Revolutionizing Weight Management: The Role of GLP-1 Injection Frequency
Glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as a transformative class of injectable medications, primarily used to aid weight loss and improve metabolic health. The therapeutic efficacy of these agents hinges not only on their pharmacological properties but also significantly on how often the injections are administered. Understanding the nuanced benefits of injection frequency offers patients and clinicians alike a strategic advantage in optimizing treatment outcomes.
Precision in Practice: Why Injection Frequency Matters More Than You Think
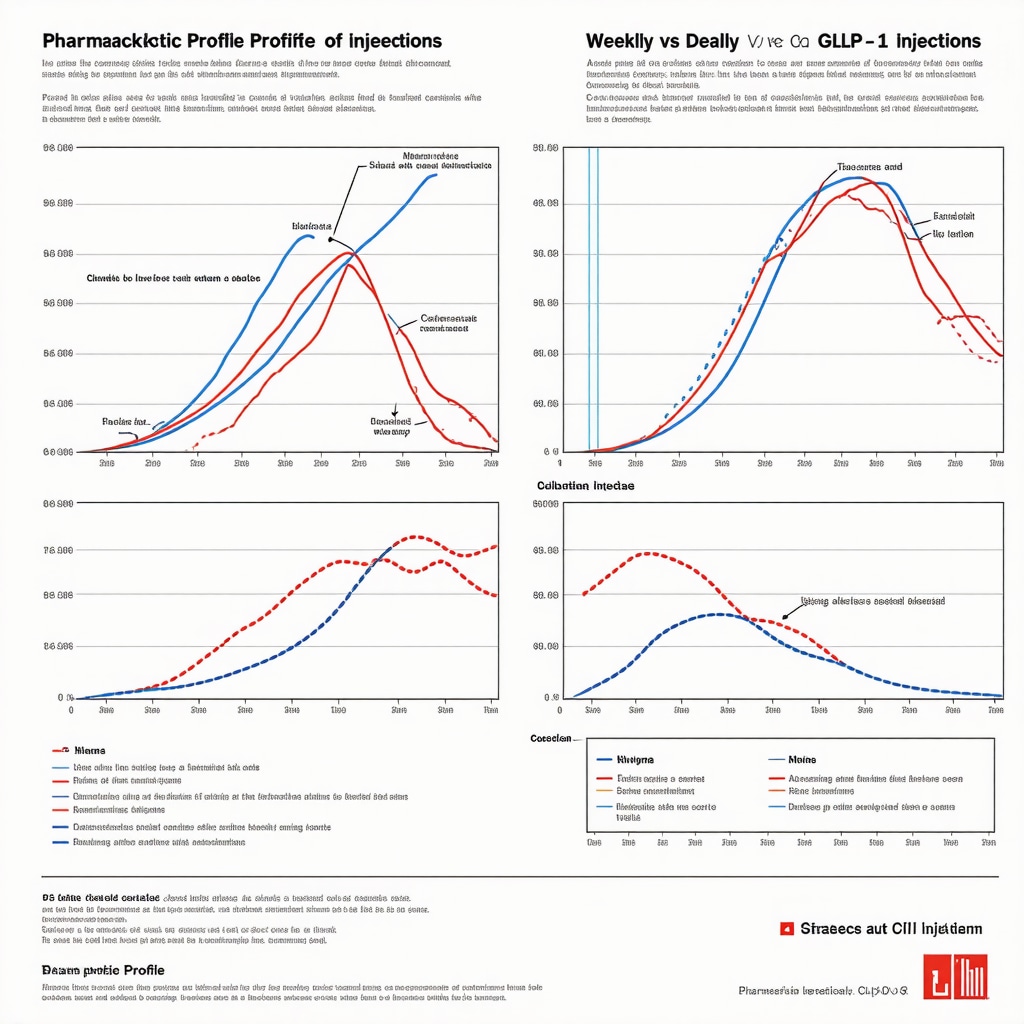
GLP-1 medications, such as semaglutide and tirzepatide, mimic the natural hormone GLP-1, which regulates appetite, insulin secretion, and gastric emptying. The frequency of injections—whether weekly or daily—can influence the drug’s plasma concentration stability, side effect profile, and ultimately, patient adherence. Weekly injections maintain steadier drug levels, reducing peaks and troughs that may cause nausea or other gastrointestinal symptoms, while daily injections might offer more flexibility but at the cost of increased injection burden.
How Does Injection Frequency Impact Long-Term Weight Loss Sustainability?
From clinical experience and trial data, weekly GLP-1 injections tend to enhance patient compliance due to convenience, which correlates with better sustained weight loss. For instance, a randomized controlled trial published in The New England Journal of Medicine demonstrated that once-weekly semaglutide resulted in significant, durable weight reduction compared to placebo over 68 weeks. This regimen minimized injection site reactions and gastrointestinal discomfort, common barriers to adherence with more frequent dosing.
Balancing Benefits and Risks: Tailoring Injection Schedules to Individual Needs
Practitioners must weigh the benefits of less frequent injections against individual patient lifestyle, tolerability, and medical comorbidities. Some patients may experience enhanced appetite suppression and metabolic improvements with weekly dosing, while others might require dosage adjustments or closer monitoring during initiation phases. Customizing injection schedules in a medically supervised setting can improve safety and efficacy, aligning with recommendations found in expert clinical guidance on semaglutide use.
Injecting Confidence: Practical Tips for Managing Injection Frequency Challenges
Adopting a consistent injection schedule is crucial, yet patients often encounter challenges such as injection site discomfort or forgetfulness. Techniques like proper site rotation, sterile injection practices, and setting reminders can mitigate these issues. Resources such as injection site rotation guides provide practical steps to enhance comfort and adherence, empowering patients throughout their weight loss journey.
Integrating Injection Frequency with Holistic Weight Loss Strategies
GLP-1 medication injections should complement, not replace, lifestyle modifications including balanced diet, regular physical activity, and behavioral changes. Synchronizing injection timing with mealtime and daily routines can optimize appetite control and glycemic regulation. For those on tirzepatide, for example, integrating exercise regimes with injection schedules has shown promising synergistic effects, as detailed in expert tips on combining medication with exercise.
What Are the Best Practices to Ensure Injection Frequency Maximizes Medication Benefits?
Experts recommend initiating GLP-1 therapy under medical supervision to tailor injection frequency based on individual response and side effect profile. Regular follow-ups allow dose titration and address potential barriers like injection anxiety or gastrointestinal symptoms. Patient education on the pharmacodynamics and expected timelines for weight loss fosters realistic expectations and sustained motivation.
If you’re navigating GLP-1 therapy, consider sharing your experiences or questions in the comments to help build a supportive community focused on effective weight management strategies.
Embracing Flexibility: How I Adapted My Injection Routine for Real Life
One of the biggest lessons I’ve learned during my GLP-1 journey is that injection frequency isn’t a rigid prescription—it’s more like a dynamic process that adapts with your lifestyle and body’s response. Early on, I was hesitant about weekly injections, fearing I’d forget or find it inconvenient. But as I synced my injection day with a weekly self-care routine, it became effortless. That said, I noticed that during particularly busy weeks or when traveling, having the option for a daily injection offered more control over side effects and timing.
This personal flexibility aligns with what many clinicians emphasize: tailoring your schedule rather than forcing a one-size-fits-all approach. For those curious about managing injection-related discomfort, I found that consulting resources like the doctor-approved tips for preventing injection site reactions was a game changer in easing soreness and swelling.
Listening to Your Body: Adjusting Injection Frequency When Side Effects Arise
It’s important to recognize that side effects such as nausea or fatigue might fluctuate with injection timing. In my experience, spacing out injections or adjusting the dose under medical supervision helped me find a balance between effectiveness and comfort. This careful adjustment process is backed by clinical observations; a review published in the National Institutes of Health database highlights how personalized dosing schedules optimize tolerability and adherence for GLP-1 therapies.
Moreover, maintaining open communication with your healthcare provider can ensure that your injection schedule evolves alongside your progress and lifestyle changes. This is why medically supervised plans, like those discussed in customizing injectable plans, are so vital.
Have You Ever Felt That Your Injection Schedule Could Be More Personalized?
Many of us focus on the medication itself but overlook how small tweaks in timing and frequency can transform the experience. I’d love to hear if you’ve found benefits in adjusting your injection routine or if you have questions about balancing frequency with side effects. Sharing these stories helps us all navigate this journey more confidently.
Integrating Mindfulness with Injection Frequency
Beyond the physical aspects, I found that pairing my injection routine with mindfulness practices significantly improved my overall well-being and motivation. For example, incorporating breathing exercises before injections helped reduce anxiety and made the process less daunting. This holistic approach is supported by emerging evidence suggesting that mindfulness can complement pharmacological treatments by reducing stress-induced eating behaviors.
If you’re interested, check out this resource on combining meditation with medication for practical ideas on weaving mindfulness into your routine.
Ultimately, the key takeaway for me has been that injection frequency is a tool—one that works best when adapted thoughtfully and paired with compassionate self-care.
Pharmacokinetic Nuances: Decoding the Impact of Injection Timing on GLP-1 Efficacy
The pharmacokinetics of GLP-1 receptor agonists are profoundly influenced by injection frequency, which dictates peak plasma levels, trough periods, and receptor engagement dynamics. Weekly formulations, such as semaglutide’s long-acting injectable, provide a sustained receptor activation profile, mitigating the oscillations in plasma concentration that can provoke adverse gastrointestinal effects. Conversely, daily injections may produce transient peaks that, while potentially intensifying appetite suppression, can also heighten side effect incidence.
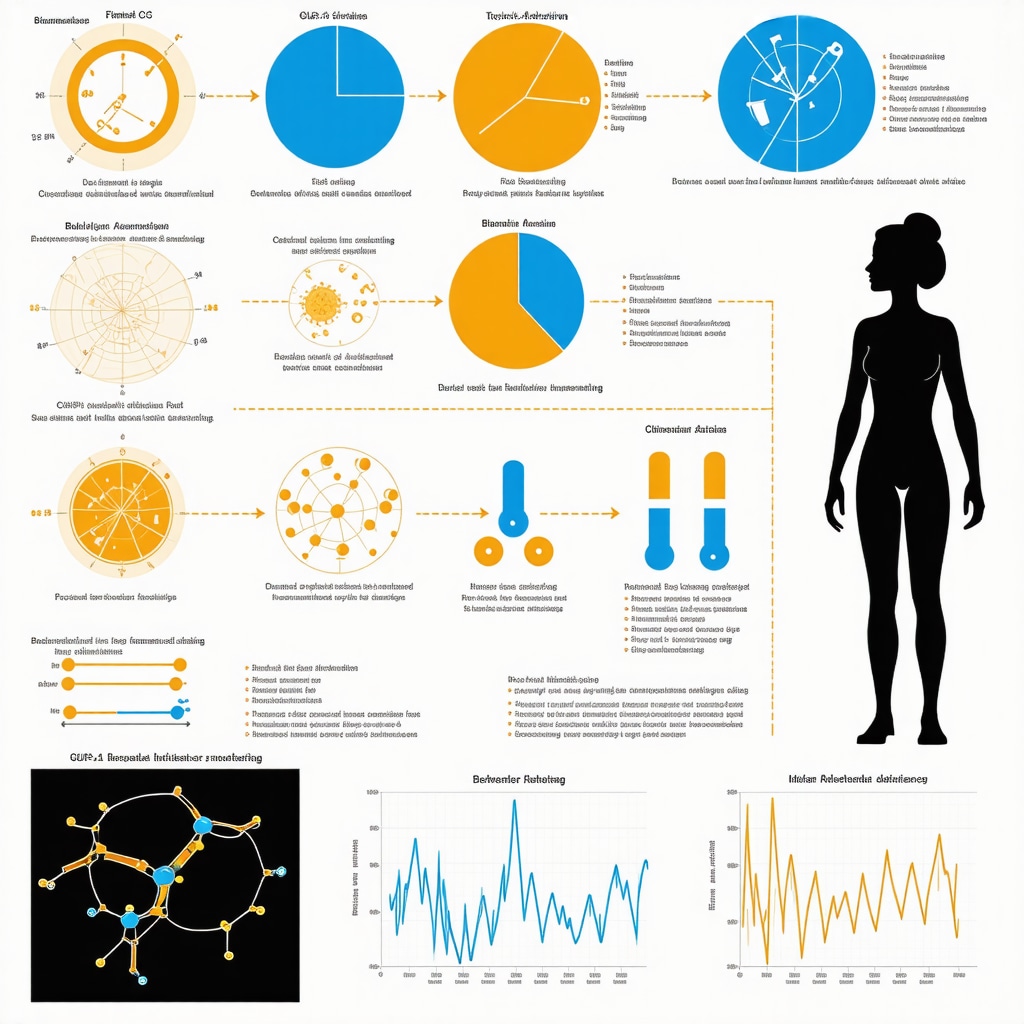
Recent pharmacodynamic modeling suggests that individualized timing—tailoring injection days to circadian rhythms and patient-specific metabolic patterns—can further optimize receptor responsiveness and weight loss outcomes. This approach underscores the importance of integrating chrono-pharmacology into GLP-1 therapy, an area ripe for clinical innovation.
Expert-Level Strategies: Personalizing Injection Frequency Through Biomarker Monitoring
Emerging evidence advocates for leveraging biomarkers such as fasting plasma glucose, HbA1c, and gut hormone profiles to refine injection schedules. By monitoring these parameters, clinicians can discern the patient’s metabolic response trajectory and adjust injection intervals accordingly to maximize efficacy while minimizing adverse events.
For example, patients exhibiting delayed gastric emptying or heightened sensitivity to GLP-1 may benefit from a lower frequency or dose titration, whereas others with suboptimal glycemic control might require more frequent administration or adjunctive therapies. These nuanced adjustments demand a multidisciplinary approach, involving endocrinologists, dietitians, and behavioral therapists to holistically support patient progress.
How Can Advanced Monitoring Improve GLP-1 Injection Frequency Decisions?
Advanced monitoring techniques, including continuous glucose monitoring (CGM) and pharmacogenomic testing, offer granular insight into individual responses to GLP-1 agonists. CGM data enable real-time assessment of glycemic variability and postprandial glucose excursions, which can inform optimal injection timing relative to meals. Pharmacogenomics may unveil genetic polymorphisms affecting drug metabolism and receptor sensitivity, paving the way for truly personalized injection regimens.
Incorporating these cutting-edge tools aligns with precision medicine principles and is supported by research published in the Journal of Clinical Endocrinology & Metabolism, which highlights the transformative potential of biomarker-guided GLP-1 therapies.
Optimizing Patient Adherence: Behavioral Economics Meets Injection Frequency
Adherence to injectable regimens remains a critical determinant of treatment success. Behavioral economics principles, such as nudges and habit formation techniques, can be strategically employed to enhance compliance with injection schedules. Tailoring reminders, simplifying injection devices, and integrating injections into pre-existing daily routines reduce cognitive load and improve consistency.
Furthermore, patient education emphasizing the physiological rationale behind injection timing fosters a sense of agency and motivation. The psychosocial dimension, including addressing injection anxiety and stigma, must also be considered, ensuring a comprehensive adherence strategy.
Synergizing GLP-1 Therapy with Nutritional Chronotherapy
Aligning GLP-1 injection timing with nutritional chronotherapy—synchronizing food intake with biological rhythms—can potentiate weight loss and metabolic benefits. Administering injections prior to meals timed during periods of heightened insulin sensitivity may amplify GLP-1’s anorectic and glycemic effects.
This innovative integration calls for meticulous patient education and lifestyle coaching, harnessing the interplay between circadian biology and pharmacotherapy to optimize outcomes.
If you are exploring advanced GLP-1 injection strategies or have insights on personalizing injection frequency, join the conversation below and deepen your understanding of cutting-edge weight management approaches.
Chrono-Pharmacology: Timing GLP-1 Injections to the Body’s Natural Rhythms
Recent advancements in chrono-pharmacology illuminate the intricate relationship between GLP-1 receptor agonist administration and the patient’s circadian biology. Understanding how injection timing aligns with endogenous metabolic cycles can potentiate both efficacy and tolerability. For example, administering weekly injections to coincide with periods of peak insulin sensitivity may enhance glucose regulation and appetite suppression without exacerbating side effects. This approach shifts the paradigm from a fixed schedule to a dynamic, biology-informed regimen, offering a new frontier in personalized weight management.
Incorporating Biomarker-Driven Personalization: A New Standard for Injection Scheduling
Leveraging biomarkers such as HbA1c levels, fasting plasma glucose, and gut hormone profiles provides a data-driven framework to tailor injection frequency and dosing. Such precision medicine strategies enable clinicians to identify patients who may benefit from altered dosing intervals or adjunct therapies. For instance, individuals exhibiting high GLP-1 sensitivity could require less frequent injections to maintain efficacy while minimizing gastrointestinal discomfort. Multidisciplinary collaboration between endocrinologists, dietitians, and behavioral specialists is fundamental to operationalizing these insights effectively.
How Can Real-Time Monitoring Technologies Revolutionize GLP-1 Injection Frequency Optimization?
Innovative tools like continuous glucose monitoring (CGM) and pharmacogenomic testing empower clinicians to customize GLP-1 injection schedules with unprecedented precision. CGM provides granular data on glycemic variability, enabling titration of injection timing to optimize postprandial glucose control. Meanwhile, pharmacogenomic profiles unravel individual differences in drug metabolism and receptor responsiveness. This fusion of technologies aligns with the precision medicine ethos, enhancing therapeutic outcomes and patient quality of life.
Authoritative research published in the Journal of Clinical Endocrinology & Metabolism underscores the transformative potential of biomarker-guided GLP-1 therapy in fostering tailored treatment plans.
Behavioral Economics Meets Injection Adherence: Strategies to Enhance Compliance
Optimizing injection frequency transcends pharmacology by incorporating behavioral science principles. Techniques such as habit stacking, nudges, and personalized reminder systems reduce cognitive burden and improve adherence to injection regimens. Simplifying injection devices and integrating injections into existing routines further promote consistency. Crucially, patient education that elucidates the physiological rationale behind timing regimens cultivates agency and mitigates injection-related anxiety, fostering a more sustainable therapy experience.
Synergistic Integration: Aligning Nutritional Chronotherapy with GLP-1 Regimens
Emerging evidence supports the strategic synchronization of GLP-1 injections with nutritional chronotherapy—timing meals and medication administration to the body’s biological clock. Administering injections prior to meals during periods of heightened insulin sensitivity can amplify anorectic effects and glycemic control. This holistic strategy demands detailed patient coaching and lifestyle modifications but offers a compelling avenue for maximizing therapeutic impact.
If you are exploring advanced GLP-1 injection strategies or have insights on personalizing injection frequency, join the conversation below and deepen your understanding of cutting-edge weight management approaches.
Frequently Asked Questions (FAQ)
What is the optimal frequency for GLP-1 injections to maximize weight loss?
The optimal injection frequency depends on the specific GLP-1 receptor agonist used, patient tolerance, and lifestyle factors. Weekly injections, especially with agents like semaglutide, have demonstrated superior adherence and sustained weight loss due to steadier plasma drug levels and fewer gastrointestinal side effects. However, some patients may benefit from daily dosing or personalized schedules based on clinical response and side effect profile.
How does injection frequency influence the side effect profile of GLP-1 medications?
Injection frequency affects plasma concentration fluctuations; weekly injections tend to produce more stable drug levels, reducing peak-related nausea and gastrointestinal discomfort. Daily injections may lead to transient higher peaks causing increased side effects but can offer greater flexibility in dosing adjustments during initiation or titration phases.
Can injection timing aligned with circadian rhythms improve GLP-1 therapy outcomes?
Yes, emerging chrono-pharmacology research suggests that synchronizing GLP-1 injections with periods of peak insulin sensitivity and metabolic activity can enhance appetite suppression and glycemic control while minimizing adverse effects. Tailoring injection timing to individual circadian biology represents a promising frontier in personalized weight management.
How can biomarkers guide the personalization of GLP-1 injection frequency?
Monitoring biomarkers such as HbA1c, fasting plasma glucose, and gut hormone profiles allows clinicians to assess metabolic response and adjust injection frequency and dosage accordingly. This biomarker-driven approach helps optimize efficacy, minimize side effects, and supports a multidisciplinary strategy involving endocrinologists and allied health professionals.
What role do continuous glucose monitoring (CGM) and pharmacogenomics play in injection scheduling?
CGM provides real-time data on glycemic patterns, aiding in precise injection timing relative to meals and glucose excursions. Pharmacogenomic testing can identify genetic factors influencing drug metabolism and receptor sensitivity, enabling customized dosing intervals. Together, these technologies support a precision medicine framework for GLP-1 therapy.
How can behavioral strategies improve adherence to GLP-1 injection regimens?
Incorporating behavioral economics principles such as habit stacking, nudges, personalized reminders, and simplifying injection processes can significantly enhance adherence. Patient education that clarifies the physiological rationale of injection timing fosters motivation and reduces anxiety, promoting consistent medication use.
Is it safe to adjust injection frequency without medical supervision?
No, adjusting GLP-1 injection frequency or dosage should always be done under medical supervision. Personalized adjustments require clinical assessment of metabolic response and side effects to ensure safety and treatment efficacy.
Can GLP-1 injections replace lifestyle modifications for weight management?
GLP-1 therapies are most effective when combined with holistic lifestyle changes, including balanced nutrition, regular physical activity, and behavioral interventions. Medications complement but do not substitute these foundational strategies.
How does injection site rotation affect treatment outcomes and comfort?
Proper injection site rotation minimizes local skin reactions, reduces discomfort, and supports consistent medication absorption. Adhering to sterile techniques and rotating injection sites are essential best practices to enhance patient comfort and adherence.
What are the emerging trends in GLP-1 injection personalization?
Advancements include chrono-pharmacology-based timing, biomarker-guided dosing, integration of real-time monitoring technologies, and behavioral economics-informed adherence strategies. These innovations aim to tailor therapy dynamically to individual patient biology and lifestyle for optimized outcomes.
Trusted External Sources
- The New England Journal of Medicine (NEJM): Provides high-quality randomized controlled trial data on GLP-1 receptor agonists, offering evidence-based insights into efficacy and safety profiles crucial for understanding injection frequency effects.
- Journal of Clinical Endocrinology & Metabolism (JCEM): Publishes research on endocrine therapies, including biomarker and pharmacogenomic studies pivotal for personalizing GLP-1 injection schedules.
- National Institutes of Health (NIH) PubMed Central: Offers comprehensive reviews and clinical trial data on GLP-1 receptor agonists, supporting evidence-based recommendations for injection frequency and management of side effects.
- American Diabetes Association (ADA): Provides clinical practice guidelines and expert consensus on injectable therapies, including GLP-1 receptor agonists, informing best practices for injection timing and patient adherence.
- Endocrine Society: A leading authority on hormonal therapies, delivering consensus statements and research updates on GLP-1 pharmacology and personalized treatment strategies.
Conclusion
Optimizing GLP-1 injection frequency is a multifaceted endeavor that integrates pharmacokinetic principles, patient lifestyle, biomarker insights, and behavioral science to maximize weight loss efficacy and minimize adverse effects. Weekly injections generally provide a favorable balance of convenience and stable drug exposure, yet personalization through chrono-pharmacology and advanced monitoring technologies heralds a new era of tailored therapy. Coupling GLP-1 regimens with holistic lifestyle modifications and mindful practices further enhances therapeutic outcomes. As research and technology evolve, embracing a dynamic, patient-centered injection schedule will empower individuals and clinicians to navigate weight management more effectively. Engage with this knowledge by sharing your experiences, asking questions, or exploring related expert content to deepen your understanding and optimize your weight loss journey.

I’ve been using a GLP-1 receptor agonist for weight management, and the discussion about injection frequency really resonates with my experience. Initially, the idea of weekly injections felt daunting due to the anxiety around remembering the exact day, but aligning it with a consistent weekly routine, as the article suggests, made a significant difference in my adherence. What I found particularly interesting is how some patients might need to tailor their injection schedules based on side effects like nausea, which can fluctuate and require dose adjustments under medical supervision. This personalized approach, factoring in lifestyle and tolerability, seems crucial for sustainable success. Additionally, pairing injections with lifestyle modifications and mindful practices has enriched my journey, improving both physical and mental well-being. I’m curious, for others who have navigated this treatment, how flexible have you found your injection schedules? Have you incorporated strategies like site rotation or mindfulness to manage side effects effectively? Sharing these insights could really benefit those starting out or seeking to improve their regimen.
This post really emphasizes the importance of personalized approaches in GLP-1 therapy, especially regarding injection frequency. I’ve noticed that for some people, weekly injections provide excellent convenience and adherence, but others might prefer a bit more flexibility, especially during travel or busy periods. I remember initially struggling with the routine but syncing injections with weekly self-care activities made a big difference for me. I’m curious—how have others managed to balance consistency with life’s unpredictability? Do you think advances in biomarker monitoring or real-time data could help tailor injection schedules more dynamically? The idea of aligning injections with circadian rhythms is fascinating, as it could potentially enhance both efficacy and tolerability. Would love to hear from those experimenting with timing adjustments or combining pharmacotherapy with lifestyle strategies like meal timing or mindfulness practices. It seems that the future of GLP-1 treatment will be increasingly personalized, which is encouraging for sustained success in weight management.
This article really highlights how crucial personalized treatment plans are when it comes to GLP-1 injections. I’ve personally found that sticking to a weekly schedule works best for my routine, but I’ve also had to adapt during busy weeks or travel. The tip about site rotation really resonated with me, as I’ve experienced some discomfort from not varying injection sites. It’s fascinating how aligning injection timing with circadian rhythms might optimize outcomes—something I haven’t explored much yet. Has anyone tried adjusting their injection time to match their daily energy patterns or meal schedule? I’m curious whether this kind of chrono-tailoring could make a difference in side effects or effectiveness over the long term. It seems that leveraging biomarker monitoring and tech tools like CGM could really personalize the approach further, but I wonder how accessible these options are for most patients. Overall, this comprehensive view makes me feel more confident about customizing my regimen safely. Would love to hear others’ thoughts on balancing consistency with flexibility—what strategies have worked best for you?