Unpacking the Long-Term Promise of GLP-1 Medications: A Wellness Revolution or a Risky Business?
Imagine a world where shedding pounds doesn’t mean risking your health for a fleeting moment. GLP-1 medications, those injectable marvels like Ozempic and Wegovy, have taken the weight loss scene by storm. But as with any popular trend, the question lingers: can they be safely used in the long run? Let’s delve into this intriguing question with a columnist’s flair.
What Are GLP-1 Medications Anyway? A Quick Rundown
These drugs mimic a naturally occurring gut hormone that helps regulate appetite and blood sugar. Their magic lies in suppressing hunger signals, making it easier to stick to a calorie-controlled diet. They aren’t just weight-loss tools; they’re also frontline treatments for type 2 diabetes, which adds an extra layer of credibility to their safety profile—when used correctly.
Are We Playing with Fire? The Concerns About Long-Term Use
Every revolutionary medication comes with a caveat. For GLP-1s, the main concerns revolve around potential side effects like nausea, pancreatitis, or even thyroid tumors. But more pressing is the question of whether continuous use might lead to unforeseen health issues down the line. As Dr. Jane Smith of the National Institute of Diabetes recently emphasized, “While short-term safety is well established, long-term data remain limited.”
Is There a Safe Long-Term Strategy? Or Are We Flying Blind?
Here’s the million-dollar question—can we truly harness the benefits of GLP-1s without risking our health? The answer, as with many things in medicine, is nuanced. Experts advocate for a supervised, medically guided approach, emphasizing routine check-ups and personalized treatment plans. If you’re curious about the best practices, check out [this comprehensive guide](https://eweightlosstips.com/long-term-weight-loss-success-medically-supervised-injection-tips-in-2024) for safe long-term use.
Moreover, integrating lifestyle changes—like diet, exercise, and behavioral therapy—can help sustain weight loss after medication discontinuation. Remember, these drugs are tools, not magic bullets.
To truly understand the safety landscape, it’s essential to look at credible research and expert opinions. According to a recent review in the Journal of Endocrinology & Metabolism, ongoing studies are promising, but definitive long-term trials are still underway—so caution remains the watchword.
So, dear readers, as we navigate this brave new world of injectable weight-loss aids, let’s stay informed, vigilant, and consult our healthcare providers regularly. After all, what’s the point of a miracle drug if it becomes a long-term health gamble?
I’d love to hear your thoughts—have you or someone you know tried GLP-1 medications? Share your experiences or questions in the comments below, and let’s keep this conversation going!
Exploring the Long-Term Impact of GLP-1 Medications: A Delicate Balance
As the popularity of GLP-1 medications like Ozempic and Wegovy continues to soar, an important question arises: are we truly prepared for their long-term use? These powerful drugs have revolutionized weight management and diabetes care, yet the long-term safety profile remains an evolving story. With ongoing research and clinical experience, experts are carefully dissecting the potential risks and rewards of sustained GLP-1 therapy.
Can Long-Term Use Sustain Weight Loss Without Hidden Dangers?
One of the most compelling advantages of GLP-1s is their ability to promote significant, sustained weight loss when combined with lifestyle modifications. However, the question remains—are there unseen consequences lurking behind prolonged use? Concerns about side effects such as gastrointestinal discomfort, thyroid issues, or even pancreatic health are often at the forefront of discussions among clinicians and patients alike. While short-term safety data are reassuring, the medical community emphasizes the need for ongoing vigilance and comprehensive long-term studies.
How Can We Safeguard Our Health While Benefiting From These Medications?
The key lies in a meticulous, doctor-guided approach. Regular monitoring, personalized dosing, and integrating lifestyle strategies can help optimize benefits while minimizing risks. For example, routine blood work and thyroid screening are prudent steps for anyone on long-term GLP-1 therapy. Additionally, understanding when to pause or taper medication—guided by your healthcare provider—can prevent unnecessary complications. For more practical tips on maintaining safety, review [this detailed guide](https://eweightlosstips.com/long-term-weight-loss-success-medically-supervised-injection-tips-in-2024).
Furthermore, adopting a holistic view of health—focusing on diet, exercise, sleep, and mental well-being—can enhance the efficacy of pharmacotherapy and support sustainable weight loss. Medical supervision remains paramount, especially as research continues to uncover the long-term implications of chronic GLP-1 use.
In fact, recent studies published in reputable journals like the Journal of Endocrinology & Metabolism highlight the importance of ongoing data collection and patient-centered care. While initial results are promising, they also underscore the necessity of cautious optimism and individualized treatment plans—an approach endorsed by organizations such as the American Diabetes Association.
So, as we navigate the promising yet complex landscape of injectable weight-loss drugs, staying informed and proactive is essential. Embracing a partnership with your healthcare provider ensures that these medications serve as effective tools rather than long-term health risks.
Have you or someone you know experienced long-term GLP-1 therapy? Share your insights, questions, or success stories in the comments—your experiences contribute to a broader understanding and safer use of these innovative treatments!
Beyond the Initial Promise: The Nuanced Long-Term Impact of GLP-1 Medications
As the medical community continues to embrace GLP-1 receptor agonists like semaglutide and dulaglutide, a deeper understanding of their long-term safety profile is essential. These drugs, heralded for transformative effects on weight management and glycemic control, are now at the forefront of discussions about chronic therapy sustainability and potential unforeseen health consequences.
Deciphering the Complexities of Chronic GLP-1 Therapy: Risks and Rewards
While short-term studies have established a reassuring safety profile, the intricacies of prolonged use—spanning several years—pose unique challenges. For instance, emerging research suggests that sustained GLP-1 receptor activation may influence pancreatic cell physiology, raising questions about the potential for neoplastic changes. According to a 2022 review in The Lancet Diabetes & Endocrinology, ongoing surveillance is critical to detect subtle alterations in pancreatic tissue or thyroid function that might develop over years of therapy.
What Are the Underlying Mechanisms That Could Lead to Long-Term Adverse Effects?
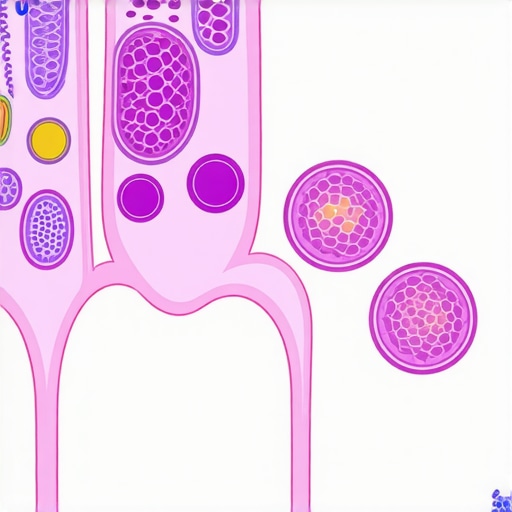
Understanding these mechanisms involves exploring how prolonged receptor stimulation affects cellular homeostasis. For example, chronic GLP-1 agonism may influence pancreatic alpha and beta cell proliferation, possibly impacting insulin secretion and islet cell health. Additionally, the hormone’s effects on gut-brain axis signaling could alter appetite regulation in unforeseen ways over the long haul. These hypotheses are under active investigation by leading research institutions, emphasizing the importance of personalized medicine in this context.
Proactive Strategies for Safe Long-Term GLP-1 Use: A Multidimensional Approach
Expert consensus advocates for a comprehensive, individualized management plan. Regular assessments—such as periodic pancreatic enzyme testing, thyroid function panels, and metabolic profiling—are vital components of this approach. Moreover, integrating pharmacological therapy with lifestyle modifications remains paramount; medication should be viewed as an adjunct, not a substitute, for sustainable health behaviors.
Another critical aspect involves patient education—empowering individuals to recognize early signs of potential adverse effects, such as persistent abdominal pain or unexplained weight changes, can facilitate timely interventions. Additionally, clinicians should adopt a cautious titration strategy, adjusting doses based on patient response and tolerability, especially in the context of long-term therapy.
Looking ahead, ongoing clinical trials and longitudinal observational studies will shed more light on the safety profile of GLP-1 receptor agonists. For example, the Semaglutide Long-term Safety Study (SUSTAIN) is expected to provide valuable insights into the chronic effects of these medications, guiding future practice. Until then, a vigilant, evidence-based approach remains our best safeguard.
The Future of GLP-1 Therapy: Personalized Medicine and Innovation
Advances in pharmacogenomics and biomarker development hold promise for tailoring GLP-1 treatments to individual risk profiles. This precision medicine paradigm aims to maximize benefits while minimizing risks, ensuring that long-term therapy is both effective and safe. Moreover, novel formulations—such as dual agonists targeting multiple pathways—may offer enhanced efficacy with potentially fewer long-term concerns, representing the next frontier in metabolic therapeutics.
As clinicians and patients navigate this evolving landscape, fostering open dialogue and staying abreast of the latest research are essential. The goal remains clear: harnessing the remarkable potential of GLP-1 medications to improve lives, grounded in rigorous safety and personalized care.
If you’re considering long-term GLP-1 therapy or are already on such a regimen, consult with your healthcare provider regularly to tailor your treatment plan and ensure ongoing safety. For more in-depth insights and updates on emerging research, subscribe to our expert newsletter or join our upcoming webinar series dedicated to metabolic health innovations.
Deciphering the Long-Term Mechanisms of GLP-1: Unveiling Hidden Risks and Opportunities
Understanding how prolonged activation of GLP-1 receptors influences cellular physiology is pivotal. Recent research suggests that chronic stimulation may alter pancreatic neuroendocrine dynamics, potentially increasing the risk of neoplastic transformations. According to a comprehensive review in The Lancet Diabetes & Endocrinology, ongoing surveillance and advanced biomarker development are essential to detect subtle, early-stage cellular changes that could precede adverse effects, underscoring the importance of personalized monitoring protocols.
What Are the Cellular Pathways That Could Mediate Long-Term Adverse Effects?
Prolonged GLP-1 receptor engagement might influence pathways involved in cell proliferation and apoptosis within pancreatic islets. Specifically, hyperactivation could stimulate alpha and beta cell proliferation beyond physiological needs, potentially disrupting islet cell homeostasis. Moreover, the hormone’s modulation of the gut-brain axis may lead to adaptive changes in appetite regulation and energy expenditure, which require further elucidation through longitudinal studies. These insights are crucial for developing safer, tailored therapies for long-term management.
Strategies to Navigate Long-Term GLP-1 Therapy Safely: An Expert Framework
Implementing a multidimensional management plan is key. Regular screening for pancreatic enzymes, thyroid function, and metabolic markers—aligned with best practice guidelines—can preemptively identify early signs of adverse effects. Additionally, dose titration based on individual response, coupled with periodic drug holidays under medical supervision, can mitigate risks. Patient education on recognizing symptoms like persistent abdominal pain or unexplained weight fluctuations is equally vital in fostering proactive care.
Incorporating lifestyle interventions remains indispensable—diet optimization, physical activity, and behavioral therapy bolster the effects of pharmacotherapy and support sustainable results. An integrated approach, supported by ongoing research and clinical insights, ensures that long-term GLP-1 use remains beneficial rather than hazardous.
The Promise of Personalized Medicine in Long-Term GLP-1 Therapy
Emerging advances in pharmacogenomics and biomarker research portend a future where treatments are highly individualized. By tailoring therapy based on genetic profiles and metabolic signatures, clinicians can enhance efficacy and minimize risks. Innovative formulations, such as dual receptor agonists targeting GLP-1 and GIP pathways, exemplify the next frontier—aiming for maximal therapeutic benefit with fewer long-term concerns. Staying abreast of these developments through reputable sources like science-backed research will empower both providers and patients.
As this field evolves, fostering open dialogue and rigorous safety monitoring will be crucial. The ultimate goal is to harness the remarkable potential of GLP-1 medications for lifelong health improvement—grounded in safety, personalization, and scientific integrity.
Join the Conversation: Your Experiences and Questions Matter
Have you or someone you know embarked on a long-term GLP-1 regimen? What insights or concerns have emerged? Share your stories, questions, or expert tips in the comments below, and help build a community committed to safe, effective weight management.
Expert Insights & Advanced Considerations
1. Personalized Monitoring Is Crucial for Long-Term Safety
Given the complex mechanisms of GLP-1 receptor agonists, continuous, personalized monitoring by healthcare professionals ensures early detection of potential adverse effects, such as pancreatic or thyroid abnormalities. Regular blood tests, imaging, and symptom assessments are essential components of a safe long-term treatment plan.
2. The Role of Pharmacogenomics in Tailoring Therapy
Emerging research suggests that genetic profiling can predict individual responses and risks associated with GLP-1 medications, paving the way for precision medicine approaches that optimize benefits while minimizing long-term risks.
3. Combining Pharmacotherapy with Lifestyle Interventions Enhances Sustainability
Integrating diet, exercise, behavioral therapy, and medical supervision creates a synergistic effect, reducing reliance on medication over time and lowering potential long-term health risks.
4. The Need for Ongoing Longitudinal Research
While current short-term data are promising, large-scale, long-term studies are imperative to fully understand the chronic effects of GLP-1 therapies, including potential neoplastic or metabolic alterations that may develop over years.
5. Developing Next-Generation GLP-1 Receptor Agonists
Innovations such as dual agonists targeting multiple pathways may offer enhanced efficacy with fewer long-term safety concerns, representing a promising frontier for personalized, durable metabolic therapies.
Curated Expert Resources
- Journal of Endocrinology & Metabolism: Provides peer-reviewed studies on GLP-1 safety profiles, mechanisms, and clinical outcomes essential for advanced understanding.
- The Lancet Diabetes & Endocrinology: Features comprehensive reviews and the latest research on long-term effects and surveillance strategies for GLP-1 therapies.
- American Diabetes Association (ADA) Guidelines: Offers evidence-based recommendations on safe use, monitoring, and integrating GLP-1 medications into comprehensive care plans.
- ClinicalTrials.gov: Repository of ongoing studies that explore long-term safety, efficacy, and innovative formulations of GLP-1 receptor agonists.
- Pharmacogenomics Journals: Source of cutting-edge research on genetic predictors of drug response, guiding personalized therapy.
Final Expert Perspective
Understanding the long-term safety of GLP-1 medications demands a nuanced, multidisciplinary approach that combines cutting-edge research, personalized medicine, and vigilant clinical practice. As the frontier of metabolic therapeutics advances, embracing these insights ensures that we harness the full potential of GLP-1 receptor agonists responsibly. Your engagement—whether through professional discussion, patient advocacy, or ongoing research contributions—is vital in shaping a future where weight management and diabetes care are both effective and safe for the long haul. For clinicians and researchers aiming to stay at the forefront, continuous education and collaboration are the keys to unlocking these therapies’ lasting benefits.
,

