Unlocking the Science Behind Injection Site Care in Weight Loss Treatments
Injectable weight loss treatments like semaglutide, tirzepatide, and other GLP-1 receptor agonists have revolutionized obesity management, offering effective fat loss through appetite regulation and metabolic enhancement. However, as these therapies become increasingly popular, proper injection site care emerges as a critical pillar for maximizing treatment efficacy and patient comfort. Understanding the nuances of managing injection sites not only prevents common adverse reactions but also fosters adherence to treatment plans essential for sustainable weight loss.
The Subtle Art of Injection Site Selection: More Than Just a Pinprick
Choosing the optimal injection site is a nuanced process influenced by factors such as skin thickness, blood flow, and previous site usage. Common sites include the abdomen, thigh, and upper arm, each offering distinct absorption characteristics. Rotating injection sites systematically reduces risks of lipohypertrophy and localized irritation. Patients should be educated to avoid injecting into scarred or inflamed areas to prevent complications that could compromise drug absorption and effectiveness.
Transforming Post-Injection Care: Practical Steps to Minimize Discomfort and Complications
Proper post-injection care involves immediate and long-term strategies: applying gentle pressure without massaging the site, using cold compresses to mitigate swelling, and maintaining hygiene to prevent infection. Anecdotal evidence from clinical practice highlights cases where patients who diligently followed site care protocols experienced significantly fewer injection-related side effects. Patients should also monitor for unusual symptoms such as persistent redness, swelling, or pain and consult healthcare providers promptly to address concerns early.
How Can Patients Effectively Manage Injection Site Reactions Without Disrupting Their Weight Loss Journey?
Injection site reactions like redness, itching, or mild swelling are common and often transient. Patients can adopt a regimen that includes gentle cleansing with mild soap, applying soothing topical agents recommended by healthcare professionals, and ensuring consistent site rotation. Importantly, maintaining open communication with medical providers allows for timely adjustments to injection techniques or medications if reactions persist. This proactive approach supports uninterrupted treatment, which is crucial for achieving desired weight loss outcomes.
Integrating Expert Knowledge: A Clinician’s Perspective on Injection Site Best Practices
Medical experts emphasize the importance of personalized injection plans tailored to individual patient anatomy and lifestyle. Incorporating clinician-guided fat loss injections with detailed instruction on site care can dramatically improve patient experiences and results. For instance, supervised injectable weight loss programs combine medical oversight with education on managing injection sites, effectively balancing safety and efficacy (source).
Leveraging such specialized guidance helps patients navigate challenges like injection anxiety or site fatigue, fostering sustained adherence. Additionally, emerging research underscores the role of site care in optimizing drug absorption, directly impacting the pharmacodynamics of injectable medications.
Avoiding Common Pitfalls: What Every User Should Know About Injection Site Hygiene
Despite the efficacy of injectable weight loss treatments, improper site care can lead to complications including infections, bruising, and delayed healing. Patients should be wary of common mistakes such as reusing needles, neglecting site rotation, or failing to cleanse the skin adequately before injection. These errors not only hinder therapeutic outcomes but can also diminish trust in the treatment process.
Educating patients on best hygiene practices and encouraging adherence to prescribed techniques can mitigate these risks substantially. For comprehensive guidance on injection safety and side effect avoidance, readers may explore expert resources like this detailed safety guide.
Engage with us below: have you experienced challenges with injection site care during your weight loss journey? Share your insights or questions to help build a supportive community informed by real experience and expert advice.
Personal Lessons in Injection Site Care: My Journey with GLP-1 Medications
When I first started using semaglutide injections, I underestimated how pivotal proper injection site care would be. Initially, I just focused on the medication itself, eager to see the scale move. But soon, I realized that discomfort and minor skin irritation at injection sites could really affect my motivation. After researching and adjusting my routine—rotating sites more diligently, cleaning the area well, and applying ice packs when needed—I noticed a remarkable difference not just in comfort but in how smoothly the medication seemed to work.
Why Does Injection Site Care Impact Medication Effectiveness?
It turns out, the absorption of medications like semaglutide or tirzepatide can vary based on the condition of the injection site. If the skin is inflamed, scarred, or bruised, the medicine might not be absorbed properly, potentially diminishing its appetite-suppressing and metabolic effects. According to a recent publication from the National Center for Biotechnology Information, proper technique and site care are crucial for optimizing drug bioavailability and minimizing side effects.
Adapting Injection Site Care to Fit Your Lifestyle
It’s important to integrate injection site care seamlessly into daily life. For me, setting reminders to rotate injection sites and keeping a small kit with alcohol wipes and cold packs handy made a big difference. I also learned to listen to my body; if an area felt tender or looked red, I avoided it and gave it time to heal. This practice helped prevent lipohypertrophy and kept my skin healthy throughout treatment.
How Do You Personally Manage Injection Site Reactions and Stay Consistent?
Everyone’s experience with injection site reactions varies, so I’d love to hear from you: What strategies have you found effective for managing injection discomfort or irritation? Have you discovered any tricks to stay consistent with your injection schedule despite site challenges? Your insights could really help others navigating similar journeys.
Exploring Advanced Injection Techniques: Insights from Medical Guidance
Working with healthcare providers who specialize in medically supervised weight loss has offered me invaluable advice. They recommended personalized injection plans that consider my skin type, activity level, and even clothing preferences to minimize irritation and maximize absorption. Programs like medically supervised weight loss injection plans can be game changers, providing tailored guidance and ongoing support.
These expert-led approaches reduce anxiety around injections and encourage adherence, critical for long-term success. They also emphasize the importance of monitoring injection sites regularly and adjusting techniques as needed—a dynamic process rather than a one-size-fits-all routine.
Practical Tips for Maintaining Injection Site Health
From my experience and expert advice, here are some practical tips to keep your injection sites happy and healthy:
- Rotate sites systematically: Follow a rotation schedule to avoid repeatedly using the same spot.
- Cleanse the skin properly: Use mild soap and alcohol wipes before injections.
- Avoid massaging post-injection: Instead, apply gentle pressure if necessary.
- Use cold compresses: Helps reduce swelling and discomfort.
- Stay hydrated and nourish your skin: Healthy skin promotes better healing.
For a deeper dive into these practices, you might find the physician-guided fat loss injection prep tips particularly helpful.
Decoding the Immunological Impact of Repeated Injection Sites on Skin Integrity
Repeated injections at the same anatomical location can provoke complex immunological responses beyond mere mechanical irritation. Chronic local exposure to injectable agents may incite a cascade of inflammatory mediators, altering the skin’s microenvironment. This can lead to fibroblast activation and collagen remodeling, culminating in lipodystrophy or even granulomatous reactions in rare cases. Understanding these immunopathological mechanisms is essential for clinicians aiming to optimize injection protocols that preserve skin integrity while ensuring maximal pharmacodynamic effect.
Advanced dermatological assessments often reveal subclinical changes in skin elasticity and microvasculature post repeated administration, which may not be immediately apparent to patients. Therefore, integrating periodic skin evaluations using non-invasive imaging modalities such as high-frequency ultrasound or dermoscopy can offer invaluable insights into early tissue alterations, allowing timely intervention.
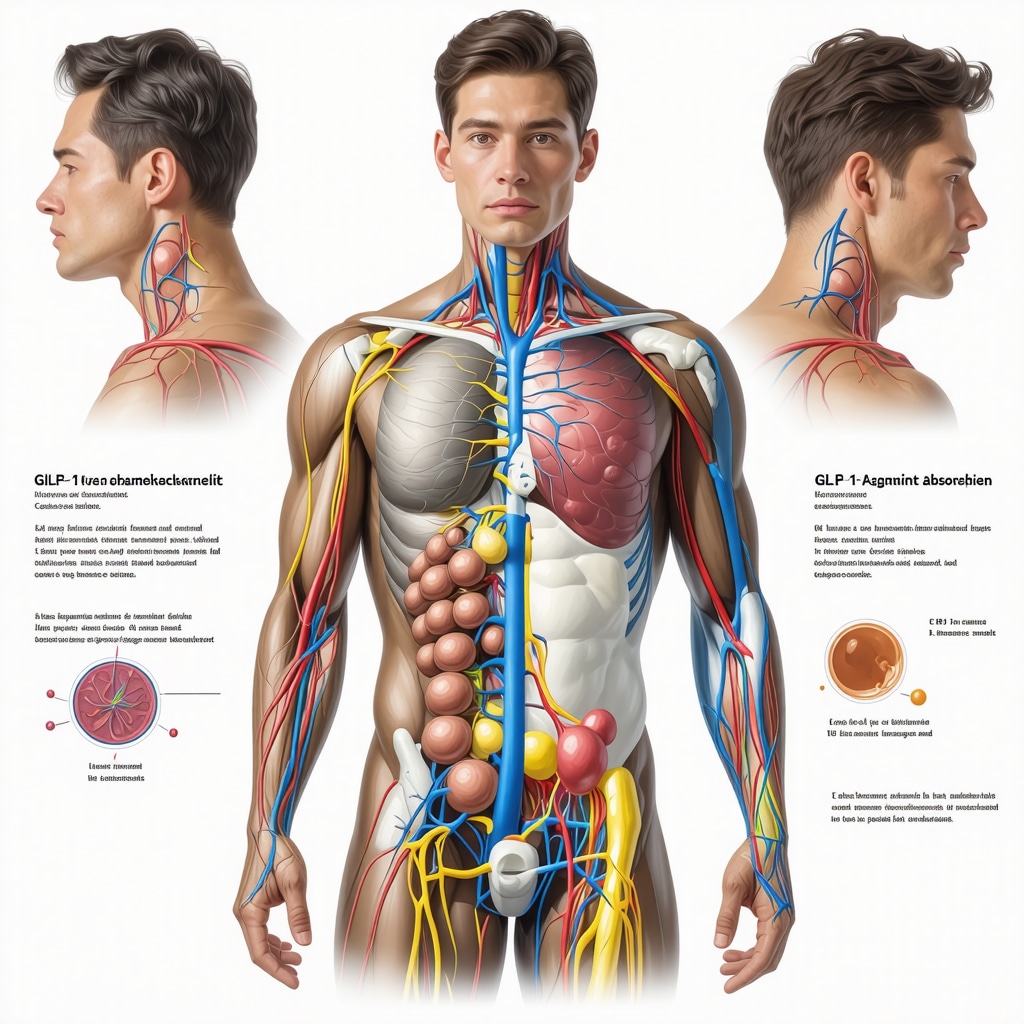
Leveraging Pharmacokinetics: How Injection Site Variability Influences GLP-1 Agonist Absorption Dynamics
The pharmacokinetic profile of GLP-1 receptor agonists like semaglutide is intricately linked to the vascularization of the injection site. Varying capillary density and interstitial fluid dynamics across injection locations modulate the absorption rate and bioavailability of these agents. For example, abdominal subcutaneous tissue generally facilitates faster absorption compared to the thigh due to richer vascular supply, potentially influencing onset of action and peak plasma concentrations.
Clinicians must weigh these factors when advising patients, particularly those with comorbid conditions affecting peripheral circulation such as diabetes mellitus or peripheral artery disease. Tailoring injection site recommendations to individual vascular health profiles could mitigate variability in therapeutic responses, enhancing overall treatment consistency.
What Are the Best Evidence-Based Practices for Preventing Lipohypertrophy in Long-Term Injectable Weight Loss Therapy?
Lipohypertrophy, characterized by localized adipose tissue hypertrophy, is a prevalent complication of chronic injection therapy. High-quality studies emphasize the importance of systematic site rotation combined with patient education on injection technique precision. Specifically, spacing injections at least 2 cm apart within a given site and avoiding needle reuse significantly reduce tissue hypertrophy incidence.
Moreover, emerging interventions include the use of shorter, finer-gauge needles and rotating between multiple anatomical sites to distribute subcutaneous trauma evenly. Regular clinical assessments to detect early lipohypertrophic changes enable timely modification of injection practices. These strategies are corroborated by guidelines published in the Journal of Diabetes Research, which provide comprehensive protocols validated across diverse patient populations.
Integrating Technology: Digital Tools and Apps for Monitoring Injection Site Health and Compliance
Advancements in digital health have paved the way for innovative solutions that empower patients in managing injection site care. Mobile applications equipped with reminders for site rotation, symptom tracking logs, and educational modules facilitate adherence and early recognition of adverse site reactions. Such platforms often incorporate image capture functionalities allowing remote clinician review, thereby bridging gaps in follow-up and personalized feedback.
Data analytics derived from these apps can identify patterns correlating injection practices with outcomes, enabling dynamic adjustments in treatment plans. Patients report higher engagement and reduced anxiety when leveraging technology-assisted management, suggesting a critical role for digital interventions in enhancing long-term success of injectable weight loss therapies.
Advanced Training for Healthcare Providers: Elevating Injection Technique Expertise
Ensuring optimal injection site care extends beyond patient education; it mandates that healthcare providers remain at the forefront of technique refinement. Specialized training programs focusing on anatomical landmarks, needle selection, and site rotation strategies can markedly improve patient outcomes. Simulation-based learning and competency assessments reinforce best practices, minimizing procedural errors that could compromise drug delivery efficacy.
Interdisciplinary collaboration between endocrinologists, dermatologists, and nurse educators fosters a holistic approach to injection site management. This synergy promotes not only technical excellence but also empathetic communication addressing patient concerns and barriers to adherence.
For practitioners seeking to deepen their expertise, the American Association of Clinical Endocrinology Weight Management Education offers advanced modules on injectable therapies and site care protocols.
Engage with our community forum to share your clinical experiences or innovations in injection site care—together, we can elevate standards and outcomes in injectable weight loss treatment.
Harnessing Immunomodulatory Insights to Preserve Skin Health in Chronic Injectable Therapy
Beyond basic care, understanding the immunological ramifications of repeated injections unveils a sophisticated layer of skin management. Chronic exposure to injectable weight loss agents can trigger localized immune responses, including activation of inflammatory cytokines and remodeling of dermal extracellular matrix components. These effects may silently compromise the skin’s barrier function and elasticity, underscoring the need for clinicians to incorporate immunopathological considerations into patient guidance.
Advanced diagnostic tools such as high-frequency ultrasonography and confocal microscopy have emerged as invaluable for detecting early subclinical changes, enabling proactive modification of injection techniques or site rotation schedules before overt complications manifest.
Pharmacokinetic Nuances: Tailoring Injection Sites to Maximize GLP-1 Receptor Agonist Absorption
The vascular heterogeneity among injection sites significantly influences the pharmacokinetics of GLP-1 receptor agonists. For instance, abdominal injections benefit from richer capillary networks, facilitating more rapid and consistent drug uptake compared to the thigh or upper arm. Patients with vascular comorbidities require tailored site recommendations to mitigate absorption variability, ensuring steady therapeutic plasma levels and optimal metabolic effects.
What Are the Best Evidence-Based Practices for Preventing Lipohypertrophy in Long-Term Injectable Weight Loss Therapy?
Preventing lipohypertrophy necessitates a multifaceted approach emphasizing systematic site rotation, precise needle placement, and patient education on injection techniques. Utilizing shorter, finer-gauge needles and spacing injections at least 2 cm apart within a given anatomical area reduces adipose tissue hypertrophy risk. Regular clinical monitoring for early detection combined with patient adherence to hygiene and technique protocols is paramount. These recommendations are substantiated by comprehensive guidelines published in the Journal of Diabetes Research, which delineate validated prevention strategies applicable across diverse populations.
Digital Innovations: Harnessing Technology to Elevate Injection Site Management and Treatment Adherence
Emerging digital health platforms empower patients through interactive tools that facilitate injection site rotation reminders, symptom tracking, and photographic documentation for remote clinician evaluation. These apps leverage data analytics to identify behavioral patterns and injection site issues early, facilitating personalized interventions. Such technology-enhanced management fosters patient engagement, reduces anxiety around injections, and supports sustained adherence—critical determinants of long-term success in injectable weight loss therapies.
Specialized Training for Healthcare Providers: Advancing Injection Technique Mastery and Patient Outcomes
Healthcare professionals play an instrumental role in optimizing injection site care through ongoing skill enhancement. Advanced training programs focusing on anatomical precision, needle selection, and empathetic patient communication reinforce best practices and minimize procedural errors. Collaboration among endocrinologists, dermatologists, and nurse educators cultivates a comprehensive care model that addresses both technical and psychosocial facets of injectable weight loss management.
Providers seeking to elevate their expertise can access cutting-edge educational resources such as the American Association of Clinical Endocrinology Weight Management Education, which offers specialized modules on injection protocols and site care strategies.
Engage with our expert community forum to exchange insights, clinical experiences, and innovations driving excellence in injection site care and patient adherence to injectable weight loss regimens.
Frequently Asked Questions (FAQ)
Why is rotating injection sites important in injectable weight loss therapies?
Rotating injection sites is crucial to prevent localized complications such as lipohypertrophy, scar tissue formation, and skin irritation. Systematic rotation allows tissue recovery, maintains consistent drug absorption rates, and reduces discomfort, thereby improving treatment adherence and efficacy.
Which injection sites offer the best absorption for GLP-1 receptor agonists like semaglutide?
The abdomen generally provides the richest vascularization and thus faster absorption compared to the thigh or upper arm. However, individual vascular health and tissue characteristics can influence this, so site selection should be personalized in consultation with healthcare providers.
How can patients manage common injection site reactions without interrupting their weight loss regimen?
Mild reactions such as redness, itching, or swelling can be managed with proper hygiene, gentle cleansing, applying cold compresses, and avoiding massaging the site post-injection. Persistent or severe symptoms warrant prompt medical evaluation to adjust treatment if necessary.
What steps can prevent lipohypertrophy during long-term injectable therapy?
Prevention includes consistent rotation of injection sites, spacing injections at least 2 cm apart within the same area, using appropriate needle sizes, and avoiding needle reuse. Regular skin assessments by clinicians help detect early tissue changes for timely intervention.
Are there technological tools that help improve injection site care and adherence?
Yes, digital health applications provide reminders for site rotation, allow symptom tracking, and enable photographic documentation for remote clinical review. These tools enhance patient engagement, facilitate early detection of complications, and support sustained compliance.
How do immunological responses affect skin integrity with repeated injections?
Repeated injections can induce local immune activation, inflammation, and remodeling of the dermal extracellular matrix. These changes may reduce skin elasticity and barrier function over time, emphasizing the need for careful site management and periodic clinical monitoring using advanced imaging techniques.
What role do healthcare providers play in optimizing injection site care?
Providers deliver essential education on technique, site selection, and hygiene, conduct clinical assessments, and tailor injection plans to patient needs. Specialized training enhances their ability to minimize complications and improve patient comfort and outcomes.
Can lifestyle factors influence injection site health?
Absolutely. Hydration, skin nutrition, avoiding trauma or irritation, and appropriate clothing choices can all contribute to healthier skin and better injection site outcomes. Patients should integrate these considerations into their routine alongside medical guidance.
Is it possible for injection site condition to impact the pharmacodynamics of weight loss medications?
Yes, compromised injection sites with inflammation, scarring, or lipohypertrophy can impair drug absorption and bioavailability, potentially reducing the medication’s appetite-suppressing and metabolic effects.
How can patients self-monitor injection sites effectively?
Patients should routinely inspect sites for redness, swelling, lumps, or unusual changes. Using mirror checks, photographic records via apps, and communicating any concerns promptly with healthcare providers enables early management of issues.
Trusted External Sources
- National Center for Biotechnology Information (NCBI): Offers peer-reviewed research articles detailing pharmacokinetics, immunological effects, and clinical guidelines on injection site care for GLP-1 receptor agonists.
- Journal of Diabetes Research: Provides evidence-based protocols for preventing injection-related complications like lipohypertrophy, critical for long-term injectable therapy success.
- American Association of Clinical Endocrinology (AACE): Publishes advanced educational resources and CME modules focused on weight management and injectable therapy best practices for healthcare professionals.
- Clinical Dermatology Journals: Deliver insights into skin immunopathology and advanced imaging techniques relevant to chronic injection site management.
- Specialized Digital Health Platforms: Emerging technology developers that offer validated apps for monitoring injection sites and supporting patient adherence in injectable weight loss treatments.
Conclusion: Mastering Injection Site Care for Optimal Weight Loss Outcomes
Injection site care is a fundamental yet often underestimated component of effective injectable weight loss therapies such as semaglutide and tirzepatide. Through meticulous site rotation, hygiene, and patient education, alongside leveraging digital tools and expert clinical guidance, patients can minimize adverse reactions, preserve skin integrity, and ensure consistent medication absorption. Healthcare providers play a pivotal role by delivering personalized injection plans and advanced training to optimize outcomes. Understanding the immunological and pharmacokinetic nuances of injection sites further refines these strategies, fostering sustained adherence and maximizing therapeutic benefits. Embrace these expert-informed practices and share your experiences or questions to contribute to a knowledgeable, supportive community dedicated to successful weight loss journeys.


Injectable weight loss treatments like semaglutide and tirzepatide have really changed the game for managing obesity, but what often gets overlooked is how crucial injection site care is to the whole process. After reading this comprehensive post, I’m struck by how much injection site condition directly affects medication absorption and overall effectiveness. It’s not just about taking the medication; it’s about optimizing the site health to get the best results. In my experience, rotating injection sites systematically made a huge difference—not only did it prevent annoying lumps or skin irritation, but I also felt the treatments worked more consistently. I also appreciate the emphasis on avoiding massaging after injections, as I used to think rubbing the area would help. It’s fascinating to learn about the immunological changes that can happen with repeated injections in the same spot and how technology like apps and imaging might help monitor these early. For those managing their injections daily, how have you integrated site care into your routine without making it feel like an extra chore? And for healthcare providers out there, what are some effective ways to educate and encourage patients to maintain these best practices consistently?
Madeline, I completely resonate with your point about the importance of injection site care in maximizing the effectiveness of treatments like semaglutide and tirzepatide. From my personal experience, integrating site care into my daily routine became manageable by treating it like a small self-care ritual rather than a chore. I keep a dedicated, portable kit with alcohol swabs, cold packs, and a site rotation chart. Setting reminders on my phone not only helps with timing but also prompts me to switch sites systematically. This approach has significantly reduced discomfort and skin irritation for me.
As for educating patients, I believe healthcare providers can enhance adherence by combining clear, personalized instructions with demonstrations during appointments. Visual aids like rotation grids and video tutorials can clarify proper techniques. Moreover, encouraging patients to use digital apps that track injection sites and symptoms can foster engagement and make adherence feel more like a streamlined habit than additional work.
How do others find digital tools impact their comfort and consistency with site care? Are there specific apps or strategies you’ve found particularly supportive? It would be helpful to share recommendations to aid those navigating this critical aspect of injectable weight loss therapy.
Madeline and Eleanor have touched on some great points about the significance of injection site care, especially the importance of systematic site rotation and integrating it as a manageable routine. From my perspective, one challenge that often goes under-discussed is how individual anatomical differences really impact site selection and absorption. For example, I found that injecting in the abdomen works well generally, but during periods of intense exercise or different hydration levels, absorption rates seemed to vary noticeably. This made me ponder if there’s a need for more dynamic site rotation strategies—perhaps factoring in daily activity or skin sensitivity rather than just fixed rotation schedules.
Moreover, I’ve found that partnering closely with my healthcare provider to personalize injection plans, considering my skin type, circulation issues, and lifestyle helped me preempt irritation and optimize absorption. As digital tools continue to evolve, I’m curious if integrating wearable tech that monitors skin condition or blood flow around injection sites could eventually tailor injection timing and location dynamically.
Has anyone else noticed such variability in absorption with lifestyle factors, and how do you adjust your injection site care accordingly? Also, for healthcare practitioners, do you see a future where personalized site rotation could become more real-time and data-informed, rather than based solely on patient recollection or manual logs?
Logan brings up a fascinating point about how lifestyle factors like exercise intensity and hydration levels can influence the absorption of injectable weight loss medications. I’ve also experienced this variability firsthand. Some days, after a vigorous workout, I noticed that injections felt a little more uncomfortable, and I’ve wondered if blood flow changes in the area could affect how quickly or effectively the medication is absorbed. Adjusting my injection sites to less exercised areas during those days seemed to help reduce discomfort and possibly improve effectiveness.
I’m really intrigued by the idea of leveraging wearable technology or real-time monitoring tools to guide site rotation and injection timing, as it could personalize treatment far beyond the current fixed rotation schedules. This would be especially useful for those with underlying vascular issues or sensitive skin.
Another aspect I pay attention to is environmental temperature and skin hydration; I make sure to moisturize well on non-injection days and avoid injecting into extremely dry or overly warm skin to prevent irritation.
For others managing these fluctuations, how do you decide when to alter your injection site based on your daily activities or skin condition? Have any healthcare professionals recommended real-time adjustments, or is it mostly left to patient intuition? It would be great to hear real-world strategies for navigating these nuances while maintaining consistent therapy.
Reading this post really made me realize how much thought needs to go into injection site care, beyond just administering the medication. I’ve experienced some minor skin irritation and noticing the benefits of consistent site rotation, but implementing it into a busy daily routine can be challenging. Personally, I’ve started keeping a small chart and setting daily reminders to rotate sites, which helps keep everything systematic without feeling overwhelming. I also find that maintaining good skin hydration and avoiding areas that are red or sensitive makes a difference in reducing irritation. It’s interesting how the immune response can subtly alter skin health over time, making regular evaluation important. Do others find that timing injections around physical activity helps improve comfort and absorption? Additionally, are there digital tools or apps that you’ve found effective for tracking site health and rotation? Sharing these practical tips can make the routine more manageable and enhance treatment outcomes.
Building on the insightful discussion about the critical role of injection site care in optimizing injectable weight loss treatments, I want to highlight the often-overlooked importance of patient empowerment through education. From my personal journey with GLP-1 receptor agonists, I noticed that initial skin irritation and discomfort were discouraging until my healthcare provider involved me deeper in the treatment process. By understanding the science behind site fatigue and immunological responses from repeated injections, I felt more motivated to adhere to rotation schedules and hygiene protocols.
I also experimented with combining site rotation with lifestyle patterns—for example, avoiding injecting on areas subjected to heavy exercise that day to reduce discomfort and ensure better absorption. This mindful approach felt more natural and sustainable. Moreover, while digital apps are recommended, I found that pairing technology with clear, visual rotation charts and regular check-ins with my provider keeps me accountable and proactive.
I’m curious—how have others balanced the demands of thorough injection site care with day-to-day activities without feeling overwhelmed? Also, for clinicians, what strategies have you found most effective in bridging the gap between patient knowledge and actionable adherence? Sharing these experiences can really build a strong community that supports better outcomes for everyone using injectable weight loss therapies.