valuable for understanding biochemical synergies.
- Journal of the American Medical Association Internal Medicine (2023): Clinical evidence supporting combined exercise and injectable therapy for superior weight loss and glycemic control outcomes.
- eWeightLossTips Physician-Guided Fat Loss Injections: Detailed guidance on customizing fat loss injections and exercise plans to individual metabolic profiles, available here.
- Behavioral Economics in Weight Management: Resources on applying cognitive strategies to enhance motivation and adherence during combined injectable and exercise therapy.
- Chronobiology and Pharmacotherapy Integration: Insights into optimizing medication timing with lifestyle interventions to maximize metabolic benefits.
Final Expert Perspective
Combining injectable weight loss treatments with personalized exercise regimens represents a frontier where molecular science meets practical lifestyle medicine. The metabolic and neuroendocrine synergies elucidated through current research emphasize that success hinges not merely on medication but on strategic, individualized physical activity and behavioral support. This integrated approach transforms injectable therapies from isolated interventions into components of a comprehensive, adaptable weight loss ecosystem.
For those navigating this sophisticated landscape, continuous learning and collaboration with healthcare professionals are paramount. Explore advanced protocols, share your journey, and access expert advice on safe semaglutide use or connect directly with specialists via our consultation portal. Empower your weight loss journey with insight, precision, and community support.


I really appreciate how this article emphasizes the importance of integrating exercise with injectable weight loss treatments. I’ve personally found that pairing moderate walking routines with my weekly semaglutide injections makes a noticeable difference in my energy levels and cravings. It’s fascinating how targeted exercise timing, especially post-injection, could further enhance results, as some studies suggest. Has anyone experimented with timing their workouts around their medication schedules to see improved outcomes? I’m curious about strategies that others have used, especially for those with busy schedules or limited mobility. The insights on personalized programs and behavioral support resonate with me—sticking to a routine can be challenging, but understanding the science behind it adds motivation. Looking forward to hearing more success stories or tips on combining these approaches effectively.