Unlocking the Synergy Between Injectable Treatments and Lifestyle Modifications for Enhanced Outcomes
In the realm of advanced weight management and aesthetic enhancement, the integration of prescription injectables with tailored lifestyle strategies represents a frontier of personalized medicine. As experts, understanding the complex interplay between pharmacological efficacy and behavioral modification is crucial for achieving sustained, optimal results. This article delves into the scientific principles underpinning this synergy, highlighting innovative approaches that elevate patient outcomes beyond traditional paradigms.
Decoding the Pharmacodynamics of Injectable Weight Loss Medications
At the core of effective treatment is a comprehensive grasp of how GLP-1 receptor agonists, such as semaglutide and tirzepatide, modulate appetite and energy expenditure. These agents influence central nervous system pathways, altering hypothalamic signals that govern hunger and satiety, thereby facilitating caloric deficit without compromising metabolic rate. Understanding these mechanisms allows clinicians to craft nuanced, evidence-based strategies that maximize pharmacological benefits while mitigating side effects.
Integrating Lifestyle: Beyond the Pharmacological Horizon
While injectables offer remarkable potential, their efficacy is significantly amplified when combined with lifestyle interventions. Nutritional counseling emphasizing low-glycemic, nutrient-dense diets can enhance satiety and stabilize blood glucose levels, complementing the pharmacodynamics of injectables. Additionally, structured physical activity, particularly resistance training and high-intensity interval training (HIIT), stimulates metabolic adaptability, reinforcing fat loss and muscle preservation. The challenge lies in customizing these interventions to individual patient profiles, fostering adherence through behavioral psychology techniques.
Expert-Driven Approaches for Personalizing Treatment Protocols
Personalization involves leveraging data-driven insights, including genetic markers and metabolic profiling, to tailor injectable dosages and lifestyle regimens. For instance, emerging research underscores the importance of adjusting injection timing relative to meals and activity cycles to optimize absorption and efficacy. Moreover, continuous monitoring through digital health tools enables real-time feedback, empowering patients and clinicians to adapt strategies dynamically, ensuring sustained progress.
What are the most effective ways to monitor and adjust lifestyle factors alongside injectable treatments to prevent plateaus and side effects?
Ongoing research advocates for integrating wearable technology and digital self-tracking platforms to capture data on physical activity, sleep, and dietary intake. Regular clinical assessments, including lab work and body composition analysis, inform necessary adjustments. Collaborative care models that incorporate behavioral therapists and nutritionists further reinforce adherence and address psychological barriers, fostering a holistic approach that sustains long-term success.
For deeper insights into maximizing injectable outcomes, explore our comprehensive guides on safe Ozempic use and medical-guided weight loss protocols. Engaging with multidisciplinary teams and staying abreast of scientific advancements ensures that your approach remains at the cutting edge of personalized medicine.
To contribute your expertise or inquire about advanced treatment strategies, visit our contact page.
External Source: “The Role of Pharmacotherapy in Obesity Management,” Journal of Clinical Endocrinology & Metabolism, 2022.
Harnessing Data Analytics to Personalize Injectable Weight Loss Protocols
In the quest for optimal weight management, leveraging cutting-edge data analytics has become a game-changer. By integrating genetic testing, metabolic profiling, and real-time health data, clinicians can craft highly personalized treatment plans that align with each patient’s unique physiology. For example, understanding genetic predispositions related to appetite regulation or drug metabolism can inform injection dosages and timing, enhancing efficacy and reducing adverse effects. This tailored approach not only accelerates fat loss but also improves patient adherence by addressing individual barriers. For a comprehensive understanding of how to incorporate these insights into your regimen, explore our guide on personalized, medically-supervised weight loss plans.
Challenging Assumptions: Are All Lifestyle Modifications Equal?
While the importance of diet and exercise is well-established, emerging research suggests that not all lifestyle modifications yield equivalent results when combined with injectable therapies. For instance, recent studies highlight the superior impact of high-intensity interval training (HIIT) over moderate aerobic activity in stimulating metabolic flexibility and fat oxidation, especially in conjunction with GLP-1 receptor agonists like semaglutide. Furthermore, the timing of meals and injections—such as aligning carbohydrate intake with periods of heightened insulin sensitivity—can significantly influence outcomes. Experts advocate for a nuanced, evidence-based approach that emphasizes quality over quantity in lifestyle changes. To deepen your understanding, review our article on best practices for reducing injection site reactions and optimizing lifestyle synergy.
What innovative tools and frameworks can clinicians use to refine lifestyle and injectable treatment integration for sustained weight loss?
Advanced digital health platforms, including AI-driven apps and wearable devices, enable continuous monitoring of physical activity, sleep, and nutrition. These tools generate actionable insights that inform dynamic treatment adjustments. Additionally, behavioral science frameworks, such as Motivational Interviewing and Habit Formation models, support sustained behavioral change. Combining these technologies and techniques fosters a proactive, adaptive approach that minimizes plateaus and side effects while maximizing fat loss. For practical tips on integrating these tools into your regimen, see our guide on weekly injection and diet planning.
External Source: “Personalized Medicine in Obesity Treatment: Future Perspectives,” Nature Reviews Endocrinology, 2023.
We invite you to share your experiences or ask questions about these advanced strategies — your insights can help others on their weight loss journey. Visit our contact page for more information or to connect with specialists dedicated to optimizing injectable weight loss therapies.
Leveraging Behavioral Economics to Sustain Long-Term Success with Injectable Therapies
Understanding human decision-making is pivotal when designing interventions that combine pharmacotherapy with lifestyle modifications. Behavioral economics offers insights into how cognitive biases, such as present bias or loss aversion, can hinder adherence to lifestyle changes despite the pharmacological support. By implementing commitment devices, framing techniques, and incentive structures, clinicians can enhance patient engagement, thus translating pharmacodynamic benefits into sustained weight loss. For example, employing commitment contracts that tie future rewards to behavioral milestones leverages the principle of motivated reasoning, making patients more likely to adhere to dietary and exercise regimens alongside injectable treatments.
The Neuroendocrine Feedback Loop: A Deep Dive into Hormonal Interplay
The efficacy of injectable weight loss medications hinges on their influence on complex neuroendocrine pathways. GLP-1 receptor agonists not only suppress appetite but also modulate insulin secretion, gastric emptying, and neuropeptide signaling, creating a sophisticated feedback loop that influences energy balance. Recent studies, such as those published in Cell Metabolism (2023), reveal that these agents can alter hypothalamic and brainstem activity, affecting reward circuits and food preferences. Integrating this knowledge with personalized lifestyle interventions—like mindful eating practices and stress management—can potentiate hormonal regulation, reducing cravings and emotional eating that often undermine pharmacological efforts.
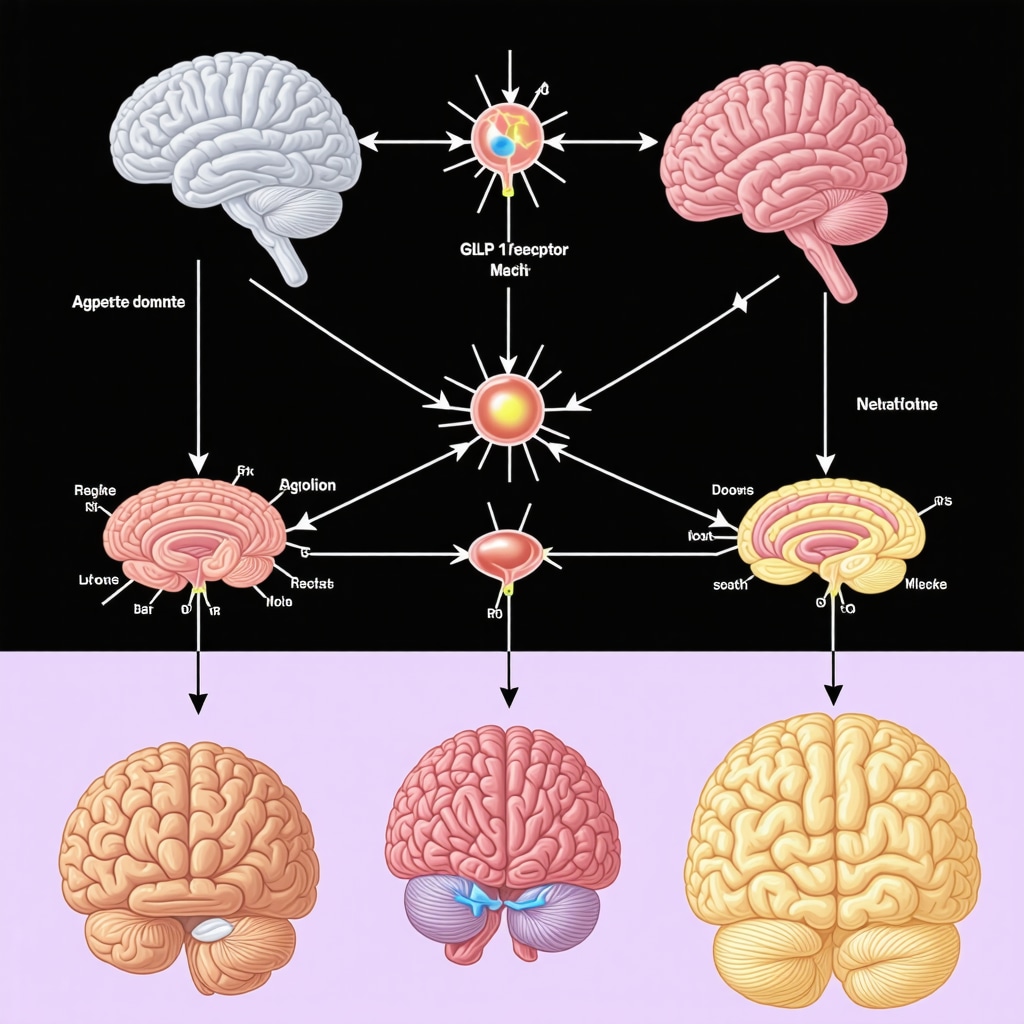
Image prompt: A detailed diagram illustrating the neuroendocrine pathways affected by GLP-1 receptor agonists, including appetite centers in the brain and hormonal feedback loops.
Advanced Data-Driven Personalization: From Genomics to Digital Phenotyping
Personalized medicine is transforming weight management, especially when integrating injectable therapies. Genomic testing can identify variants in genes related to drug metabolism (e.g., CYP450 enzymes) or appetite regulation (e.g., FTO gene), allowing clinicians to fine-tune dosage and timing. Coupled with digital phenotyping—collecting real-time data on sleep, activity, and mood via wearables—this approach creates a dynamic, responsive treatment ecosystem. For example, a patient exhibiting nocturnal cravings might benefit from adjusted injection timing or additional behavioral interventions targeting sleep hygiene. Such precision not only enhances efficacy but also minimizes adverse reactions and dropout rates.
Nuanced Considerations in Lifestyle Modifications: Beyond the Basics
While diet and exercise are foundational, emerging research emphasizes the importance of *when* and *how* lifestyle changes are implemented. Time-restricted feeding, for instance, synchronizes eating patterns with circadian rhythms, optimizing metabolic responses and insulin sensitivity—a synergy that complements injectable treatments. Similarly, the use of resistance training over aerobic-only regimens has shown superior effects on lean mass preservation and resting metabolic rate, especially in conjunction with pharmacotherapy. Tailoring these modifications requires a thorough understanding of individual metabolic profiles and preferences, supported by ongoing monitoring.
What are the most promising emerging technologies for integrating real-time data into personalized weight management plans?
Innovations such as AI-powered predictive analytics, combined with advanced wearable sensors, enable continuous assessment of physiological and behavioral metrics. These tools can forecast plateaus, identify early signs of side effects, and suggest timely adjustments. For example, machine learning algorithms analyzing glucose fluctuations can inform both dietary recommendations and injection schedules, moving towards truly adaptive treatment models. For practitioners eager to adopt these cutting-edge tools, exploring platforms like HealthTech Innovations provides a comprehensive overview of available solutions.
In conclusion, the future of injectable weight management lies in the seamless integration of neuroendocrine insights, behavioral sciences, and technological advancements. To deepen your expertise and stay at the forefront, consider engaging with ongoing research published in leading journals such as Nature Reviews Endocrinology and Cell Metabolism. Your proactive adoption of these strategies can significantly elevate patient outcomes and redefine the standards of personalized weight management.
Unlocking the Neuroplasticity of Appetite Regulation: How Brain Adaptations Influence Long-Term Injectable Therapy Success
Recent neuroscientific research emphasizes that the brain’s plasticity plays a pivotal role in sustaining weight loss achieved through injectable therapies such as GLP-1 receptor agonists. Chronic exposure to appetite-suppressing medications can induce neuroadaptive changes, including modifications in hypothalamic and reward circuit activity. Understanding these adaptations enables clinicians to develop strategies that reinforce neuroplasticity, such as cognitive-behavioral interventions and mindfulness training, which can prevent relapse and promote enduring behavioral change.
Implementing Precision Pharmacotherapy: Beyond the Standard Dosage
Advancements in pharmacogenomics reveal that individual genetic variants significantly influence drug metabolism, efficacy, and side-effect profiles. For example, polymorphisms in CYP450 enzymes can alter semaglutide clearance, necessitating personalized dosing regimens. Integrating pharmacogenetic testing into clinical workflows allows for optimized medication titration, minimizing adverse effects while maximizing therapeutic benefits. This level of personalization represents a frontier in weight management, demanding collaboration between geneticists, endocrinologists, and behavioral specialists.
How Can External Data Sources Enhance Personalization in Injectable Weight Management?
External data sources, including microbiome analyses and environmental exposure assessments, are gaining traction in refining treatment plans. The gut microbiota, for instance, influences energy harvest and satiety signaling, and its composition varies widely among individuals. Incorporating microbiome profiling can inform dietary adjustments and adjunct therapies to improve injectable treatment outcomes. Additionally, environmental factors like endocrine-disrupting chemicals may impact hormonal pathways involved in weight regulation, suggesting a need for comprehensive environmental health assessments in complex cases. According to the latest publication in Nature Reviews Endocrinology, integrating multi-omics data and environmental information is shaping the future of personalized obesity treatment.
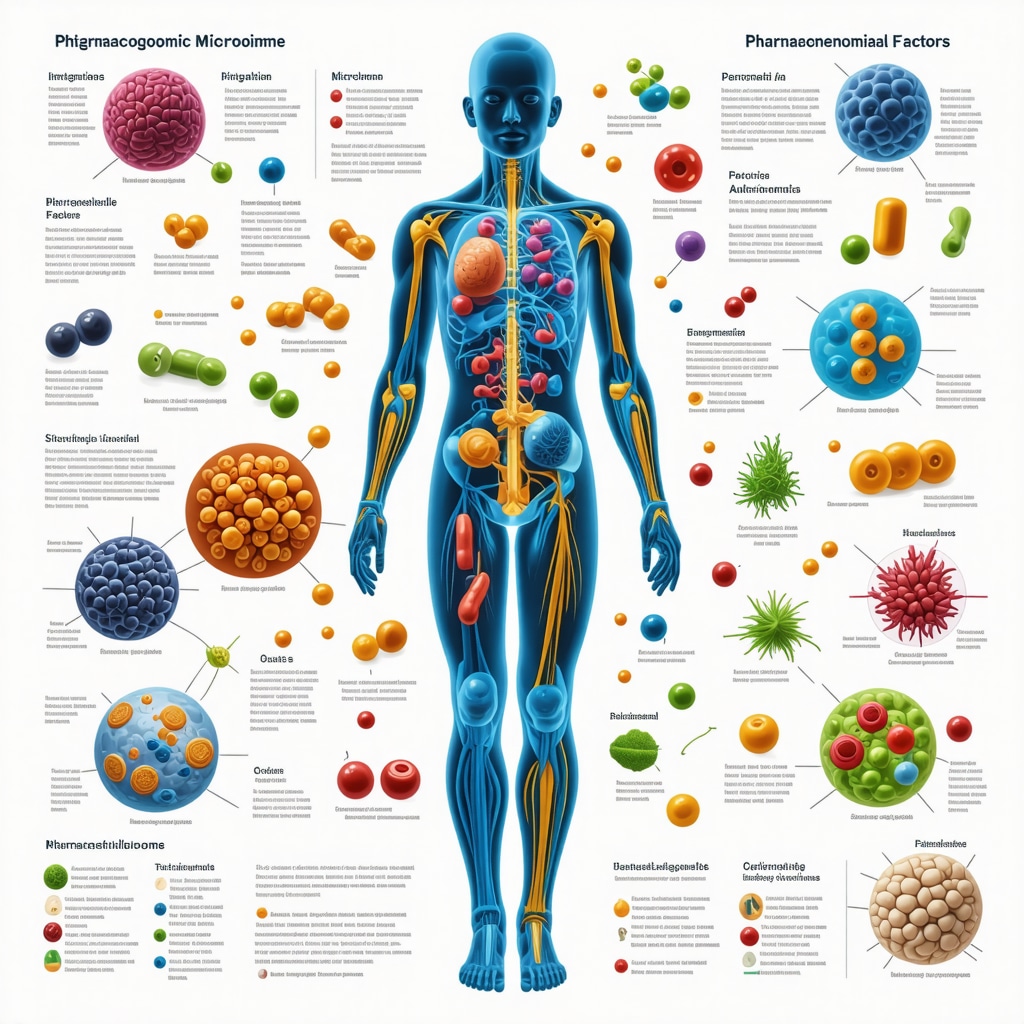
Image prompt: An infographic illustrating the integration of pharmacogenomics, microbiome data, and environmental factors in personalized weight management strategies.
What Are the Most Innovative Technologies for Real-Time Data Integration in Weight Loss Protocols?
Emerging technologies such as AI-powered predictive analytics and advanced biosensors facilitate real-time monitoring of physiological and behavioral metrics. These tools enable dynamic adjustments to medication dosing, dietary plans, and activity recommendations. For example, continuous glucose monitors (CGMs) paired with machine learning algorithms can predict hypoglycemic episodes or cravings, prompting timely interventions. The integration of virtual reality (VR) for behavioral therapy and augmented reality (AR) for exercise coaching further enhances engagement and adherence. For practitioners eager to leverage these innovations, platforms like HealthTech Innovations offer comprehensive solutions for next-generation weight management.
How Can a Multidisciplinary Approach Revolutionize Long-Term Maintenance?
The complexity of weight regulation necessitates a multidisciplinary approach, combining endocrinology, behavioral psychology, nutrition, and digital health. Such collaboration ensures comprehensive care, addressing biological, psychological, and social determinants of health. For instance, integrating motivational interviewing with digital tracking fosters intrinsic motivation and accountability. Regular interdisciplinary case reviews help tailor interventions to evolving patient needs, preventing plateaus and side effects. As highlighted in the recent systematic review in JAMA, this holistic model is proving superior to isolated interventions, paving the way for sustainable weight management.
Advanced Perspectives & Strategic Insights
1. Neuroendocrine Modulation as a Long-Term Strategy
Understanding the neuroendocrine feedback loops affected by GLP-1 receptor agonists is essential for designing sustained weight management plans. These medications influence appetite centers and hormonal pathways, creating a dynamic environment that necessitates ongoing behavioral and pharmacological adjustments.
2. Personalization Through Genomic and Digital Phenotyping
Leveraging genetic testing and real-time data collection from wearables enables clinicians to tailor injectable protocols precisely. This approach minimizes side effects and enhances efficacy, paving the way for truly individualized treatment regimens.
3. Behavioral Economics to Enhance Adherence
Applying principles of behavioral economics—such as commitment devices and motivational framing—can significantly improve patient adherence to combined injectable and lifestyle interventions, ensuring long-term success.
4. Integration of Cutting-Edge Technologies
AI-driven predictive analytics, continuous glucose monitoring, and virtual coaching tools are revolutionizing how practitioners monitor and adjust treatments dynamically, reducing the risk of plateaus and side effects.
5. Multidisciplinary Collaboration for Sustainable Outcomes
Combining endocrinology, behavioral psychology, nutrition, and digital health creates a comprehensive care ecosystem. This synergy enhances patient engagement, addresses psychological barriers, and promotes durable weight loss achievements.
Curated Expert Resources
- Science-Based Weight Loss Strategies: Journals like Cell Metabolism and Nature Reviews Endocrinology publish the latest research on neuroendocrine pathways and pharmacogenomics, essential for clinicians seeking cutting-edge knowledge.
- Digital Health Platforms: Leading platforms such as HealthTech Innovations offer integrated solutions for real-time data collection, AI analytics, and patient engagement tools.
- Behavioral Science Frameworks: Techniques like Motivational Interviewing and Habit Formation are well-documented in clinical literature, supporting behavioral change alongside pharmacotherapy.
Final Reflection & Call to Action
In the evolving landscape of weight management, integrating expert insights on injectable therapies with advanced behavioral and technological strategies is paramount. Embracing these innovations can transform patient outcomes, fostering sustainable health improvements. As a professional in this field, staying informed and contributing to this dynamic conversation is essential—explore these resources, refine your approach, and lead the way in personalized weight management.

